Securing a child’s airway during general anesthesia is a high-stakes procedure. For pediatric anesthesiologists, recognizing the nuances of a child’s anatomy, underlying health, and procedure-specific factors is critical. A new landmark study from Japan sheds light on when and why airway complications occur, and how to prevent them.
A multicenter, prospective observational study, known as the J-PEDIA study (Japan Pediatric Difficult Airway in Anesthesia), has analyzed over 17,000 airway management procedures across 10 tertiary care hospitals. The findings are both reassuring and enlightening, offering practical strategies for improving safety in pediatric anesthesia.
Key findings at a glance
- Adverse event rate during airway management: 2.0%
- Respiratory-specific events: 1.1%
- Desaturation events (≥ 10% SpO₂ drop): 2.3%
- Higher risk in neonates, infants, and children with difficult airway features
- Lower risk when supraglottic devices or muscle relaxants were used
Why airway management matters in children
Children are anatomically and physiologically distinct from adults:
- Smaller airway diameters
- Higher oxygen consumption
- Reduced apnea tolerance
These factors contribute to an increased likelihood of life-threatening events if the airway is not secured quickly and effectively during anesthesia.
About the J-PEDIA study
Study design:
- Period: June 2022 – January 2024
- Institutions: 10 tertiary centers (6 pediatric, 4 mixed adult-pediatric)
- Population: 16,695 children; 17,007 airway management encounters
Objective: To evaluate the incidence of adverse events during airway-securing procedures and identify modifiable and non-modifiable risk factors.
What qualifies as an adverse event?
The study tracked both hemodynamic and airway-related events, including:
