Learning objectives
- Diagnose and treat carbon monoxide (CO) poisoning
Definition and mechanisms
- Carbon monoxide is a colorless, odorless, tasteless gas produced by burning gasoline, wood, propane, charcoal, or other fuel
- volatile anesthetics can produce CO when used with CO2 absorbents
- CO intoxication causes tissue hypoxia in three ways:
- CO binds with hemoglobin with about 250 times the affinity of oxygen, therefore, preventing oxygen binding
- CO also leads to a shift in the oxygen dissociation curve to the left impending delivery
- CO competitively inhibits the binding of oxygen with cytochrome oxidase, a key mitochondrial enzyme, significantly impairing cellular utilization of oxygen
- Mortality is 1-3%
Signs and symptoms
| Acute poisoning | |
| Central nervous system | Headache Dizziness Confusion Altered mental status Incoordination Ataxia Seizures Coma |
| Cardiovascular system | Dysrhythmias Ischemia Hypertension Hypotension |
| Gastrointestinal tract | Abdominal pain Nausea Vomitting Diarrhea |
| Respiratory system | Dyspnea Tachypnea Chest pain Palpitation |
| Other | Non-cardiogenic pulmonary edema Lactic acidosis Rhabdomyolysis Hyperglycemia Disseminated Intravascular Coagulation (DIC) Bullae Alopecia Sweat gland necrosis |
| Chronic exposure | |
| May have similar effects to acute poisoning, but often with a gradual, insidious onset, and symptoms may fluctuate with varying levels of exposure to CO over time | Headache Personality changes Poor concentration Dementia Psychosis Parkinson’s disease Ataxia Peripheral neuropathy Hearing loss |
Complications
- Chronic fatigue
- Permanent brain damage
- Damage to your heart, possibly leading to life-threatening cardiac complications
- Fetal death or miscarriage
- Death
Diagnosis
- Standard SpO2 does not identify CO poisoning
- HbCO level of more than 3% among nonsmokers and more than 10% among smokers
- ECG indication of ischemia
- Clinically significant acidosis
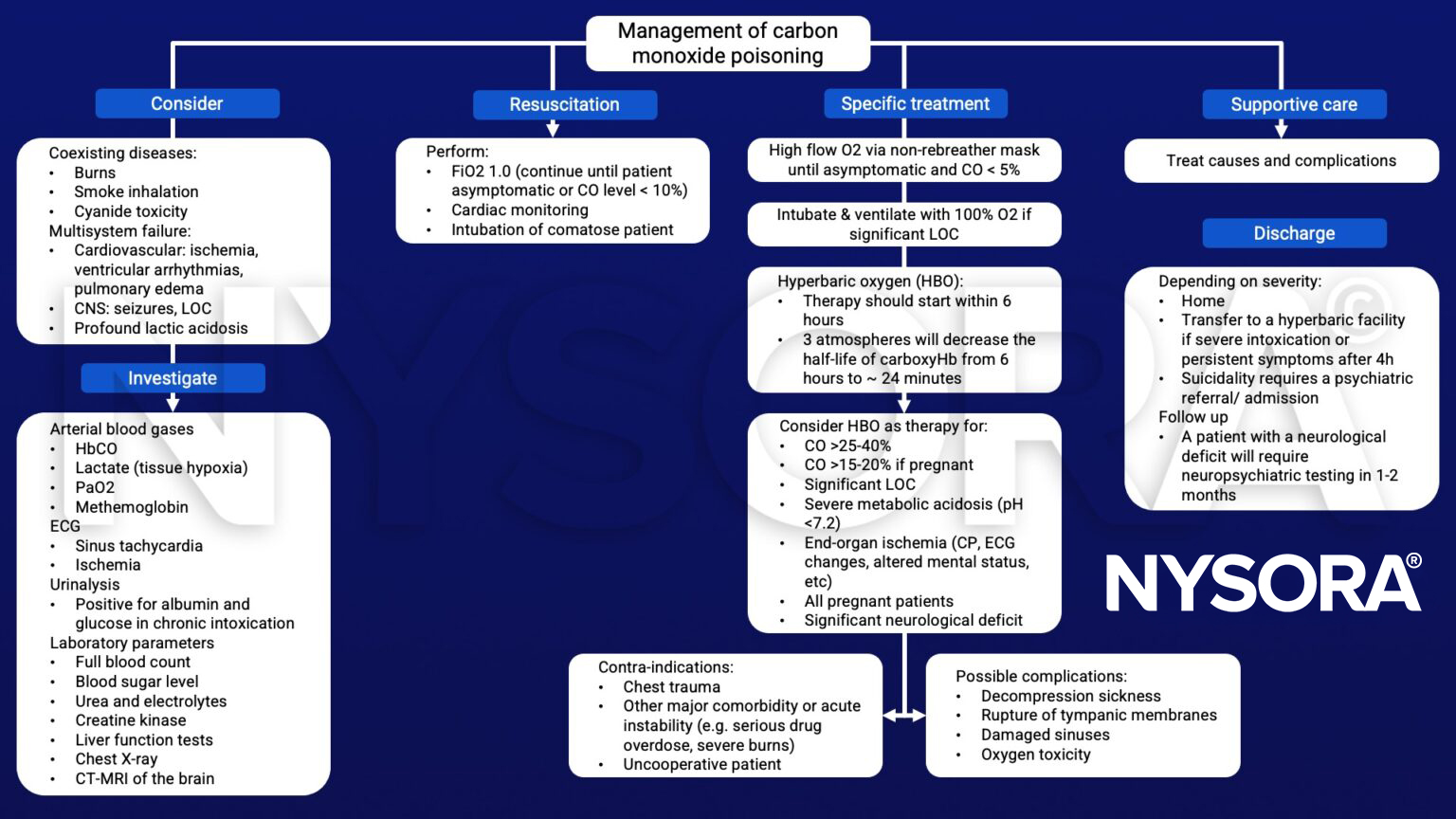
Management
Suggested reading
- Chenoweth JA, Albertson TE, Greer MR. Carbon Monoxide Poisoning. Crit Care Clin. 2021;37(3):657-672.
- Horncastle, E., Lumb, A.B., 2019. Hyperoxia in anaesthesia and intensive care. BJA Education 19, 176–182.
- Gill, P., Martin, R.V., 2015. Smoke inhalation injury. BJA Education 15, 143–148.
Clinical updates
Savioli et al. (Journal of Clinical Medicine, 2024) provide an updated pathophysiological framework for carbon monoxide poisoning, emphasizing that toxicity is not solely due to carboxyhemoglobin formation but also to direct cellular injury via mitochondrial cytochrome c oxidase inhibition, oxidative stress, inflammatory activation, and disruption of the hypothalamic–pituitary axis. The review highlights that COHb levels correlate poorly with clinical severity (except at > 40–50%) and that delayed neurological syndrome (occurring in up to 1–47% of cases, sometimes within 40 days) represents a major long-term complication. The authors stress early blood gas analysis in the ED, careful differential diagnosis in neurologic and cardiac presentations, structured follow-up for late sequelae, and individualized selection between normobaric and hyperbaric oxygen therapy .
- Read more about this study HERE.









