Learning objectives
- Describe the clinical presentation of Parkinson’s disease
- Diagnose and treat Parkinson’s disease
- Manage Parkinson’s disease patients presenting for surgery
Background
- Parkinson’s disease (PD) is an idiopathic neurodegenerative disorder, characterized by bradykinesia, muscle rigidity, and asymmetric resting tremor
- Most common movement disorder (~1% prevalence in the population >65 years of age)
- Loss of dopaminergic neurons in the pars compacta region of the substantia nigra
Etiology
- The etiology of PD is unknown but may be induced by genetic, environmental, or infectious factors
- Increasing age is the most consistent risk factor
Signs & symptoms
Clinical features Timing
Primary motor features Resting tremor (usually asymmetrical) Usually at diagnosis
Bradykinesia
Rigidity
Early non-motor features Fatigue May precede diagnosis
Depression/anxiety
Sleep disturbance
Constipation
Later features Gait change: Stooped posture, shuffling gait with small steps, loss of arm-swing 5–10 years after onset of symptoms
Dysphagia
Expressionless face
Small handwriting
Soft speech
Postural instability
Cognitive disturbance, slowed cognitive speed, inattention, poor problem solving Increasing likelihood as time from diagnosis increases
Dementia >80% at 20 years after diagnosis
Autonomic Postural hypotension 5-10 years after onset of symptoms
Sialorrhea
Urinary dysfunction
Sexual dysfunction
Diagnosis
- There are no specific diagnostic tests for PD
- Clinical diagnosis based on the hallmark symptoms (tremor at rest, muscle rigidity, bradykinesia)
Treatment
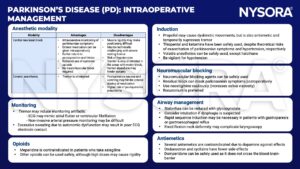
- Treatment is symptomatic and usually pharmacological
| Medications | Indication | Side-effects | Anesthetic implications | |
|---|---|---|---|---|
| Dopamine agonists | Pramipexole, ropinirole | Monotherapy in early and established PD, adjunct to levodopa-DDI regime | Nausea, orthostatic hypotension, impulsive control disorders, somnolence | Risk of dopamine agonist withdrawal syndrome on acute withdrawal |
| Rotigotine | ‘Bridging’ therapy in patients who are unable to take or absorb antiparkinsonian medication, adjuncts to levodopa-DDI regime | Nausea, orthostatic hypotension, impulsive control disorders, somnolence | Parenteral transdermal preparation | |
| Apomorphine | ‘Bridging’ therapy in patients who are unable to take or absorb antiparkinsonian medication, adjuncts to levodopa-DDI regime | Nausea, dyskinesias, cognitive impairment, postural instability | Subcutaneous infusion or injectable ‘pen’ for patients with troubling motor fluctuations, very emetogenic, risk of severe hypotension | |
| Dopamine precursors with peripherally acting dopa decarboxylase inhibitor (DDI) | Levodopa-carbidopa, levodopa-benserazide | Motor symptoms in established PD | Nausea, orthostatic hypotension, dyskinesia, hallucinations | Risk of parkinsonism-hyperpyrexia syndrome on acute withdrawal; short halflife (1.5 h) - need to continue enteral administration in prolonged procedures |
| Monoamine oxidase B inhibitors | Selegiline, rasagiline | Used as monotherapy in early PD, or as adjunct to levodopa-DDI regime | Headache, arthralgia, exacerbation of levodopa side-effects when used as adjunct | Risk of serotonin syndrome (fever, hypertension, tachycardia, agitation) with meperidine |
| Catechol-O-methyl transferase inhibitors (COMTIs) | Entacapone, Tolcapone | Adjunct to levodopa-DDI regime | Dark-colored urine, exacerbation of levodopa side-effects | Reduce dose of other drugs metabolized by COMT pathways, e.g., epinephrine |
- Abrupt withdrawal of medications can result in withdrawal complications:
- Parkinsonism-hyperpyrexia syndrome
- Due to withdrawal of levodopa
- Symptoms: Muscle rigidity, fever, cardiovascular instability, altered mental status (agitation, delirium, coma).
- Significant mortality, up to 20% in untreated cases
- dopamine agonist withdrawal syndrome (DAWS)
- Symptoms: Anxiety, nausea, depression, pain, orthostatic hypotension
- Withdrawal of dopamine agonists should be planned electively and simultaneously replaced with levodopa therapy
- Parkinsonism-hyperpyrexia syndrome
Anesthetic management
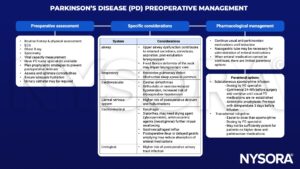
- Preoperative
- Intraoperative
- Postoperative
- Consider ICU admission
- Assess the feasibility of enteral anti-parkinsonian medication
- Adequate analgesia, tremor, and rigidity may hinder patient-controlled analgesia
- Postoperative delirium: Non-pharmacological management is preferred, avoid haloperidol, benzodiazepines are safer
- Physiotherapy facilitates early mobilization
Suggested reading
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Chambers DJ, Sebastian J, Ahearn DJ. Parkinson’s disease. BJA Education. 2017;17(4):145-9.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com