Jerry D. Vloka and Admir Hadzic
INTRODUCTION
Distal sciatic nerve block (popliteal fossa block) is a very clinically valuable technique that results in anesthesia of the calf, tibia, fibula, ankle, and foot. This section describes the landmarks and nerve stimulator techniques to perform a popliteal sciatic nerve block.
The sciatic nerve can be approached from either the posterior approach, described by Duane Keith Rorie, or the lateral approach, described by Jerry Vloka. Both approaches provide equivalent anesthesia and are suitable for catheter placement. Overall, however, the posterior approach is easier for trainees to learn.
Popliteal fossa block performed with long-acting local anesthetics such as ropivacaine can provide 12–24 hours of analgesia after foot surgery.
When used as a sole technique popliteal fossa block provides excellent anesthesia and postoperative analgesia, allows use of a calf tourniquet, and avoids the disadvantages of neuraxial block.
Analgesia with popliteal fossa blocks lasts significantly longer than with ankle blocks. For instance, David H. McLeod found that lateral popliteal fossa block with 0.5% bupivacaine lasted 18 hours when compared with ankle block, which lasted only 6.2 hours. Popliteal fossa block has also been used as an effective analgesic technique in children. In a study of the efficacy of the popliteal sciatic nerve block (0.75 mL/kg of ropivacaine 0.2%) after foot and ankle surgery, 19 of 20 children required no analgesic agents during the first 8–12 hours postoperatively.
Indications and Contraindications
The popliteal block is one of the most commonly used techniques in regional anesthesia practice. Some common indications include corrective foot surgery, foot debridement, short saphenous vein stripping, repair of the Achilles tendon, and others. As opposed to the more proximal block of the sciatic nerve, popliteal fossa block anesthetizes the leg distal to the hamstring muscles, allowing patients to retain knee flexion.
Functional Anatomy
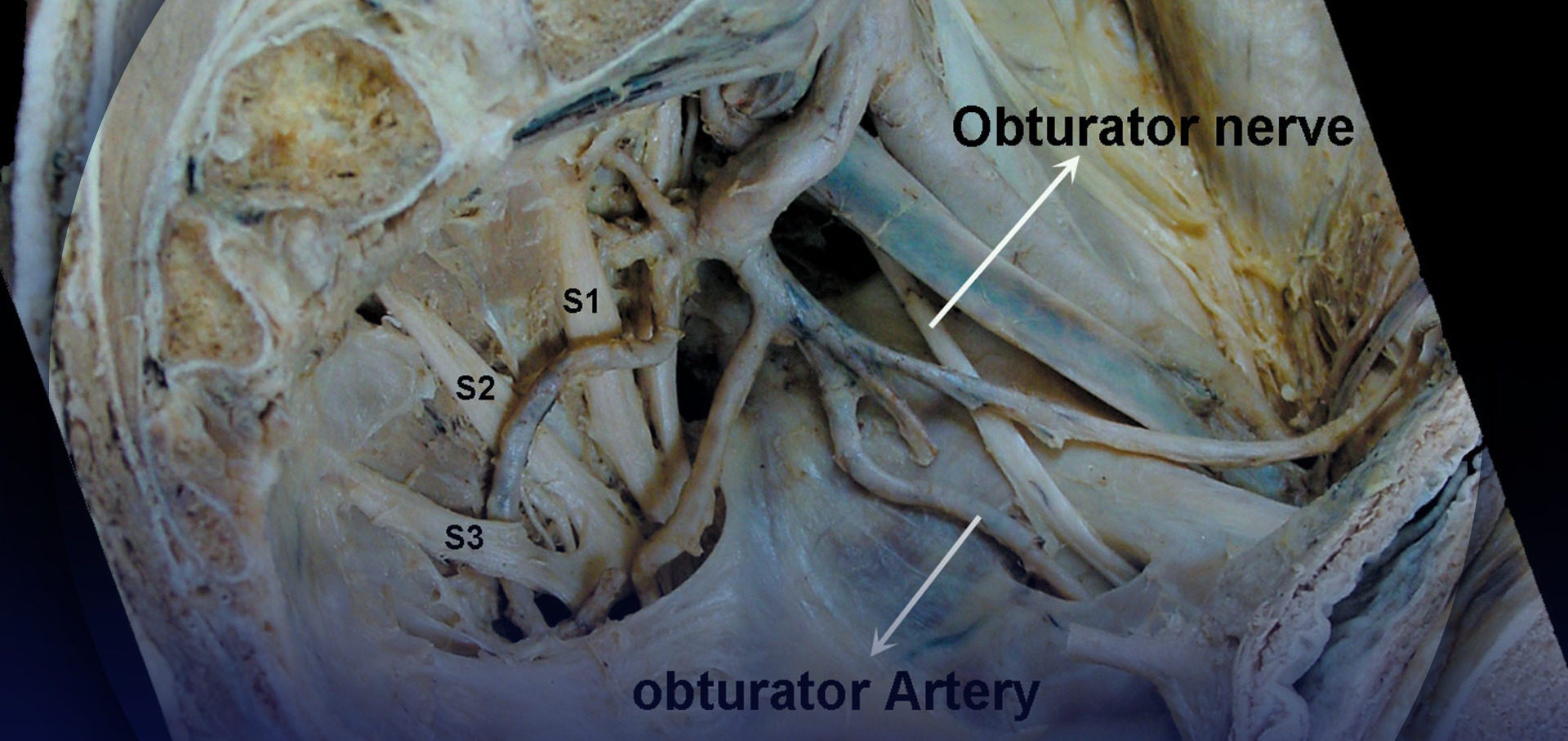
The sciatic nerve consists of two separate nerve trunks: the tibial and common peroneal nerves. A common paraneural sheath envelops these two nerves from their origin in the pelvis, which is distinctly separate from the epineurium of each nerve. Studies utilizing ultrasound imaging have shown that injecting local anesthetic within this sheath consistently gives a rapid onset, safe, and effective block. This is not considered to be an intraneural injection as long as the epineurium of the individual nerves is not breached. As the sciatic nerve descends toward the knee, the two components eventually diverge just proximal to the popliteal fossa, giving rise to the tibial and common peroneal nerves (Figure 1). This division of the sciatic nerve usually occurs between 50 and 120 mm proximal to the popliteal fossa crease. Following its divergence from the sciatic nerve, the common peroneal nerve continues its path laterally and descends along the head and neck of the fibula. Its major branches in this region are branches to the knee joint and cutaneous branches that form the sural nerve. Its terminal branches are the superficial and deep peroneal nerves. The tibial nerve is the larger of the two divisions of the sciatic nerve and continues its path vertically through the popliteal fossa. Its terminal branches are the medial and lateral plantar nerves. Its collateral branches give rise to the cutaneous sural nerves, muscular branches to the muscles to the calf, and articular branches to the ankle joint.
