Learning objectives
- Describe the indications and contraindications for blind nasal intubation
- Describe the technique for blind nasal intubation
- Describe the possible repositioning actions and complications of blind nasal intubation
Background
- Blind nasal intubation was originally used in spontaneously breathing patients anesthetized with an inhalational agent, but has been modified for intubating awake patients, with or without sedation
- Useful technique for patients with a difficult airway
- Has been largely replaced by fiber-optic intubation, but remains a relevant and easy alternative when a fiber-optic scope is not available or fiber-optic intubation has failed
- Indicated when there are structural abnormalities in the mouth or limited mouth opening
Indications & contraindications
- Indications
- Known difficult intubation or previous nasal intubation
- Anticipated difficult intubation
- After failed intubation in an unanticipated difficult airway
- Known or suspected difficult mask ventilation
- Unstable C-spine
- Contraindications
- Absolute
- Patient refusal or inability to cooperate
- Relative
- Lack of trained personnel
- Risk of impending airway obstruction
- Coagulopathy or bleeding in airway
- Allergy to local anesthetic
- Base of skull fracture
- Absolute
Technique
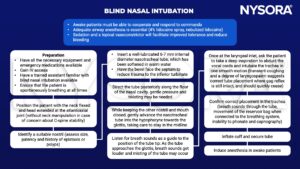
- Clinical findings for tube repositioning to facilitate successful intubation:
| Position | Clinical findings | Action |
|---|---|---|
| Trachea | Breath sounds through tube maintained as it is advanced, coughing through tube | Confirm ETCO2, bilateral air entry |
| Anterior | Breath sounds heard through tube but unable to advance further, bulge felt anteriorly at level of hyoid, coughing mostly through tube | Withdraw tube 2 cm, reduce neck extension or externally manipulate larynx before readvancing |
| Left/right piriform fossa | No breath sounds, unable to advance tube, no coughing, a bulge may be seen or palpated superio- lateral to larynx | Withdraw tube until breath sounds return, rotate tube to midline or turn head towards bulge and readvance |
| Esophagus | Tube advances smoothly with loss of breath sounds, no cough, larynx elevated | Withdraw tube until breath sounds return and try the following maneuvers before readvancing: • Head extension • Cricoid pressure • Inflate cuff with 15 mL of air to direct the tip anteriorly. Advance until resistance met, ensure breath sounds retained (at laryngeal inlet), slowly deflate cuff while maintaining some advancing pressure on tube to enter trachea |
Complications
- General complications:
- Oversedation
- Respiratory depression
- Airway obstruction
- Apnea
- Trauma
- Bleeding
- Laryngospasm
- Vomiting
- Local anesthetic allergy
- Toxicity
- Risk of aspiration due to loss of laryngeal reflexes
- Specific complications related to nasal route
- Epistaxis
- Turbinate or polyp fracture
- Retropharyngeal laceration
- Retropharyngeal abscess and mediastinitis
- Intracranial placement in basal skull fracture and pneumocephalus
- Specific complications related to blind technique:
- Airway trauma from multiple intubation attempts
- Obstruction caused by the epiglottis being pushed into the glottic opening
- Esophageal intubation
Suggested reading
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com