- Laryngospasm
- Bronchospasm
- Esophageal intubation
- Vomiting with aspiration
- Pulmonary edema
- Cardiac arrhythmia
- Stridor
- Desaturation (≥ 10% drop in SpO₂)
These were assessed from preoxygenation through successful device placement, ensuring the child was stable both respiratorily and hemodynamically.
Which children are most at risk?
The data revealed several high-risk groups for airway-related adverse events:
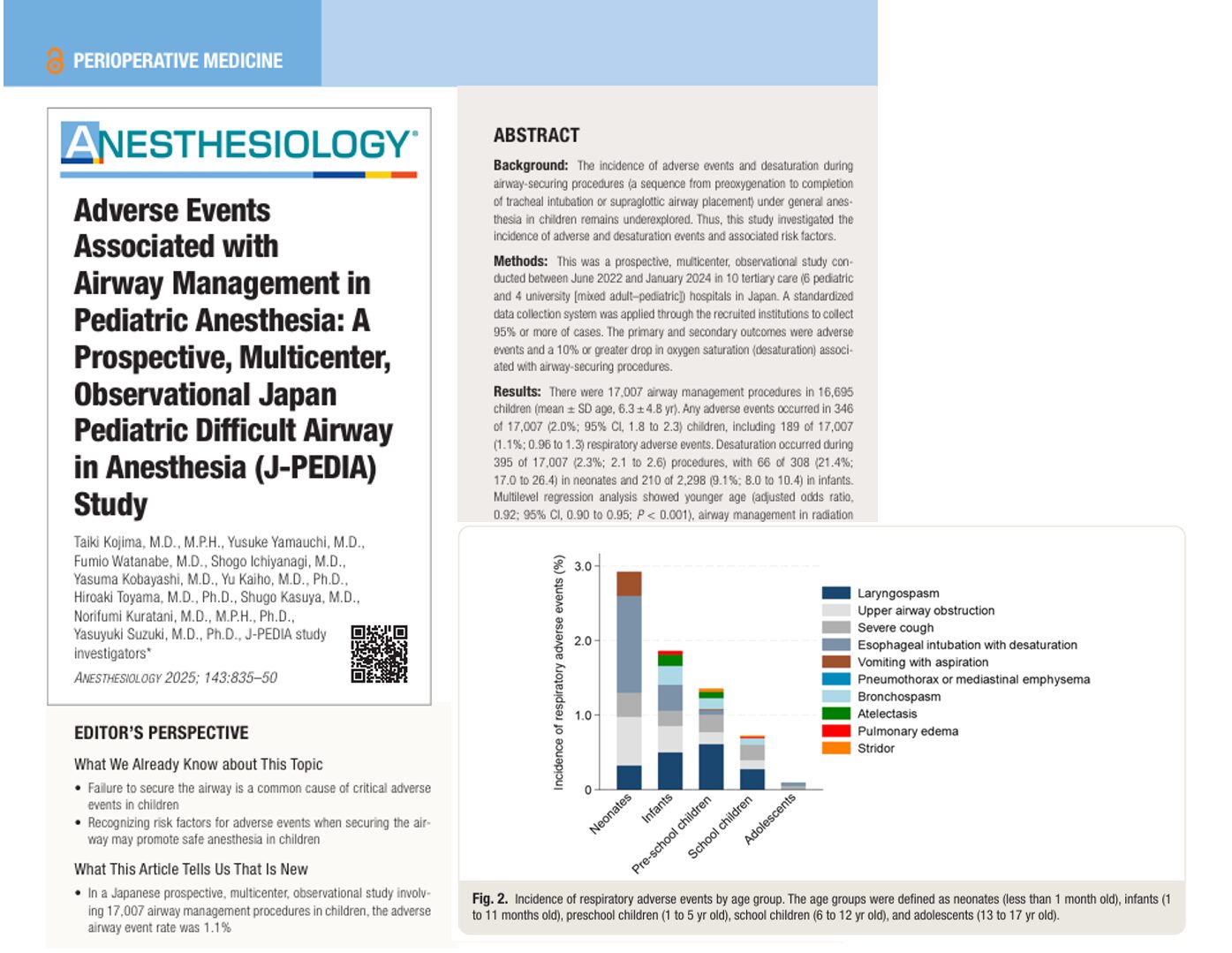
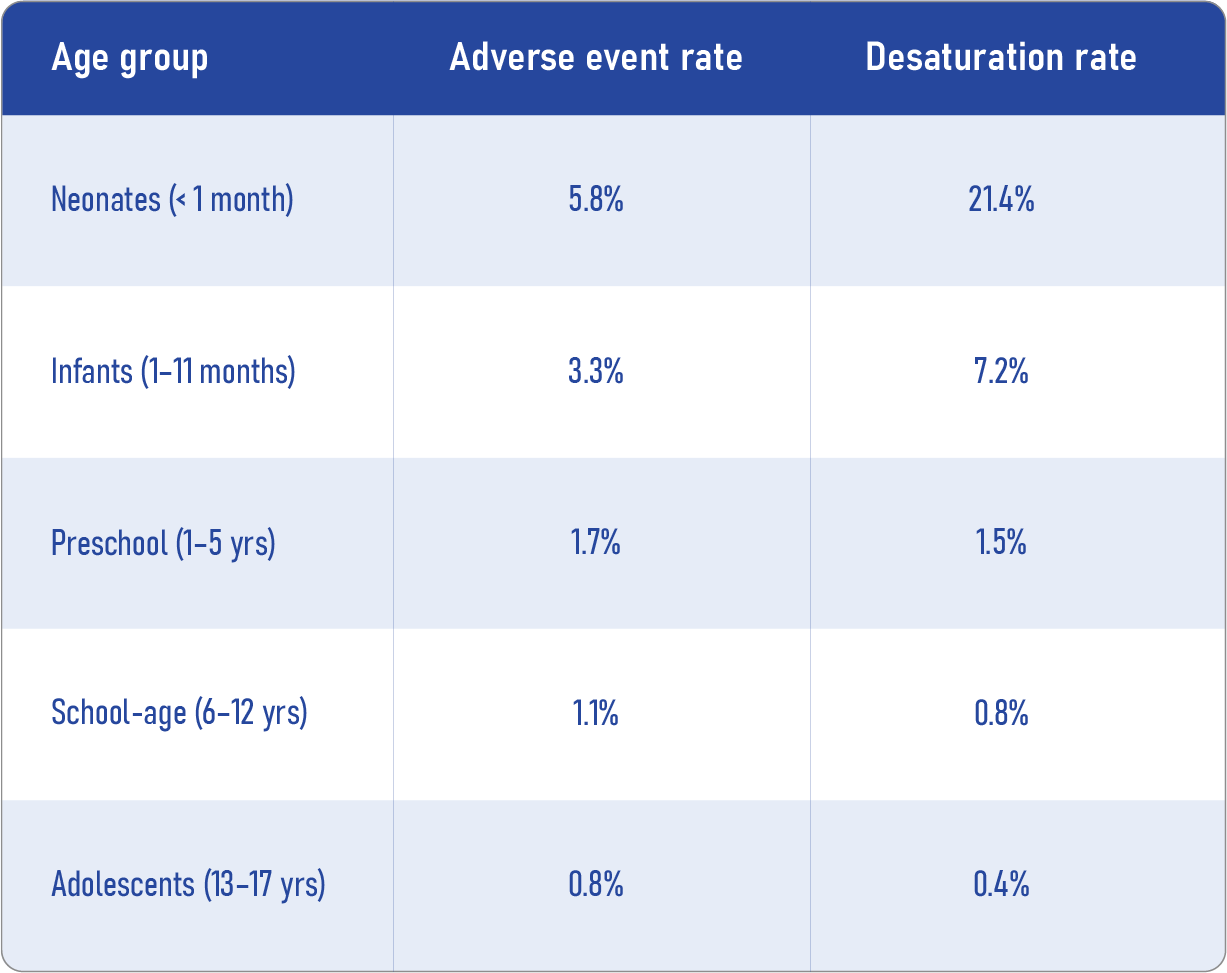
Age-related risk
- Neonates: 5.8% experienced adverse events; 21.4% had desaturation
- Infants: 3.3% experienced adverse events; 7.2% had desaturation
- Risk decreases with age
Medical and procedural risk factors
- Airway sensitivity (URI, asthma)
- Craniocervical surgeries
- Presence of difficult airway features
- Anesthesia in CT/MRI/radiation rooms
What helps reduce the risk?
Some factors were significantly protective:
- Use of supraglottic devices (SGDs) at the first attempt
- Use of muscle relaxants during first attempt
This suggests that strategic planning before airway attempts can mitigate many risks, especially in complex cases.
Step-by-step: Reducing pediatric airway risk
-
Preoperative assessment:
- Screen for anatomical red flags (macroglossia, micrognathia, etc.)
- Identify recent upper respiratory tract infections
- Review allergy and comorbidity history
- Screen for anatomical red flags (macroglossia, micrognathia, etc.)
-
Optimize induction strategy:
- Consider inhalational induction when feasible
- Use muscle relaxants to improve intubation conditions
- Consider inhalational induction when feasible
-
Choose the right device:
- For non-critical cases, SGDs may be safer than tracheal intubation
- Video laryngoscopy may offer benefits, though findings were mixed