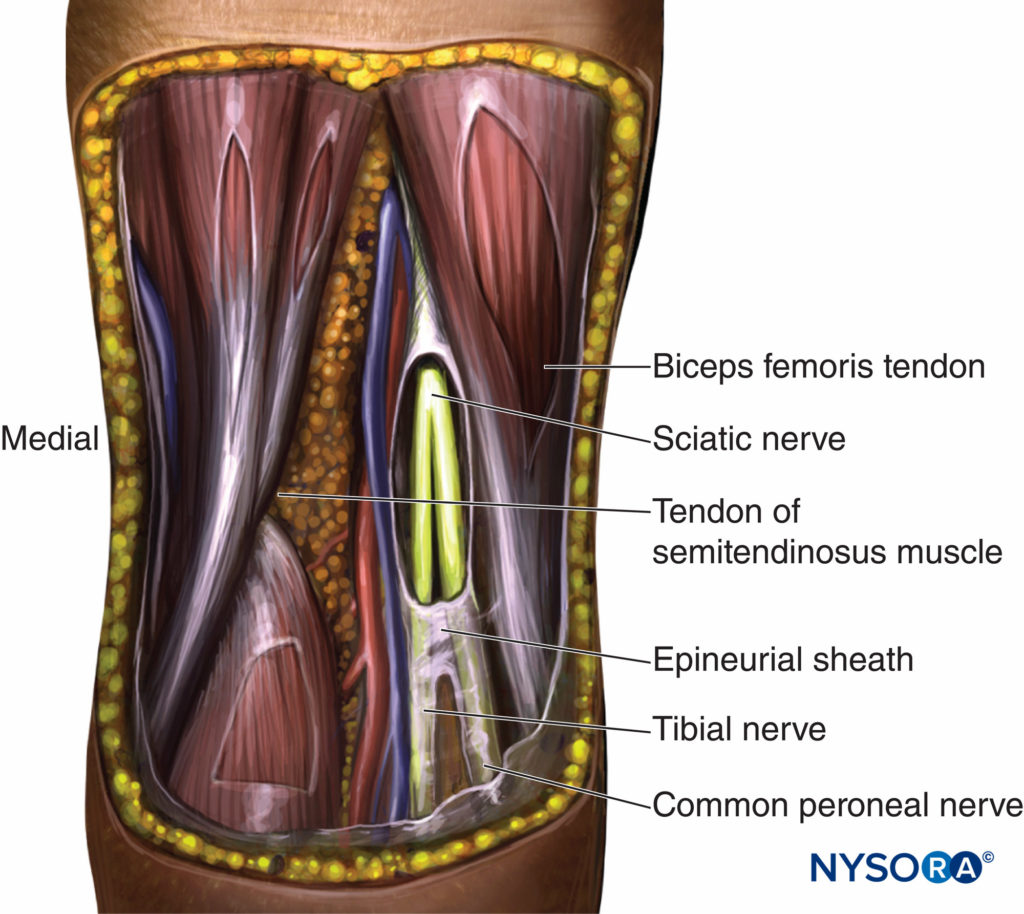
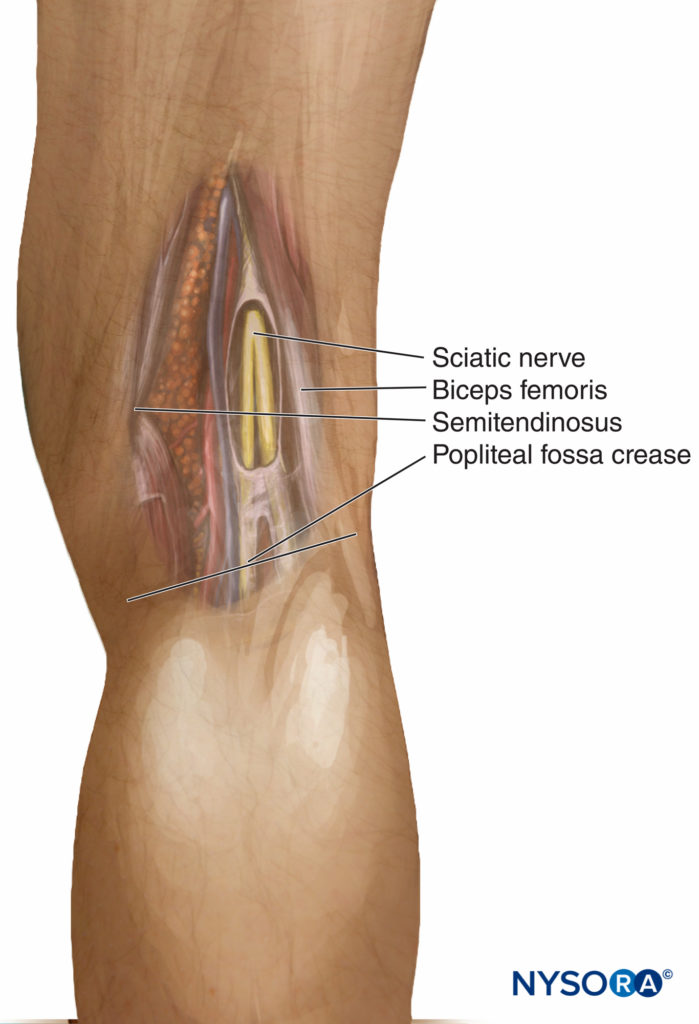
FIGURE 1. Anatomy of the distal sciatic nerve. The sciatic nerve descends between the hamstring muscles and diverges as tibial and common peroneal nerves approximately at or below 7–8 cm above the popliteal fossa crease. A common epineural sheath that serves as a conduit for injected local anesthetic is shown dissected.
The tibial nerve is enveloped by a well-defined paraneural sheath; consequently, a single injection of a large volume of local anesthetic into the sheath of the tibial nerve may carry a higher success rate than an injection into the sheath of the common peroneal nerve. Note that in contrast to the common assumption, the sciatic nerve is not enveloped by the same tissue sheath as are the popliteal vessels; consequently, the concept of the neurovascular sheath is not applicable to this block. Instead, in the popliteal fossa, the sciatic nerve components are lateral and superficial to the popliteal artery and vein. This anatomic characteristic is important in understanding why vascular punctures and systemic toxicity are so rare after popliteal block.
Learn more about Functional Regional Anesthesia Anatomy.
Distribution of Anesthesia
Popliteal block results in anesthesia of the entire distal two thirds of the lower extremity, with the exception of the medial aspect of the leg (Figure 2). Cutaneous innervation of the medial leg below the knee is provided by the saphenous nerve, a superficial terminal extension of the femoral nerve. Depending on the location of surgery, the addition of a saphenous nerve block may be required. Saphenous nerve block is not generally required for patients to tolerate tourniquet pain below the knee because this pain is the result of pressure and ischemia of the deep muscle beds.
