Learning objectives
- Understand the indications and contraindications for tonsillectomy
- Anesthetic management for patients undergoing tonsillectomy
- Discuss the management of post-tonsillectomy bleeding
Definition and mechanisms
- Tonsillectomy is a surgical procedure to remove the palatine tonsils, which are lymphoid tissue covered in the respiratory epithelium and invaginated to create crypts
- It is a common procedure in children to treat recurrent acute sore throat
- Adenotonsillar hypertrophy can present with nasal obstruction, recurrent infections, secretory otitis media, deafness (secondary to Eustachian tube dysfunction), and obstructive sleep apnea (OSA)
- The surgery is performed through the mouth using a Boyle-Davis gag → difficulties may be encountered due to a poorly placed gag, obstructing the tracheal tube or laryngeal mask airway
Patient characteristics
- Chronic/recurrent throat infections
- Comorbidities
- OSA
- Congenital abnormalities (e.g., Down syndrome)
- May have malignancy
- Other incidental medical conditions
- Cor pulmonale due to long-term hypoxia
Indications and contraindications for surgery
Absolute indications
- Upper airway obstruction, dysphagia, and OSA
- Peritonsillar abscess, which is unresponsive to adequate medical management and surgical drainage
- Recurrent tonsillitis with associated febrile convulsions
- Requirement for biopsy to confirm tissue pathology
