Learning objectives
- Definition of epilepsy
- Anesthetic management of epilepsy
Definition and mechanisms
- Epilepsy is a central nervous system (neurological) disorder in which brain activity becomes abnormal, causing seizures or periods of unusual behavior, sensations, and sometimes loss of awareness
- It is characterized by recurrent (2 or more) seizures which means that having a single seizure does not mean that a patient also has epilepsy
- Normal regulatory functions are altered in epileptogenic disorders
- The standard treatment for adults with epilepsy is antiepileptic drug (AED) therapy
- Approximately 20–30% of patients remain refractory to drug therapy or develop intolerable side effects and resective surgery may be considered
- Epilepsy occurs in approximately 1 in 200 of the general population
Sign and symptoms
- Seizures
- Temporary confusion
- A staring spell
- Stiff muscles
- Uncontrollable jerking movements of the arms and legs
- Loss of consciousness or awareness
- Psychological symptoms such as fear, anxiety, or deja vu
Classification
- Generalized epilepsy
- Tonic-clonic
- Absence
- Myoclonic
- Clonic
- Tonic
- Atonic
- Focal seizures
- Simple
- Complex
- Evolving to generalized
- Mixed seizures (focal and generalized)
- Unclassified
Causes
- Most cases are idiopathic and a definite cause is only found in 25%–35%
- Specific causes include:
- Genetic: juvenile myoclonic epilepsy
- Trauma: depressed skull fractures or intracranial hemorrhage
- Tumors: particularly slow-growing frontal tumors
- Infection: meningitis or encephalitis
- Cerebrovascular disease: 6%–15% of stroke patients
- Alcohol: lowers the seizure threshold