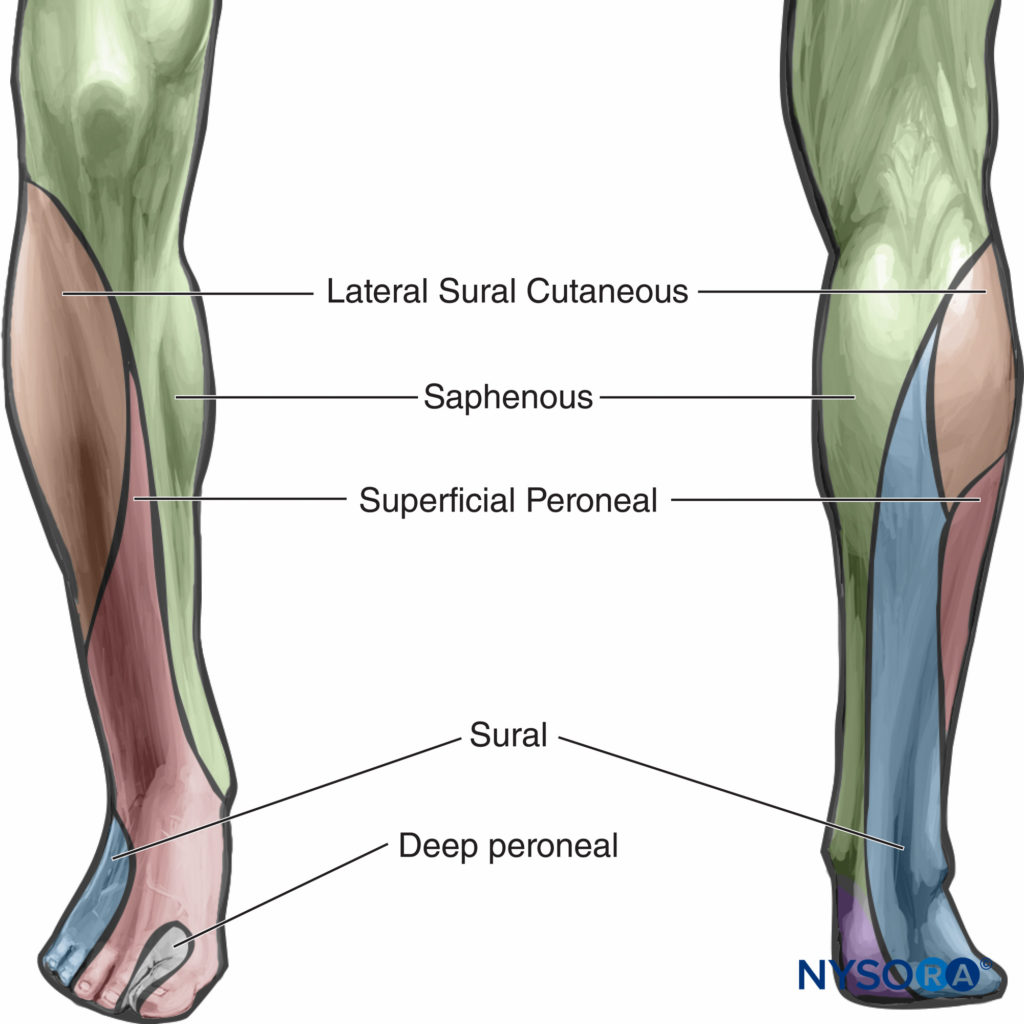
FIGURE 2. Sensory distribution of anesthesia after popliteal block. Popliteal block results in anesthesia of all shaded areas except that of the saphenous nerve (femoral).
Choice of Local Anesthetic
Popliteal block requires a larger volume of local anesthetic (20 mL) to achieve anesthesia of both divisions of the nerve. The choice of type, volume, and concentration of local anesthetic should be based on the patient’s size and general condition and whether the block is planned for surgical anesthesia or pain management. The type and concentration of local anesthetics and the choice of additives to local anesthetic influence the onset and, particularly, the duration of the block (Table 1).
TABLE 1. Local anesthetics choice for popliteal block.
| Onset (min) | Anesthesia (h) | Analgesia (h) | |
|---|---|---|---|
| 3% 2-Chloroprocaine | 10–15 | 1 | 2 |
| 1.5% Mepivacaine | 15–20 | 2–3 | 3–5 |
| 1.5% Mepivacaine epinephrine | 15–20 | 2–5 | 3–8 |
| 2% Lidocaine epinephrine | 10–20 | 2–5 | 3–8 |
| 0.5% Ropivacaine | 15–30 | 4–8 | 5–12 |
| 0.75% Ropivacaine | 10–15 | 5–10 | 6–24 |
| 0.5 (L) Bupivacaine | 15–30 | 5–15 | 6–30 |
TECHNIQUES
Intertendinous (Posterior) Approach
The patient is in the prone position. The foot on the side to be blocked should be positioned so that even the slightest movement of the foot or toes can be easily observed. This is best achieved by allowing the foot to protrude off the edge of the bed.
Equipment
A standard regional anesthesia tray is prepared with the following equipment:
- Sterile towels and 4-in. × 4-in. gauze packs
- One 20-mL syringes with local anesthetic
- Sterile gloves, marking pen, and surface electrode
- One 1.5-in., 25-gauge needle for skin infiltration
- A 5-cm long, short-bevel, insulated stimulating needle
- Peripheral nerve stimulator
- Injection pressure monitor
Learn more about Equipment for Regional Anesthesia.
