Learning objectives
- Describe the causes and risk factors for corneal abrasion
- Prevent corneal abrasion
- Manage corneal abrasion occurrence
Background
- Corneal abrasion is the most common ophthalmologic complication in patients undergoing general anesthesia for nonocular surgery
- Can result in eye pain or soreness in response to bright light
- May develop into inflammation or ulcers by infection of bacteria or fungi on the scar
- Postoperative pain can be more severe than
Causes
| Mechanical injury | Direct contact with drapes, masks, or other equipment/items |
| Inadvertent pressure on the eyeball | |
| Loss of pain perception and inhibition of protective corneal reflexes further increase risk | |
| Chemical injury | Spillage of antimicrobial solutions into the eyes during skin preparation |
| Contact with cleaning solutions retained on the anesthetic mask | |
| Ocular hypersensitivity to inhaled anesthetic agents (e.g., halothane) | |
| Antiseptic solutions containing detergents or alcohol | |
| Exposure keratopathy | Sedatives and neuromuscular blocking agents inhibit active contraction of the orbicularis oculi muscle, resulting in incomplete eyelid closure, corneal exposure, and dryness |
| Correlated with the duration of corneal exposure | |
| Reduced tear production | General anesthesia suppresses the autonomic nerve supply to the lacrimal gland |
| Specific drugs (e.g., beta-blockers, hydrochlorothiazide) inhibit tear production | |
| Ocular hypoperfusion secondary to deliberate hypotension | |
| Anesthetic gases delivered via face mask add to corneal dehydration | |
| General anesthesia inhibits the blink reflex and redistribution of tears over the ocular surface | |
| Bell’s phenomenon (upward rotation of the eyeball to protect the cornea during sleep) is absent during anesthesia |
Risk factors
- General anesthesia
- Lower ASA status
- History of dry eyes
- Advanced age
- Proptosis or exorbitism
- History of corneal trauma
- Longer procedures
- Preoperative anemia
- Prone, lateral or Trendelenburg position
- Procedures near head/neck
- Intraoperative hypotension
Prevention
- Eyelid taping immediately after induction (preferred method)
- Ocular lubricants (fat-based ointments are retained longer than aqueous solutions but pose a higher risk of complications)
- Hydrogel dressings
- Bio-occlusive dressings
- Continuous perioperative eye monitoring
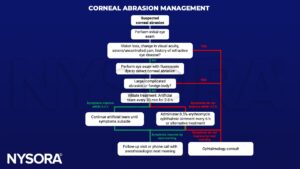
Management
Suggested reading
- Hewson DW, Hardman JG. Physical injuries during anaesthesia. BJA Educ. 2018;18(10):310-316.
- Malafa MM, Coleman JE, Bowman RW, Rohrich RJ. Perioperative Corneal Abrasion: Updated Guidelines for Prevention and Management. Plast Reconstr Surg. 2016 May;137(5):790e-798e.
- Lichter JR, Marr LB, Schilling DE, et al. A Department-of-Anesthesiology-based management protocol for perioperative corneal abrasions. Clin Ophthalmol. 2015;9:1689-1695. Published 2015 Sep 11
- Grixti A, Sadri M, Watts MT. Corneal protection during general anesthesia for nonocular surgery. Ocul Surf. 2013;11(2):109-118.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com