Learning objectives
- Definition of a renal transplant
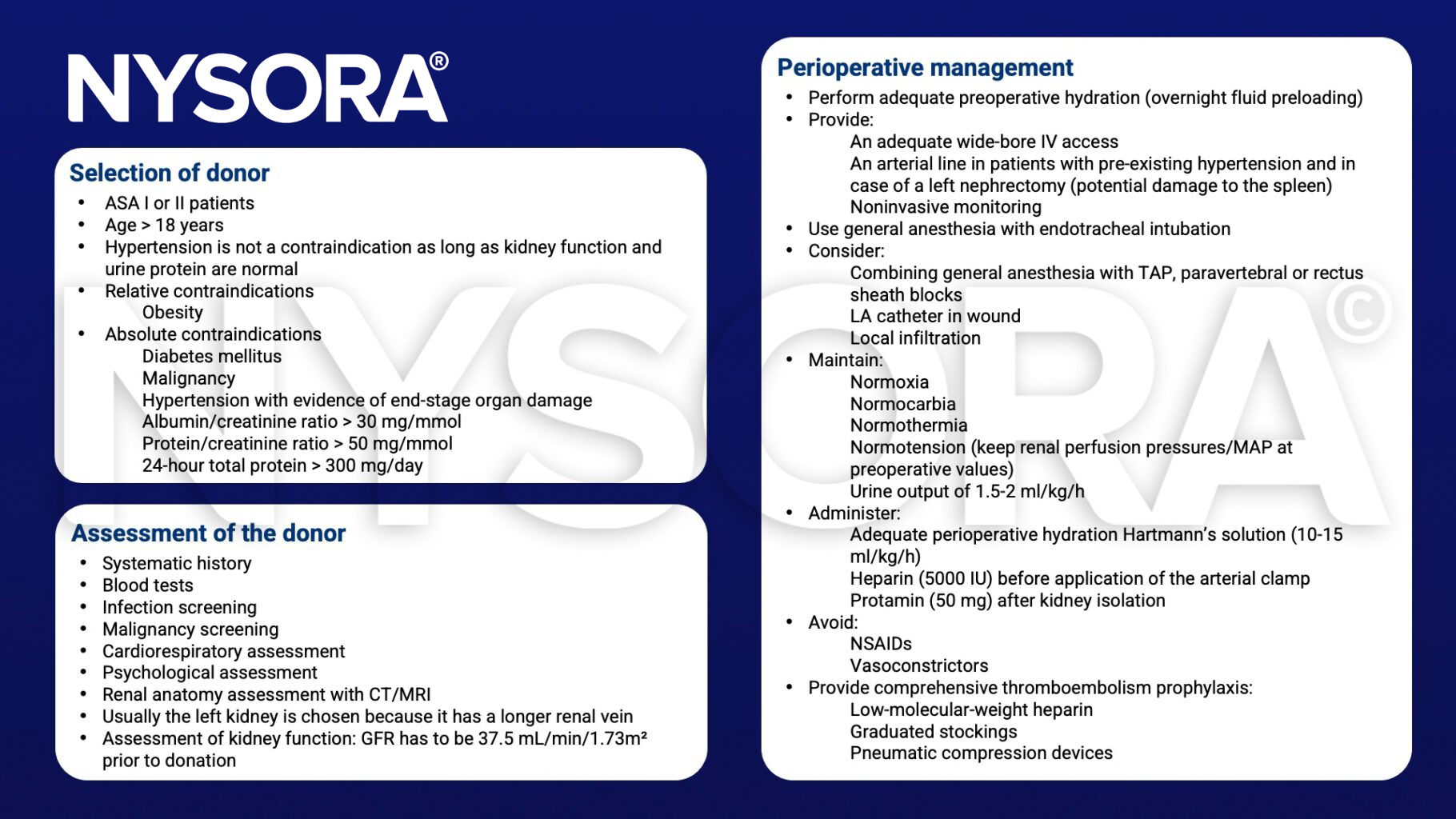
- Management of a living donor during a nephrectomy
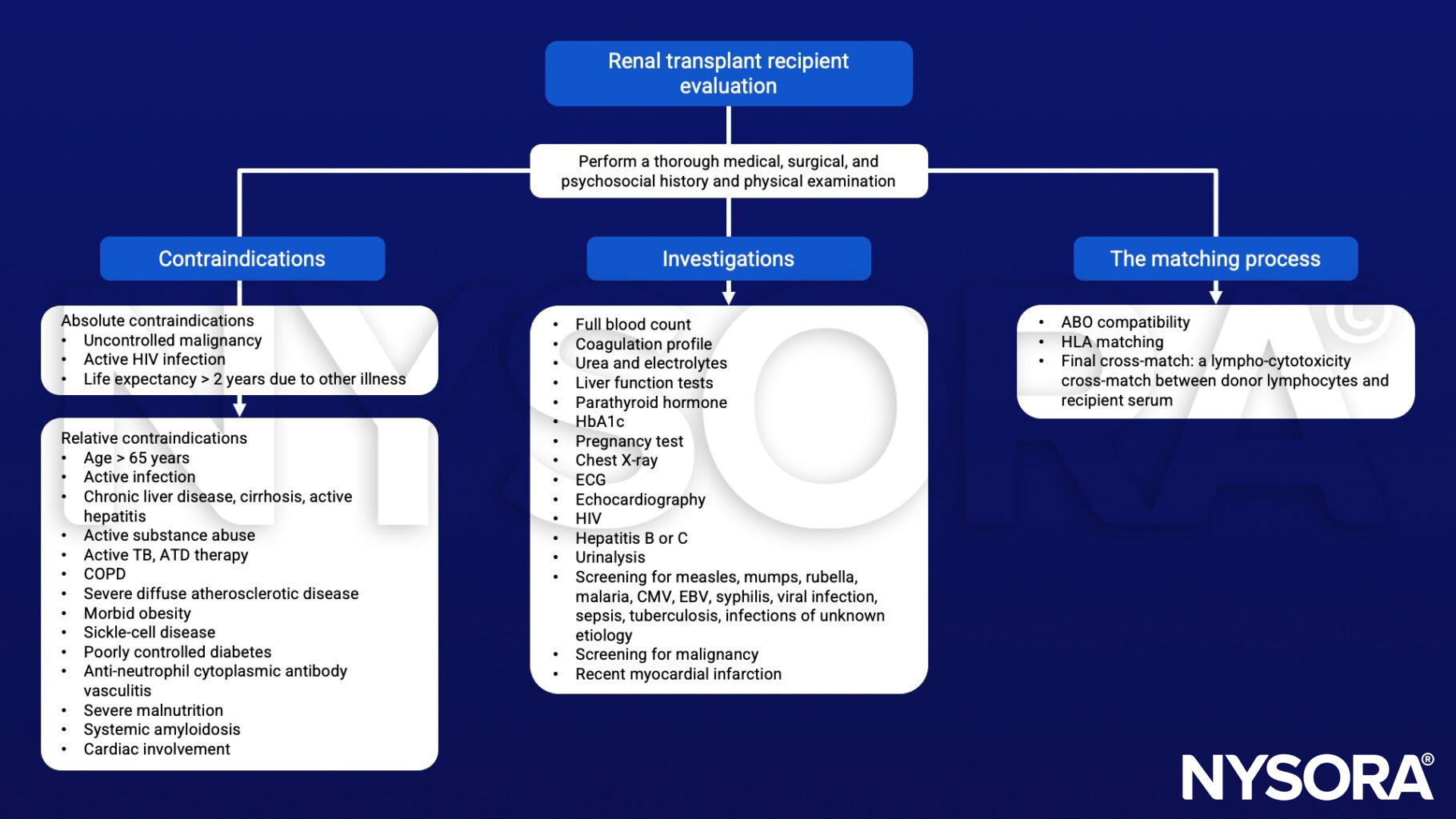
- Management of a renal transplant recipient
Definition and mechanisms
- A renal transplant is the organ transplant of a kidney into a patient with end-stage kidney disease (ESRD)
- Classified as deceased-donor (formerly known as cadaveric) or living-donor nephrectomy (LDN)
- Improves both length and quality of life for patients with end-stage renal disease (ESRD)
- ESRD is defined as chronic kidney disease (CKD) with a glomerular filtration rate (GFR) <15 mL/min/1.73 m² or where renal replacement therapy is needed
- Diabetes is the most common cause of ESRD followed by glomerulonephritis, polycystic kidney disease, pyelonephritis, hypertension, and auto-immune disorders
- Two-year graft survival is > 80% for cadaveric and 90% for living-donor grafts and overall patient survival is > 95%
Signs and symptoms
Complications
- Bleeding
- Vascular thrombosis and stenosis
- Transplant rejection (hyperacute, acute, or chronic)
- Ureteral obstruction
- Urinary leakage
- Infections and sepsis due to immunosuppression
- Post-transplant lymphoproliferative disorder
- Electrolyte imbalance (particularly calcium and phosphate)
- Proteinuria
- Hypertension
Management of the living donor during nephrectomy
Postoperative care of the living donor
- Provide postoperative analgesia via a fentanyl PCA
- Consider a paravertebral or TAP block to complement analgesia
- Avoid NSAIDs
- Apply early mobilization along with breathing exercises and incentive spirometry
- Consider postoperative complications:
- Pulmonary embolism
- Hepatitis
- Myocardial infarction
- Arrhythmias
- Pneumonia