- Others: dementia, multiple sclerosis, metabolic disorders
Risk factors
- Young or older age
- Familial history
- Head injury
- Stroke and other vascular diseases
- Dementia
- Infection (e.g. meningitis)
- Seizures in childhood
Complications
- Status epilepticus
- Sudden unexpected death in epilepsy
Diagnosis
- At least two unprovoked (or reflex) seizures occurring more than 24 hours apart
- One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years
- Witnessed seizures
- Tests:
- EEG
- CT, MRI
- Blood glucose
- ECG
Anti-epileptic agents
- The aim is to achieve a seizure-free patient with minimal drug-related side-effects
- Consider the seizure type and history, patient age, and side effects to choose the correct anticonvulsant
- Monotherapy will control seizures in many patients but some require the addition of second or third-line agents
Agent Side-effects
Phenytoin Skin rash, drowsiness, ataxia, slurred speech, gingival hypertrophy, excess hair growth, anemias, neuropathy
Sodium Valproate Tremor, drowsiness, weight gain, alopecia, raised hepatic transaminase, thrombocytopenia
Carbamazepine Rash, double vision, ataxia, hyponatremia, thrombocytopenia
Phenobarbitone Drowsiness, rash, osteomalacia, anaemia, folate deficiency
Ethosuximide Nausea, drowsiness, anorexia, photophobia
Lamotrigine Rash, drowsiness, double vision, headache, insomnia, tremor, flu-like symptoms
Levetiracetam Dizziness, drowsiness, insomnia, ataxia, tremor, headache, behavioral problems
Primidone Nausea, nystagmus, sedation, anemias, ataxia
Vigabatrin Visual field defects, drowsiness, psychotic reactions
Gabapentin Drowsiness, dizziness, headache