- For non-critical cases, SGDs may be safer than tracheal intubation
-
Have backup plans:
- Prepare for difficult mask ventilation
- Ensure availability of alternative airway devices and experienced providers
- Prepare for difficult mask ventilation
-
Monitor and respond early:
- Use pulse oximetry
- Be ready for positive pressure ventilation or bronchodilators if needed
- Use pulse oximetry
Important numbers from the study
Clinical implications
The J-PEDIA study offers data-driven guidance for managing pediatric airways, particularly in Asian populations. It emphasizes that early recognition, tailored equipment use, and provider training are key to reducing complications.
Future directions:
- Develop risk stratification tools
- Expand studies to include emergency room and ICU settings
- Compare data across global regions to refine universal best practices
Conclusion
The J-PEDIA study confirms that adverse events during pediatric airway management are relatively rare but predictable. By identifying high-risk scenarios and applying evidence-based interventions, anesthesiologists can significantly improve outcomes and ensure safer surgical experiences for children.
This research not only adds valuable insights for the medical community in Japan but sets a benchmark for pediatric airway safety worldwide.
Reference: Kojima T et al. Adverse Events Associated with Airway Management in Pediatric Anesthesia: A Prospective, Multicenter, Observational Japan Pediatric Difficult Airway in Anesthesia (J-PEDIA) Study. Anesthesiology. 2025;143:835-850.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant App. Prefer a physical copy? Get the latest literature and guidelines in book format. For an interactive digital experience, check out the Anesthesia Updates Module on NYSORA360!