Learning objectives
- Describe cleft lip and palate
- Summarize the anticipated complications during the intraoperative and postoperative period among patients with cleft lip and palate
- Discuss the perioperative management of patients with orofacial clefts
Definition and mechanisms
- Orofacial clefts, encompassing cleft lip with or without cleft palate and cleft palate alone, are the most common craniofacial abnormalities
- They are birth defects and result from tissues of the face not joining properly during development
- These disorders affect the patient’s feeding, speech, hearing, dental health, appearance, and psychological health
- Cleft lip: Fissure in the upper lip and may be incomplete or complete (through to the nasal cavity), unilateral, or bilateral
- Cleft palate: Gap in the soft palate that may or may not involve the hard palate, submucous (mildest form), incomplete or complete, unilateral or bilateral
Common syndromes associated with cleft lip and palate
| Chromosomal syndromes | Features |
|---|---|
| Velocardiofacial (DiGeorge) syndrome | Microcephaly and microstomia Flat nasal bridge, small ears, short stature Immune deficiency, congenital cardiac disease Velopharyngeal incompetence with or without cleft palate Laryngeal and tracheal anomalies 22q11 deletion (FISH test) Cleft palate in 30% of cases |
| Trisomy 21 (Down's syndrome) | Microstomia and relative macroglossia Epicanthic folds, simian crease Congenital cardiac disease Atlantoaxial subluxation and instability |
| Monogenic syndromes | |
| Van der Woude syndrome | Lower lip pits Hypodontia Congenital cardiac disease Musculoskeletal issues Most common orofacial clefting syndrome |
| Treacher-Collins syndrome | Micrognathia and maxillary hypoplasia Choanal atresia Eye and ear malformations Intubation may become more difficult with age Cleft palate in 30% of cases |
| Hemifacial microsomia (Goldenhar syndrome) | Hemifacial and mandibular hypoplasia Cervical spine abnormalities Ear and eye abnormalities Intubation may become more difficult with age |
| Stickler syndrome | Progressive connective tissue disorder (autosomal dominant) Midface hypoplasia Micrognathia/PRS Retinal detachment and early cataracts Deafness Hypermobility of joints |
| Sequence | |
| Pierre-Robin sequence (PRS) | Micrognathia Glossoptosis Underlying syndrome/anomalies Usually easier to intubate with age Cleft palate in 80% of cases |
Signs and symptoms
- Opening in the upper lip that may extend into the nose or palate
Cleft lip
- Cleft does not affect the palate structure of the mouth
- Partial or incomplete cleft lip: Formed in the top of the lip as a small gap or indentation of the lip
- Complete cleft lip: Cleft continues into the nose
- Can occur as a one-sided (unilateral) or two-sided (bilateral) condition
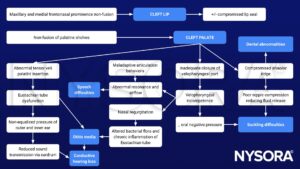
- Due to failure of the fusion of the maxillary prominence and medial nasal processes (formation of the primary palate)
Cleft palate
- The two plates of the skull that form the roof of the mouth are not completely joined
- Cleft lip is also present in most cases
- Complete cleft palate: Soft and hard palate, possibly including a gap in the mandible
- Incomplete cleft palate: A hole in the roof of the mouth, usually as a cleft soft palate
- Submucous cleft palate: Mildest form with no visible cleft but a failure of the palatal muscles to unite
- The uvula is usually split
- Due to failure of the fusion of the lateral palatine processes, nasal septum, or median palatine processes (formation of the secondary palate)
- The hole in the roof of the mouth connects the mouth directly to the inside of the nose, resulting in velopharyngeal insufficiency (VPI) → hypernasal speech, nasal emission, and nasal turbulence
Causes
- Most clefts are polygenic and multifactorial in origin with many genetic and environmental factors contributing
- Genetic factors cause clefts in 20% to 50% of the cases
- The remaining clefts are attributable to either environmental factors (e.g., teratogens) or gene-environment interactions
Complications
- Feeding problems
- Speech problems
- Hearing problems
- Frequent ear infections
Risk factors
- Smoking during pregnancy
- Diabetes
- Obesity
- Older mother
- Certain medications (i.e., some used to treat seizures)
Pathophysiology
Treatment
- Speech therapy: Improve velopharyngeal function and develop normal speech without compensatory articulations
- Dental care
- Corrective surgery
- Cleft lip: 8-12 weeks
- Cleft palate: 6-12 months (dependent upon the size of the cleft)
Management
Considerations for anesthesia for cleft lip and palate surgery
| Patient-related factors | Usually infants or young pediatric patient Associated comorbidities and syndromes Nutritional status Airway obstruction Potential difficult airway |
| Anesthetic factors | General anesthesia with tracheal tube Shared airway |
| Surgical factors | Elective surgery (time to optimize) |
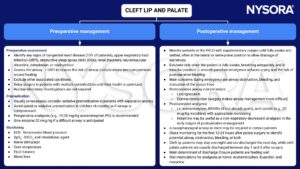

Keep in mind
- Orofacial clefts are the most common craniofacial abnormality and patients with clefts require specialized multidisciplinary care from infancy through adulthood
- Assess patients appropriately in the preoperative period as cleft anomalies are associated with numerous congenital abnormalities
- Management of the airway may be challenging because of a difficult, shared airway, and postoperative airway obstruction
- Monitor patients for signs of airway obstruction throughout their recovery from anesthesia
- A multimodal approach to analgesia is important to provide optimal conditions for recovery
Suggested reading
- Denning S, Ng E, Wong Riff KWY. Anaesthesia for cleft lip and palate surgery. BJA Education. 2021; 21(10): 384-389.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com