Anatomic Landmarks
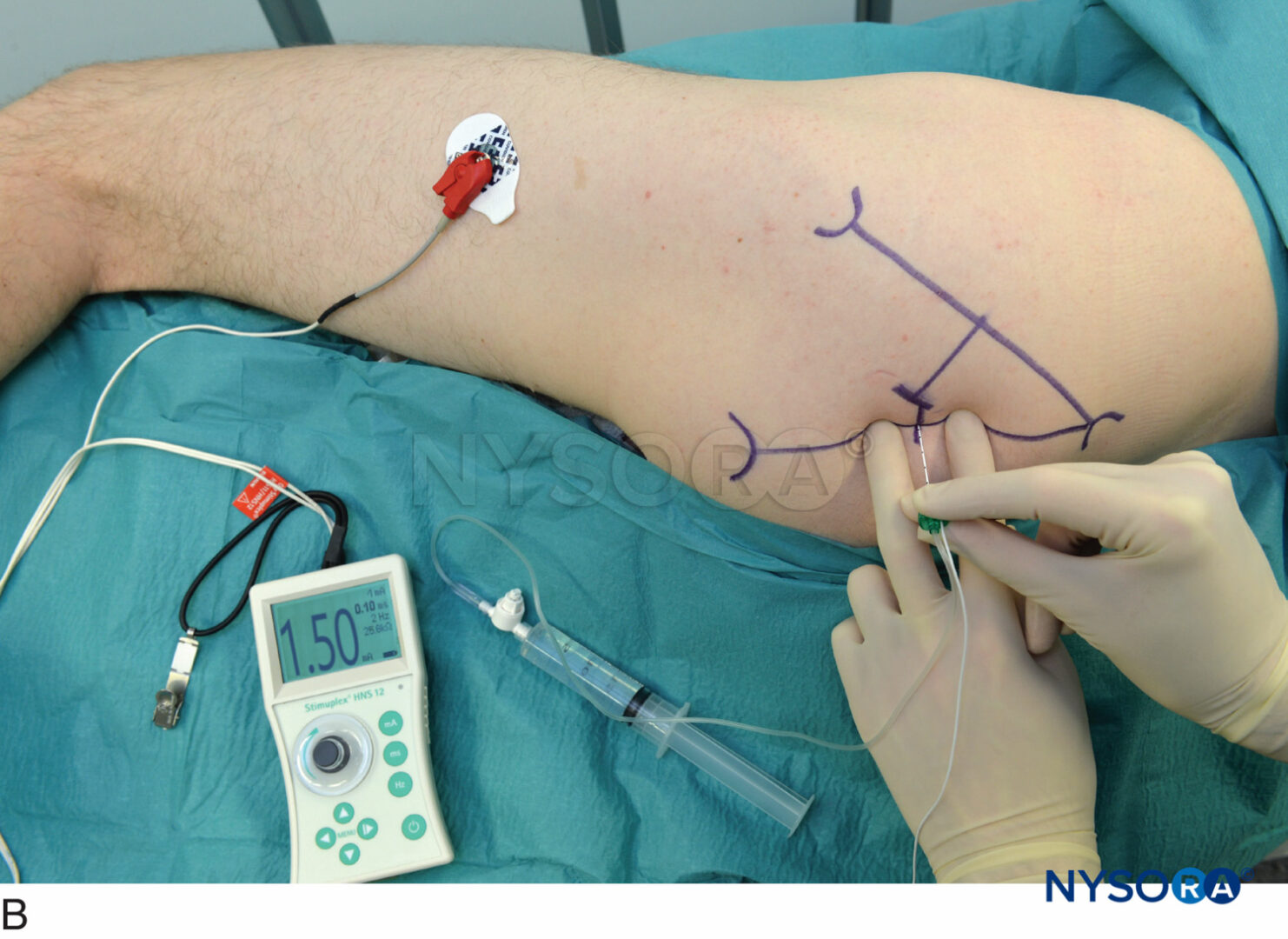
Landmarks for this approach are easily identified, even in obese patients (Figure 3). The landmarks should be routinely outlined by a marking pen: (1) popliteal fossa crease, (2) tendon of biceps femoris (laterally), and (3) tendons of semitendinosus and semimembranosus (medially). The needle insertion point is marked at 7 cm above the popliteal fossa crease at the midpoint between the tendons. This point is just above the sciatic nerve in the popliteal fossa in nearly two thirds of patients (Figure 4).
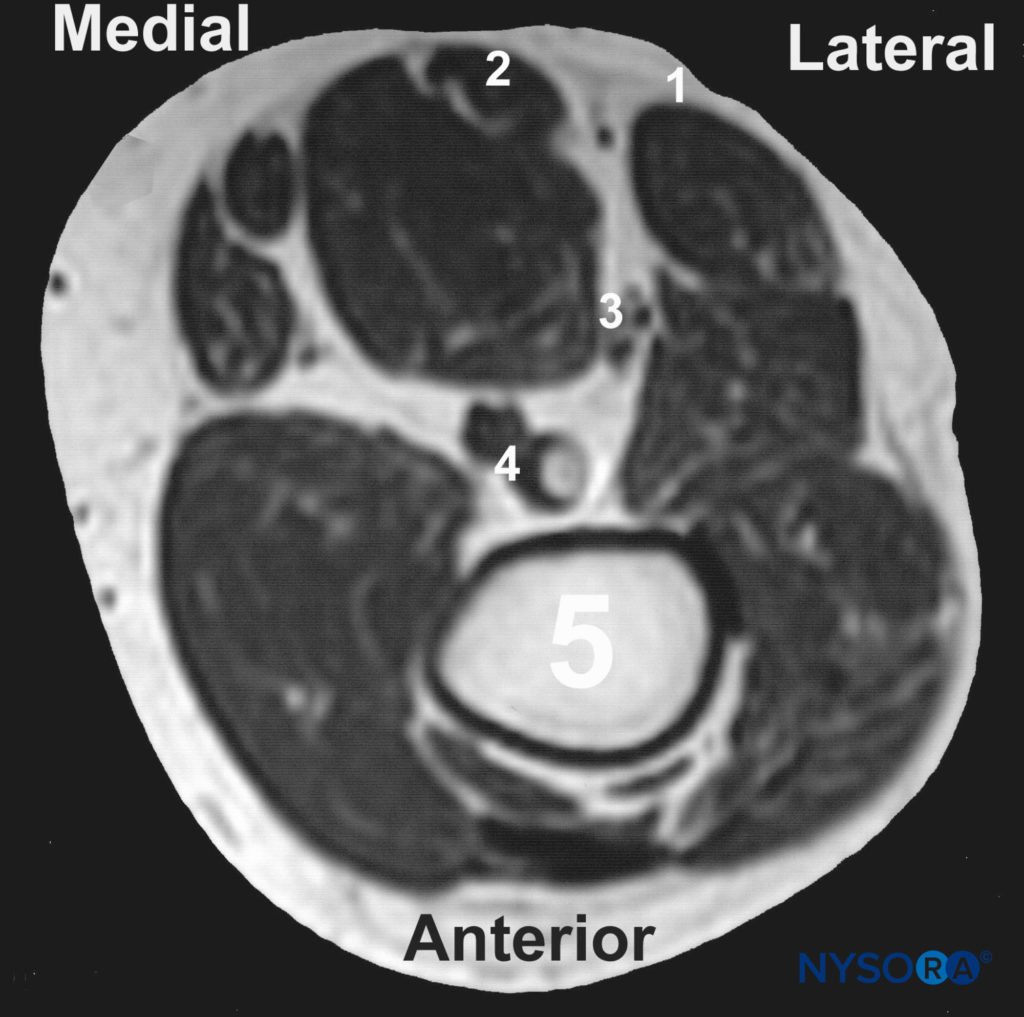
FIGURE 4. Magnetic resonance image (MRI) of the popliteal fossa 7 cm above the popliteal fossa crease. 1, Tendon of the biceps femoris muscle; 2, tendon of the semitendinosus muscle; 3, sciatic nerve in the popliteal fossa (shown are both components: the tibial nerve is positioned more anteriorly and medially, whereas the common peroneal nerve is more posterior and lateral); 4, popliteal artery and vein; 5, femur.