Relative indications
- Recurrent tonsillitis, which is unresponsive to medical treatment
- Sore throat secondary to tonsilitis
- >5 episodes of tonsillitis in one year
- Symptoms >1 year
- Episodes of sore throats are disabling
- Persistent bad breath and taste in the mouth due to chronic tonsillitis
- Persistent tonsillitis in streptococcus carrier, which is unresponsive to beta-lactamase-resistant antibiotics
- Pathology thought to be neoplastic
Contraindications
- Bleeding diathesis
- Acute infection
- Anemia
- Significant anesthetic risk
Management
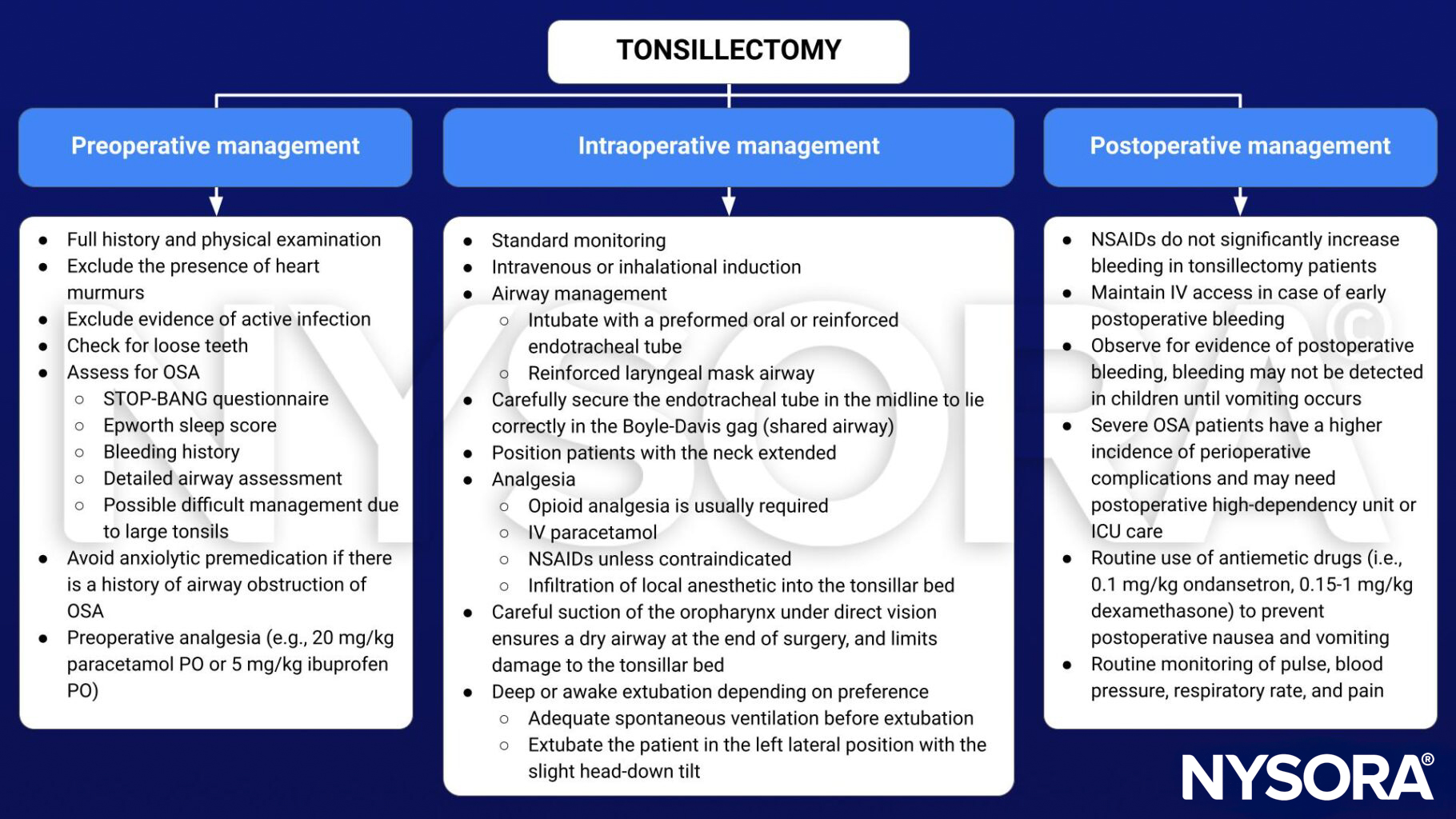
Post-tonsillectomy bleeding
- Serious complication of tonsillectomy that can occur in the recovery or hours later
- Emergency with limited time to optimize
- Persistent swallowing can be an early indicator of bleeding from the tonsillar bed
- Patient may be hypovolemic and require fluid resuscitation before induction → assess patient’s fluid status and cardiovascular parameters
- Risk of aspiration due to potential full stomach with blood
- Potential difficult airway due to blood in the airway and edema from recent intubation
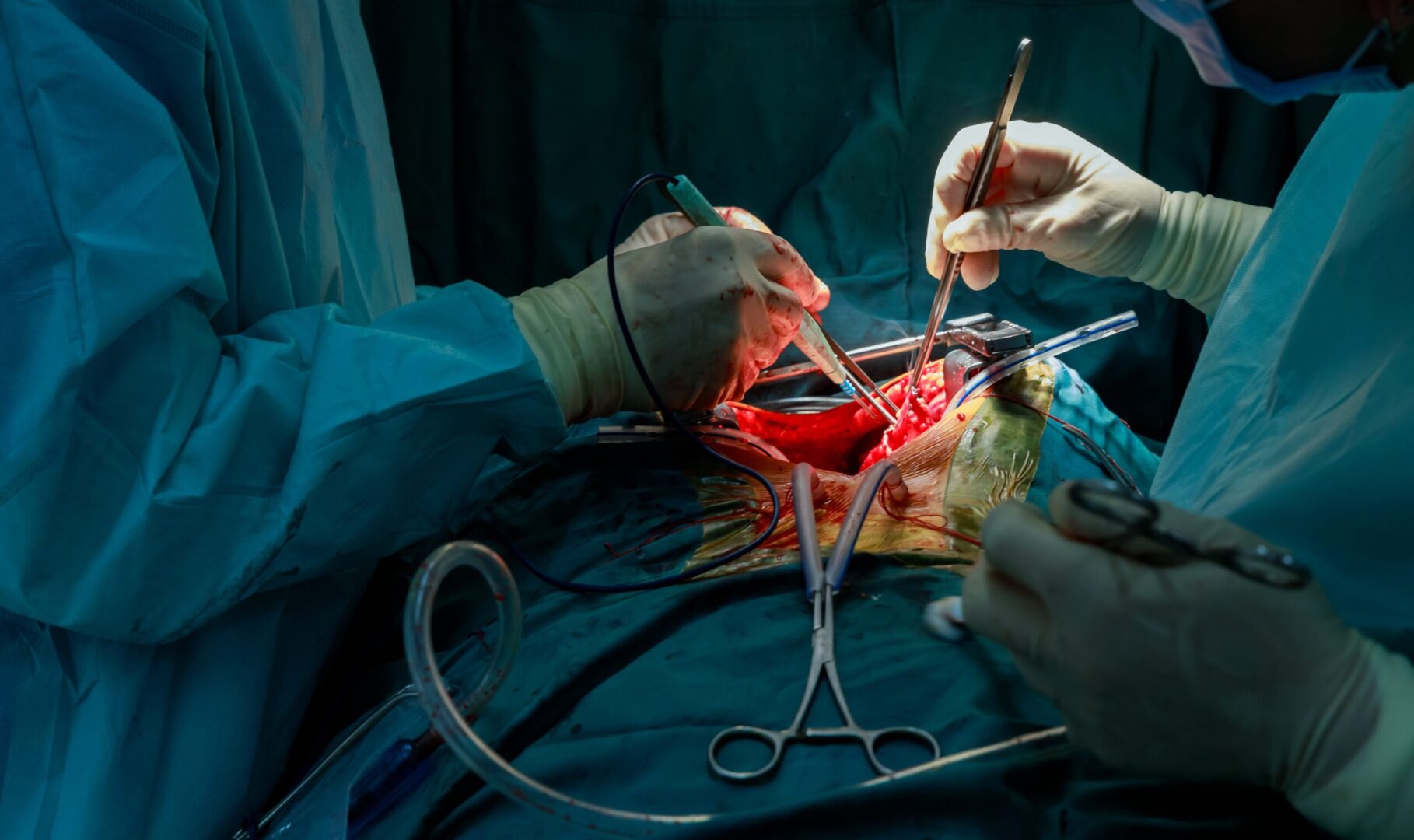
Intraoperative management
- Resuscitate patients and apply full monitoring
- Assess previous anesthetic record
- Suction must be immediately available
- Head-down tilt helps to drain blood away from the larynx
- Rapid sequence induction ensures quick intubation and protects the airway during induction
- Intubation may require a smaller sized endotracheal tube than originally inserted
- Continue fluid resuscitation throughout surgery
- Empty the stomach with a wide-bore naso- or orogastric tube, and ensure that the stomach is empty before extubation
- Extubate patients only when fully awake, in the head-down, left lateral position
Postoperative management
- Patients have to stay in the recovery for an extended period to ensure that the bleeding has stopped
- Check the hemoglobin and coagulation, and transfuse blood if necessary
- Closely monitor patients for further bleeding
Suggested reading
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 19 ENT Surgery, MacNab R, Bexon K, Clegg S, Hutchinson A.
- Davies K. Anaesthesia for tonsillectomy. WFSA. April 2, 2007. Accessed February 10, 2023. https://resources.wfsahq.org/atotw/anaesthesia-for-tonsillectomy/.
Clinical updates
Einhorn et al. (Anesthesiology, 2024) report that a single intraoperative dose of methadone during pediatric tonsillectomy significantly improves postoperative analgesia and reduces opioid requirements without increasing respiratory adverse events. In this randomized study, methadone was associated with lower pain scores and reduced need for rescue opioids compared with standard short-acting opioid regimens.
- Read more about this study HERE.