- Atelectasis
- Urinary tract infection
- Wound infections
- Splenic lacerations
Management of the recipient


Suggested reading
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Mayhew D, Ridgway d, Hunter JM. 2016. Update on the intraoperative management of adult cadaveric renal transplantation. BJA education. 16;2:53-57.
- O’Brien, B., Koertzen, M., 2012. Anaesthesia for living donor renal transplant nephrectomy. Continuing Education in Anaesthesia Critical Care & Pain 12, 317–321.
- Rabey P. 2001. Anesthesia for renal transplantation. BJA CEPD Reviews. 1;1:24-17.
Clinical updates
Kim et al. (RAPM, 2024) report in a double-blinded randomized controlled trial of 88 living-donor renal transplant recipients that a unilateral anterior quadratus lumborum (QL) block did not reduce 24-hour postoperative opioid consumption or pain scores compared with a sham block when used within a multimodal analgesia regimen. Secondary outcomes were also similar between groups, suggesting routine use of the anterior QL block is not supported for analgesia after renal transplantation.
- Read more about this study HERE.
Hofer et al. (2025, A&A) report that preoperative intrathecal hydromorphone (median 100 µg) in kidney transplant recipients is associated with a 66% reduction in 72-hour postoperative opioid consumption and significantly lower pain scores at 24 and 72 hours, without increasing respiratory depression, naloxone use, or length of stay. The main trade-off was a higher incidence of postoperative nausea and vomiting, underscoring the need for proactive antiemetic prophylaxis. These findings support intrathecal opioids as a safe, opioid-sparing adjunct within evolving ERAS-style pathways for renal transplantation.
- Read more about this study HERE.