NYSORA Tips
- Relying on tendons (rather than on subjective interpretation of the “popliteal fossa triangle” as described else-where) gives a much more precise and consistent localization of the popliteal nerve.
- The landmarks can be accentuated by asking the patient to flex the knee joint (Figure 5). This maneuver tightens the hamstring muscles and facilitates more accurate palpation of the tendons.
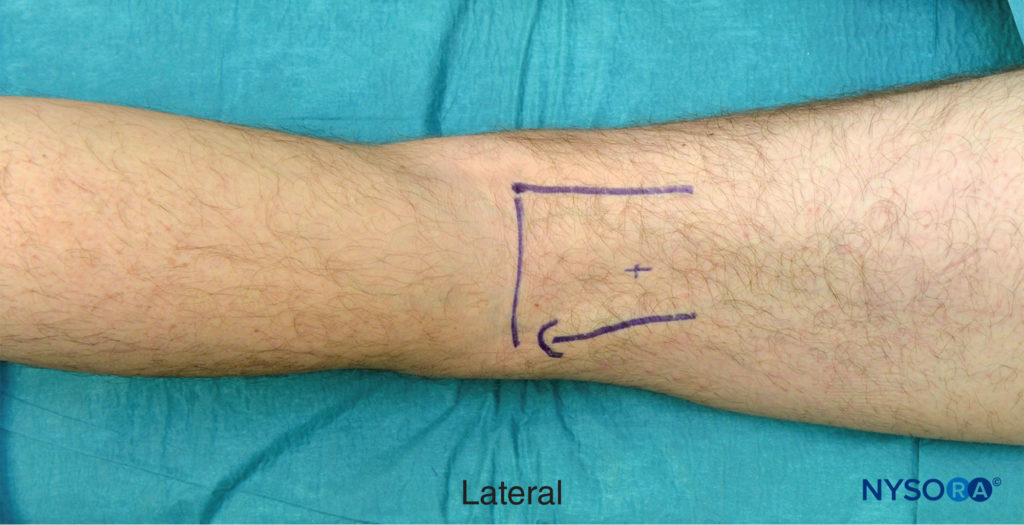
FIGURE 5. Landmarks for the popliteal block, intertendinous approach. The landmarks can be accentuated by asking the patient to flex the leg. The arrow indicates attachment of the biceps femoris tendon; + sign indicates site of needle placement.
Technique
The practitioner is best positioned on the side of the patient with the palpating hand on the biceps femoris muscle while observing the motor response of the foot and toes (Figure 6A-C). The needle is introduced at the mid-point between the tendons. The nerve stimulator should be initially set to deliver 1.5 mA current (2 Hz, 100 μsec). When the needle is inserted in the correct plane, advancement of the needle should not result in any local muscular twitches; the first response to nerve stimulation is typically that of the sciatic nerve (foot twitch). The stimulating current is gradually decreased and the needle repositioned until twitches are still seen or felt at 0.2–0.5 mA. This typically occurs at a depth of 3–5 cm from the skin. After negative aspiration for blood, 20 mL of local anesthetic is slowly injected.

FIGURE 6. A. Popliteal block, intertendinous approach. The needle is inserted perpendicularly between tendons of the biceps femoris and semitendinosus muscles. B. In case no foot or toe twitch can be elicited, withdraw and redirect 15 degrees laterally. C. In case no foot or toe twitch can be elicited after redirection, withdraw needle completely, reinsert 1 cm laterally, and repeat the procedure starting with perpendicular needle insertion.
NYSORA Tips
- In patients with long-standing diabetes mellitus, peripheral neuropathy, sepsis, or severe peripheral vascular disease. Stimulating currents up to 1 mA can be accepted.
- When a rather small change in the needle position (e.g.,1 mm) results in a change of the motor response from that of the popliteal nerve (plantar flexion of the foot) to that of the common peroneal nerve (dorsiflexion of the foot), the needle tip is above the divergence of the sciatic into tibial and common peroneal nerves.
- Entrance of the needle into the sciatic sheath is almost always associated with a “fascial click.” The skilled practitioner should use this sign as a valuable clue in conjunction with the nerve stimulation information to ascertain proper needle position.
- Absence of high opening injection pressure is essential to assure extrafascicular needle placement as motor response may be absent after injection.
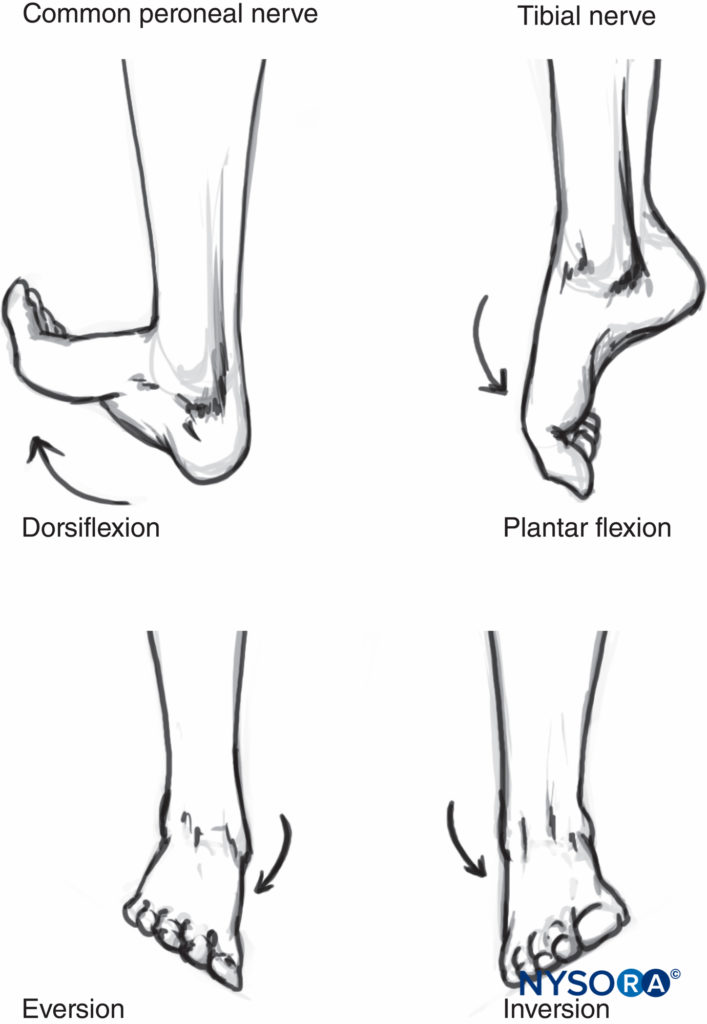
There are two types of motor responses that can be elicited with sciatic nerve stimulation at the level of the popliteal fossa. Common peroneal nerve stimulation results in dorsiflexion and eversion of the foot, whereas stimulation of the tibial nerve results in plantar flexion and inversion (Figure 7). As the stimulating current is being decreased, the twitch of the great toe often remains the only motor response seen with currents of <0.5 mA. Either response is adequate when the response is still present with current intensity of 0.2–0.4 mA (0.1 msec) as long as a large volume of local anesthetic is used. Some common responses to nerve stimulation and the course of action to obtain the proper response are shown in Table 2.