Clobazam Drowsiness, tolerance
Management
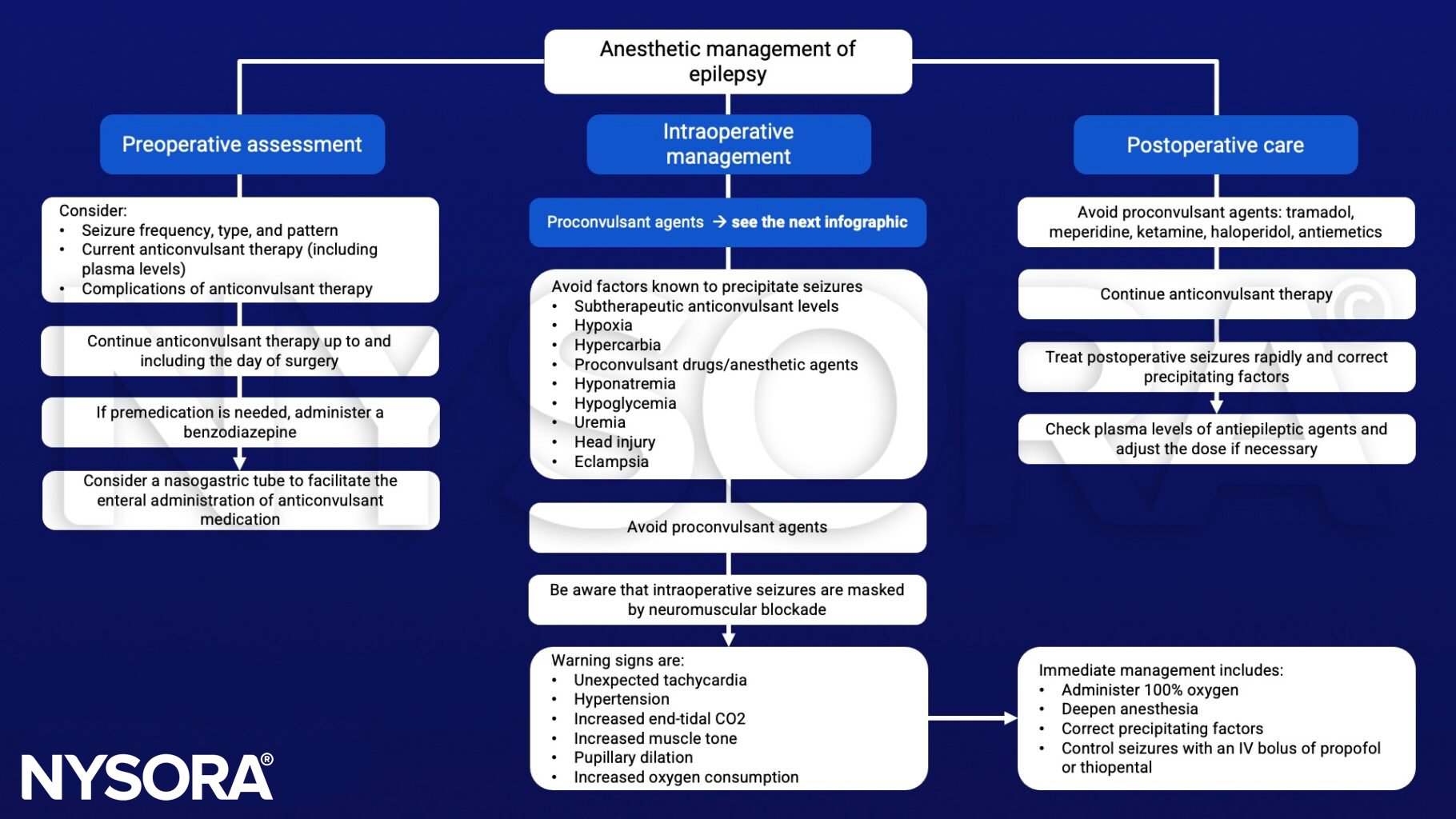
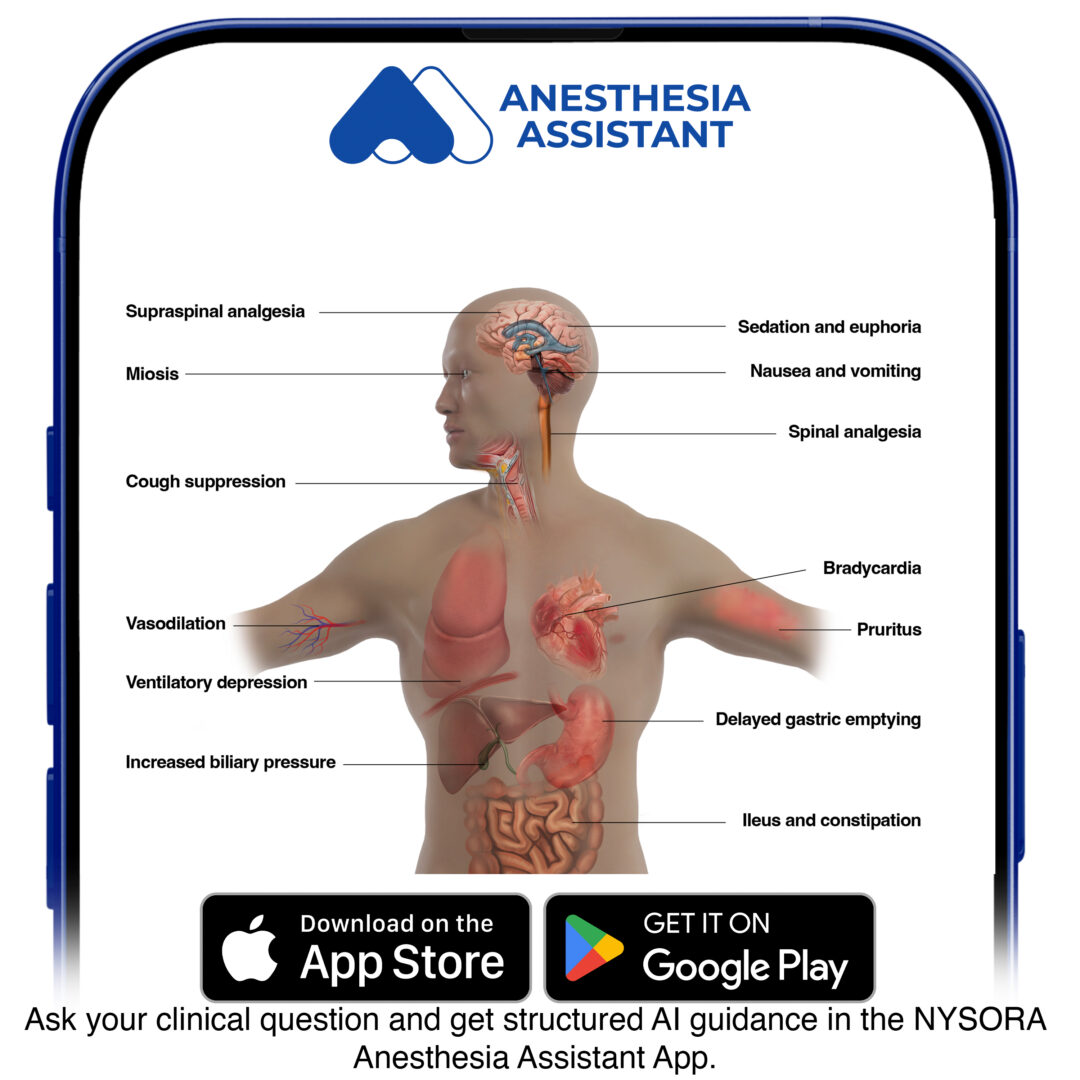
Interactions between antiepileptic and anesthetic agents
![]()
Suggested reading
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Carter, E.L., Adapa, R.M., 2015. Adult epilepsy and anaesthesia. BJA Education 15, 111–117.
Clinical updates
Jacobwitz et al. (Neurocritical Care, 2024) report that in children and neonates with refractory status epilepticus, ketamine used as the first-line anesthetic infusion achieved seizure termination more frequently than midazolam (61% vs 28%) and was associated with significantly fewer adverse effects (3% vs 24%), even after multivariable adjustment. These findings suggest ketamine may be a more effective and better-tolerated initial anesthetic option for pediatric RSE, although survival to discharge remained higher in the midazolam group, reflecting underlying disease severity rather than drug-related mortality.
Rossetti et al. (Intensive Care Medicine, 2024) provide an updated, comprehensive review emphasizing that refractory and super-refractory status epilepticus require early ICU admission, continuous EEG monitoring, and protocolized escalation from benzodiazepines to non-sedating antiseizure medications and anesthetic infusions. The authors highlight ketamine as an important adjunct or alternative in refractory cases due to its NMDA antagonism and relative hemodynamic stability, with mortality rising stepwise from ~10% in responsive SE to nearly 40% in super-refractory SE, underscoring the prognostic importance of early seizure control and etiology-directed therapy.