Learning objectives
- Describe the risk factors for PMI
- Give prophylactic treatment to high-risk patients
- Manage PMI cases
Definition & mechanisms
- Postoperative myocardial injury/infarction (PMI) is a common complication after non-cardiac surgery
- PMI is defined as the increase of troponin caused by ischemia within 30 days after surgery
Pathophysiology
- Type I MI: plaque destruction followed by coronary atherosclerotic thrombosis
- Type II MI: Imbalance in myocardial oxygen supply and demand resulting in ischemia
Risk factors
| Patient-specific | Previous coronary artery disease |
| Age >70 years | |
| Female sex | |
| Renal failure | |
| Diabetes | |
| Peripheral artery disease | |
| Emergency or redo surgery | |
| Severe LV dysfunction (LVEF<35%) or cardiogenic shock | |
| Intraoperative | Open surgery |
| Prolonged intraoperative time with hypotension | |
| Intraoperative heart rate of >110 or <55 BPM | |
| Tachycardia | |
| Intraoperative transfusions | |
| Perioperative vasopressors | |
| Postoperative | Postoperative bleeding |
| Sepsis | |
| Hypoxia | |
| Sustained tachycardia | |
| Hypotension | |
| Severe anemia |
Prophylaxis
- β-adrenergic blockers
- Calcium channel blockers
- α2 agonists
- Statins
- Aspirin
- Coronary revascularization (requires further investigation)
- Anemia corrections
Management
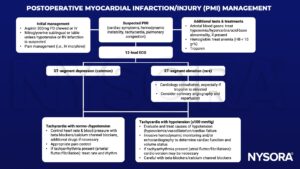
Keep in mind
- Careful perioperative monitoring for ischemia, a low threshold for treating and preventing tachycardia while avoiding hypotension, decreased cardiac output, and/or cardiac decompensation help prevent PMI
- Coronary intervention is rarely indicated as the first line of treatment
- Antithrombotic therapy may exacerbate bleeding
Suggested reading
- Gao L, Chen L, He J, et al. Perioperative Myocardial Injury/Infarction After Non-cardiac Surgery in Elderly Patients. Front Cardiovasc Med. 2022;9:910879.
- Landesberg G, Beattie WS, Mosseri M, Jaffe AS, Alpert JS. Perioperative myocardial infarction. Circulation. 2009;119(22):2936-2944.
- Nashef S., Roques F., Michel P., et al. European system for cardiac operative risk evaluation. Eur J Cardiothorac Surg 1999; 16:9-13
We would love to hear from you. If you should detect any errors, email us at [email protected]