TABLE 2. Intertendinous popliteal block: troubleshooting.
| Response Obtained | Interpretation | Problem | Corrective Action |
|---|---|---|---|
| Local twitch of the biceps muscle | Direct stimulation of the biceps femoris muscle | Too lateral placement of the needle | Withdraw the needle and redirect slightly medially (5–10 degrees) |
| Local twitch of the semitendinosus/membranosus muscles | Direct stimulation of the semitendinosus/membranosus muscles | Too medial placement of the needle | Withdraw the needle and redirect slightly laterally (5–10 degrees) |
| Twitch of the calf muscles without foot or toe movement | Stimulation of the muscular branches of the sciatic nerve | These small branches are often outside the sciatic sheath | Disregard and continue advancing the needle until the foot/toes twitches are obtained |
| Vascular puncture | Blood in the syringe most commonly indicates placement into the popliteal artery or vein | Too medial or too deep needle placement | Withdraw and redirect laterally |
| Bone contact | The needle encounters the femur | Too deep needle insertion—either the nerve was missed or motor response was not appreciated | Withdraw the needle slowly and look for the foot twitch; if twitches are not seen, reinsert in another direction |
Block Dynamics and Perioperative Management
The intertendinous approach to the popliteal block is associated with relatively minor patient discomfort because the needle passes only through the adipose tissue of the popliteal fossa. Regardless, adequate sedation and analgesia are always important to ensure a still and tranquil patient. Midazolam 1–2 mg after the patient is positioned and alfentanil 250–500 mcg or 5 mg ketamine just before block placement suffices for most patients. A typical onset time for this block is 10–25 minutes, depending on the type, concentration, and volume of local anesthetic used. The first signs of block onset are usually that the patient reports that the foot “feels different” or that they are unable to wiggle the toes. Sensory anesthesia of the skin with this block is often the last to develop. Inadequate skin anesthesia despite the apparent timely onset of the block is common because it may take up to 30 minutes for full block to develop. However, local infiltration at the site of the incision is often all that is needed to allow the surgery to proceed.
Continuous Popliteal Block
Continuous popliteal block is an advanced regional anesthesia technique, and adequate experience with the single-shot technique is necessary to ensure its efficacy. The technique is similar to the single-shot injection; however, slight angulation of the needle cephalad is necessary to facilitate insertion of the catheter. This technique can be used for surgery and postoperative pain management in patients undergoing a wide variety of lower leg, foot, and ankle surgeries.
Ilfeld reported excellent postoperative analgesia using a continuous catheter in the popliteal fossa and a portable infusion pump for outpatients having moderately painful, lower extremity orthopedic surgery. The patients who received ropivacaine experienced a significant decrease in sleep disturbances, oral opioid use, and opioid-related adverse effects, and had a high rate of satisfaction with the technique.
Klein et al. examined the efficacy and complications of long-acting popliteal nerve block after discharge home. This prospective study included 1791 patients who had received an upper- or lower-extremity nerve block with 0.5% ropivacaine and were discharged on the day of surgery. The results showed that long-acting popliteal nerve block may be used in the ambulatory setting with a high degree of efficacy, safety, and satisfaction.
Chelly et al. documented the benefits of a continuous lateral popliteal sciatic nerve block infusion technique for postoperative analgesia in patients who had undergone open reduction and internal fixation of the ankle. Continuous infusion of ropivacaine 0.2% was associated with a significant reduction of morphine consumption by 29% and 62% during postoperative days 1 and 2, respectively.
Technique
After insertion, the block needle is advanced slowly with a slight cranial direction while seeking a motor response. After obtaining an appropriate motor response at a current of 0.5 mA, a bolus of local anesthetic is injected (10-15 ml) and the catheter advanced 5 cm beyond the needle tip (Figure 8). The catheter is aspirated to check for inadvertent intravascular placement, then an infusion can be started. A typical infusion regimen is ropivacaine 0.2% at 5 mL/h with a 5 mL/q60min patient-controlled bolus.
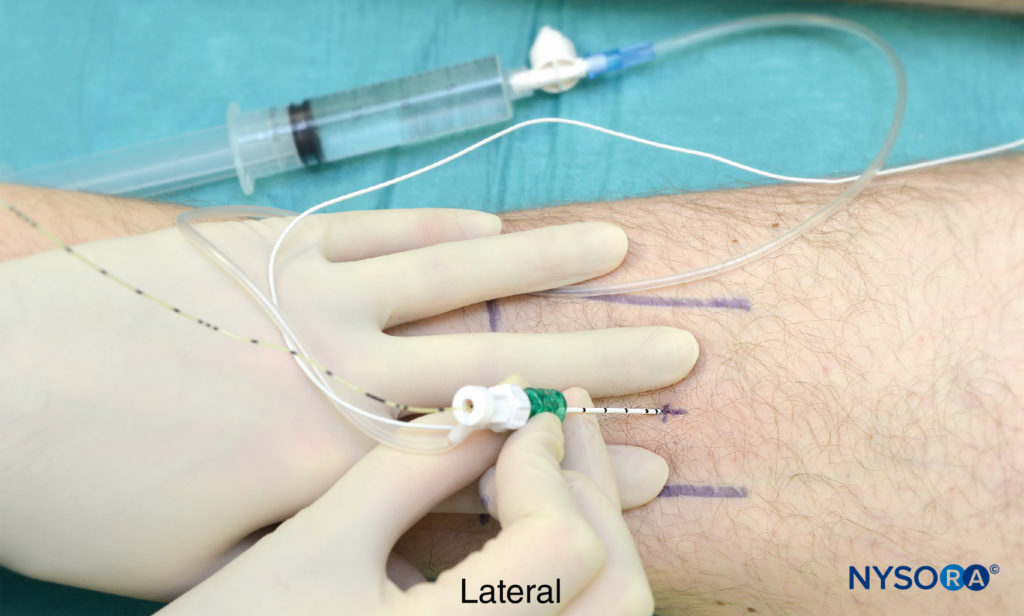
FIGURE 8. Image depicts a non-sterile catheter field. Popliteal block, intertendinous approach. Catheter insertion.
NYSORA Tips
- Breakthrough pain in patients on continuous infusion is always managed by administering a bolus of local anesthetic. Increasing only the rate of infusion is never adequate.
- Patients receiving continuous nerve block infusion should also be prescribed an alternative oral or intravenous (e.g., intravenous patient-controlled analgesia [IV PCA]) pain management protocol because incomplete analgesia and catheter dislodgement can occur leaving the patient without a back-up option.
Popliteal (Lateral) Approach
The main advantage of the lateral approach, described by Jerry Vloka is that the patient does not need to be positioned in the prone position.
Regional Anesthesia Anatomy
The sciatic nerve is located between the biceps and semitendinosus muscles (see Figure 4). During block performance, stimulation of the common peroneal nerve is usually obtained first (65%) because this nerve is positioned more lateral and superficial than the tibial nerve.
Patient Positioning
The patient is in the supine position. The foot on the side to be blocked should be positioned so that even the slightest movement of the foot or toes can be easily observed. This is best achieved by placing the foot on a footrest.
Equipment
The equipment is identical to that for the posterior intertendinous approach except that a 10-cm stimulating needle is used.
Learn more about Equipment for Regional Anesthesia.
Anatomic Landmarks
Landmarks for the lateral approach to popliteal block include the popliteal fossa crease, vastus lateralis muscle, and biceps femoris muscle (Figure 9). The needle insertion site is marked in the groove between the vastus lateralis and biceps femoris muscles, 8 cm proximal to the popliteal crease (Figure 10).

FIGURE 9. Popliteal block, lateral approach. Landmarks for this technique include vastus lateralis (VL), biceps femoris (BF), and popliteal fossa crease. The needle insertion site is marked 8 cm above the popliteal fossa crease (thick vertical line).
Technique
The operator should be seated, facing the side to be blocked. The height of the patient’s bed is adjusted to allow for an ergonomic position and greater precision during block placement. This position also allows the operator to simultaneously monitor both the patient and the responses to nerve stimulation. The site of needle insertion is cleaned with an antiseptic solution and infiltrated with local anesthetic.
A 10-cm, 22-gauge needle is connected to a nerve stimulator inserted in a horizontal plane between the vastus lateralis and biceps femoris muscles, and advanced to contact the femur (see Figure 10). The contact with the femur is important because it provides information on the depth of the nerve (typically 1–2 cm beyond the skin–femur distance) as well as on the angle at which the needle will need to be redirected posterior to stimulate the nerve.

FIGURE 10. Popliteal block, lateral approach. The needle is inserted between vastus lateralis (VL) and biceps femoris in the horizontal plane to contact the femur.
The current intensity is initially set at 1.5 mA. Keeping the fingers of the palpating hands firmly pressed and immobile in the groove, the needle is then withdrawn to the skin, redirected 30 degrees posterior to the angle at which the femur was contacted, and advanced toward the nerve (Figure 11).

FIGURE 11 After the femur is contacted, the needle is redirected 30 degrees posterior to the plane in which the femur was contacted. VL, vastus.
When the sciatic nerve is not localized on the first needle pass, the needle is withdrawn to the skin level and the following procedure is followed:
NYSORA Tips
- Assure that the nerve stimulator is functional and properly connected to the patient and to the needle and that it is set to deliver current of desired intensity.
- Assure that the leg is not externally rotated at the hip joint and that the foot forms a 90-degree angle to the horizontal plane of the table. Any deviation from this angle changes the relationship of the sciatic nerve to the femur and biceps femoris muscle.
- Mentally visualize the plane of the initial needle insertion and redirect the needle in a slightly posterior direction (5–10 degrees posterior angulation).
- If the above maneuver fails, withdraw the needle and reinsert with an additional 5–10 degrees posterior redirection.
- If the above maneuvers fail, withdraw the needle to the skin and reinsert 1 cm inferior to the initial insertion site; then repeat the above steps.
- Failure to obtain foot response to nerve stimulation should prompt reassessment of the landmarks and leg position. In addition, the stimulating current should be increased to 2 mA.
After the initial stimulation of the sciatic nerve is obtained, the stimulating current is gradually decreased until the motor response of the foot or toes is still seen or felt at 0.5 mA. This typically occurs at a depth of 5–7 cm. Entrance of the needle into the sheath with a Touhy-style tip needle is often accompanied by a perceptible “click.” At this point, the needle should be stabilized, and after negative aspiration for blood, 20 mL of local anesthetic is slowly injected. The hands should be kept as immobile as possible to prevent injection outside the sheath of the sciatic nerve.
Continuous Popliteal Block Through the Lateral Approach
The continuous popliteal block technique through the lateral approach is similar to the single-injection technique, except that a 10-cm Tuohy-style tip needle is used. When the needle is directed toward the sciatic nerve, a slight cranial angulation should be taken to facilitate catheter insertion (Figure 12). After obtaining appropriate twitches at 0.2–0.5 mA, a bolus of local anesthetic is injected and the catheter advanced 5–7 cm beyond the tip of the needle. The management of the catheter is similar to that of the intertendinous technique.

FIGURE 12. Popliteal block, lateral approach. Continuous technique is similar to the single-injection method except that a larger needle is used. The needle opening should be directed cephalad, and a slight cephalad needle angulation is used after localization of the sciatic nerve; these maneuvers facilitate insertion of the catheter.
NYSORA Tips
- In some patients, the biceps muscle may be atrophic and the iliotibial aponeurosis may be more prominent. In such cases, the needle insertion site is labeled in the groove between the vastus lateralis and the iliotibial tract.
- Flexing the patient’s leg in the knee helps with identification of the popliteal fossa crease and the biceps and vastus lateralis muscles (Figure 13).

FIGURE 13. Popliteal block, lateral approach. Asking the patient to flex the leg in the knee joint facilitates identification of the landmarks (popliteal fossa crease, vastus lateralis, and biceps femoris).
Some common responses during block placement using a nerve stimulator and the course of proper action to obtain twitches of the foot (Table 3).
TABLE 3. Lateral popliteal block: troubleshooting.
| Response Obtained | Interpretation | Problem | Corrective Action |
|---|---|---|---|
| Local twitch of the biceps muscle | Direct stimulation of the biceps femoris muscle | Too shallow placement of the needle | Advance the needle deeper |
| Local twitch of the vastus lateralis muscle | Direct stimulation of the vastus lateralis muscles | Too anterior placement of the needle | Withdraw the needle and reinsert posterior |
| Twitch of the calf muscles without foot or toe movement | Stimulation of the muscular branches of the sciatic nerve | These small branches are often outside the sciatic sheath | Disregard and continue advancing the needle until the foot/toes twitches are obtained |
| Vascular puncture | Blood in the syringe most commonly indicates placement into the popliteal artery or vein | Too deep and anterior placement of the needle placement | Withdraw and redirect laterally |
| Twitches of the foot or toes | Stimulation of the sciatic nerve | None | Accept and inject local anesthetic |
COMPLICATIONS AND HOW TO AVOID THEM
A retrospective review of 400 continuous popliteal catheters revealed one case of infection (abscess formation requiring surgical drainage) and two cases of nerve injury resulting in paresthesias. Table 4 provides specific instructions on possible complications and how to avoid them. Special attention should be paid when common peroneal response is elicited as most neurologic injuries occur to this nerve, probably because of its composition where there is often one or two large fascicles that present a greater risk for intrafascicular needle placement.
TABLE 4. Complications of popliteal block and measures to prevent them.
| Infection | • Use strict aseptic technique |
| Hematoma | • Avoid multiple needle passes with a continuous block needle; the larger needle diameter and/or Tuohy design may result in a hematoma of the biceps femoris or vastus lateralis muscles |
| Vascular puncture | • Avoid too deep insertion of needle because the vascular sheath is positioned medially and deeper to the sciatic nerve • When the nerve is not localized within 2 cm after the local twitches of the biceps muscle cease, the needle should be withdrawn and reinserted at a different angle, rather than advanced deeper |
| Nerve injury | • Use nerve stimulation and slow needle advancement; do not inject when patient complains of pain or high pressures on injection are met; do not inject when stimulation is obtained at <0.2 mA current (100 μsec) |
| Pressure necrosis of the heel | • Instruct patient on the care of the insensate extremity• Use heel padding and frequent repositioning |
SUMMARY
Popliteal sciatic block is useful technique to accomplish anesthesia and analgesia for ankle and foot surgery. Posterior and lateral approaches are both highly effective and applicable in numerous clinical scenarios.
REFERENCES
- Hadzic A, Vloka JD: A comparison of the posterior versus lateral approaches to the block of the sciatic nerve in the popliteal fossa. Anesthesiology 1998;88:1480–1486.
- Rongstad K, Mann RA, Prieskorn D, et al: Popliteal sciatic nerve block for postoperative analgesia. Foot Ankle Int 1996;17:378–382.
- Rorie DK, Byer DK, Nelson DO, et al: Assessment of block of the sciatic nerve in the popliteal fossa. Anesth Analg 1980;59:371–376.
- Singelyn FJ, Gouverneur JM, Gribomont BF: Politeal sciatic nerve block aided by a nerve stimulator: a reliable technique for foot and ankle surgery. Reg Anesth 1991;16:278–281.
- Hansen E, Eshelman MR, Cracchiolo A: Popliteal fossa neural block as the sole anesthetic technique for outpatient foot and ankle surgery. Foot Ankle Int 2000;21:38–44.
- McLeod DH, Wong DH, Claridge RJ, Merrick PM: Lateral popliteal sciatic nerve block compared with subcutaneous infiltration for analgesia following foot surgery. Can J Anaesth 1994;41:673–676.
- Tobias JD, Mencio GA: Popliteal fossa block for postoperative analgesia after foot surgery in infants and children. J Pediatr Orthop 1999;19:511–514.
- Vloka JD, Hadzic A, Mulcare R, et al: Combined blocks of the sciatic nerve at the popliteal fossa and posterior cutaneous nerve of the thigh for short saphenous vein stripping in outpatients: an alternative to spinal anesthesia. J Clin Anesth 1997;9:618–622.
- Ilfeld BM, Morey TE, Wang DR, Enneking F K: Continuous popliteal sciatic nerve block for postoperative pain control at home: a randomized, double-blinded, placebo-controlled study. Anesthesiology 2002;97: 959–965.
- Mulroy MF, McDonald SB: Regional anesthesia for outpatient surgery. Anesthesiol Clin North Am 2003;21:289–303.
- Vloka JD, Hadzic A, Lesser JB, et al: A common epineural sheath for the nerves in the popliteal fossa and its possible implications for sciatic nerve block. Anesth Analg 1997;84:387–390.
- Perlas A, Wong P, Abdallah F: Ultrasound-guided popliteal block through a common paraneural sheath versus conventional injection: a prospective, randomized, double-blind study. Reg Anesth Pain Med. 2013;38: 218–225.
- Andersen HL, Andersen SL, Tranum-Jensen J: Injection inside the paraneural sheath of the sciatic nerve: direct comparison among ultrasound imaging, macroscopic anatomy, and histologic analysis. Reg Anesth Pain Med. 2012;37:410–414.
- Franco D: Connective tissues associated with peripheral nerves. Reg Anesth Pain Med. 201;37:363–365.
- Sunderland S: The sciatic nerve and its tibial and common peroneal divisions. anatomical features. In: Sunderland S (ed): Nerves and Nerve Injurie. Edenburgh, Scotland: Livingstone, 1968, 543:1012–1095.
- Vloka JD, Hadzic A, April EW, et al: Division of the sciatic nerve in the popliteal fossa and its possible implications in the popliteal nerve block. Anesth Analg 2001;92:215–217.
- Benzon HT, Kim C, Benzon HP, et al: Correlation between evoked motor response of the sciatic nerve and sensory block. Anesthesiology 1997;87:548–552.
- Vloka JD, Hadzic A, Koorn R, Thys D: Supine approach to the sciatic nerve in the popliteal fossa. Can J Anaesth 1996;43:964–967.
- Hadzic A, Vloka JD: Popliteal block. In: Hadzic A, Vloka J (eds): Peripheral Nerve Blocks: Principles and Practice. New York, NY: McGraw-Hill, 2004.
- Saporito A, Sturini E, Borgeat A, Aguirre J: The effect of continuous popliteal sciatic nerve block on unplanned postoperative visits and readmissions after foot surgery –a randomised, controlled study comparing day-care and inpatient management. Anaesthesia. 2014;69:1197–1205.
- Klein SM, Nielsen KC, Greengrass RA: Ambulatory discharge after long-acting peripheral nerve block: 2382 blocks with ropivacaine. Anesth Analg 2002;94:65–70.
- Chelly JE, Greger J, Casati A: Continuous lateral sciatic blocks for acute postoperative pain management after major ankle and foot surgery. Foot Ankle Int 2002;23:749–752.
- Zetlaoui PJ, Bouaziz H: Lateral approach to the sciatic nerve in the popliteal fossa. Anesth Analg 1998;87:79–82.
- Compére V, Rey N, Baert O, et al: Major complications after 400 continuous popliteal sciatic nerve blocks for post-operative analgesia. Acta Anaesthesiol Scand. 2009;53:339–345.