Learning objectives
- Define and recognize aortic stenosis
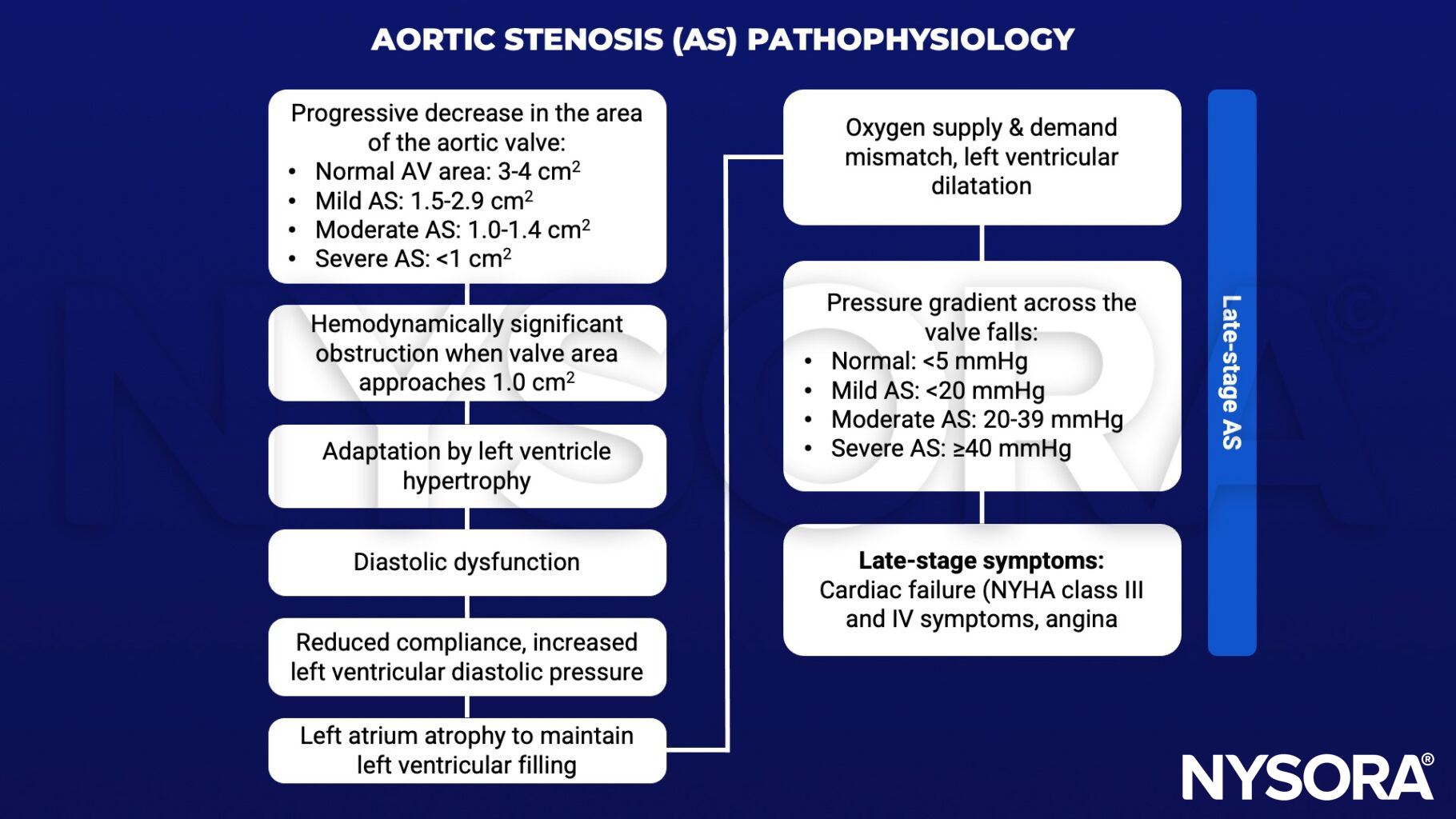
- Describe the pathophysiology of aortic stenosis and its consequences
- Describe the general anesthetic management principles for aortic stenosis
Definition & mechanisms
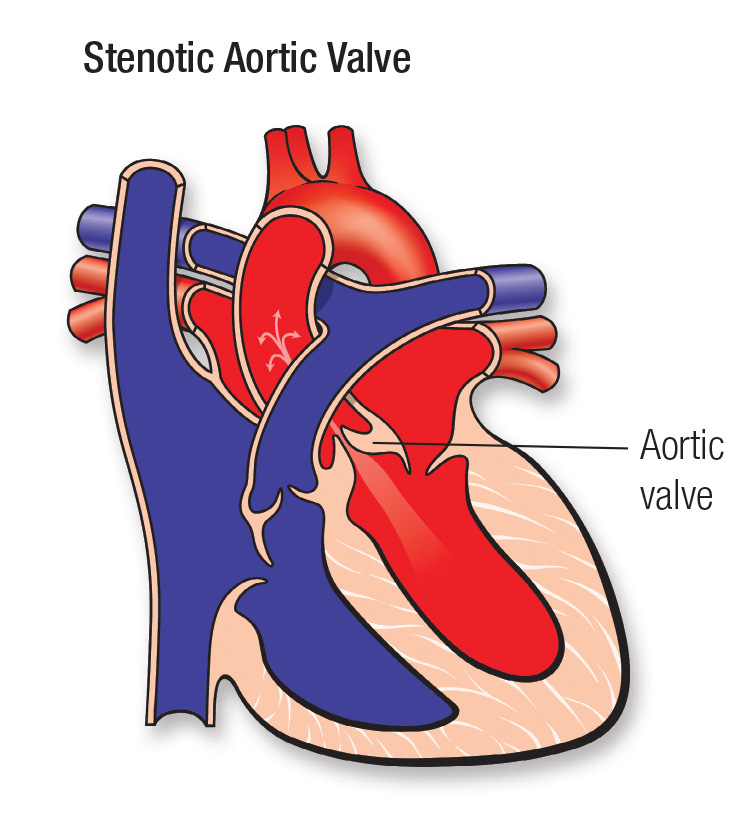
- Aortic stenosis occurs when the aortic valve narrows and blood cannot flow normally
- Severe aortic stenosis is a risk factor for perioperative cardiac complications in non-cardiac surgery
- There are several causal mechanisms:
- Degenerative calcific aortic stenosis: Progressive fibrosis and calcification due to mechanical stress over time
- Congenital bicuspid aortic valve: Abnormal valve structure, with two rather than three leaflets, which can produce fibrosis and calcifications
- Rheumatic aortic stenosis: Long-term consequence of acute rheumatic fever
Severity assessment
| Aortic sclerosis | Mild | Moderate | Severe | |
|---|---|---|---|---|
| Peak velocity (m/s) | <_2.5 m/s | 2.6–2.9 | 3.0–4.0 | ≥4.0 |
| Mean gradient (mmHg) | - | <20 | 20–40 | ≥40 |
| AVA (cm2) | - | >1.5 | 1.0–1.5 | <1.0 |
| Indexed AVA (cm2 /m2) | - | >0.85 | 0.60–0.85 | <0.6 |
| Velocity ratio | - | >0.50 | 0.25–0.50 | <0.25 |
Anesthetic management
- The severity and pathophysiology of aortic stenosis determine the anesthetic management plan
- The following general principles apply:
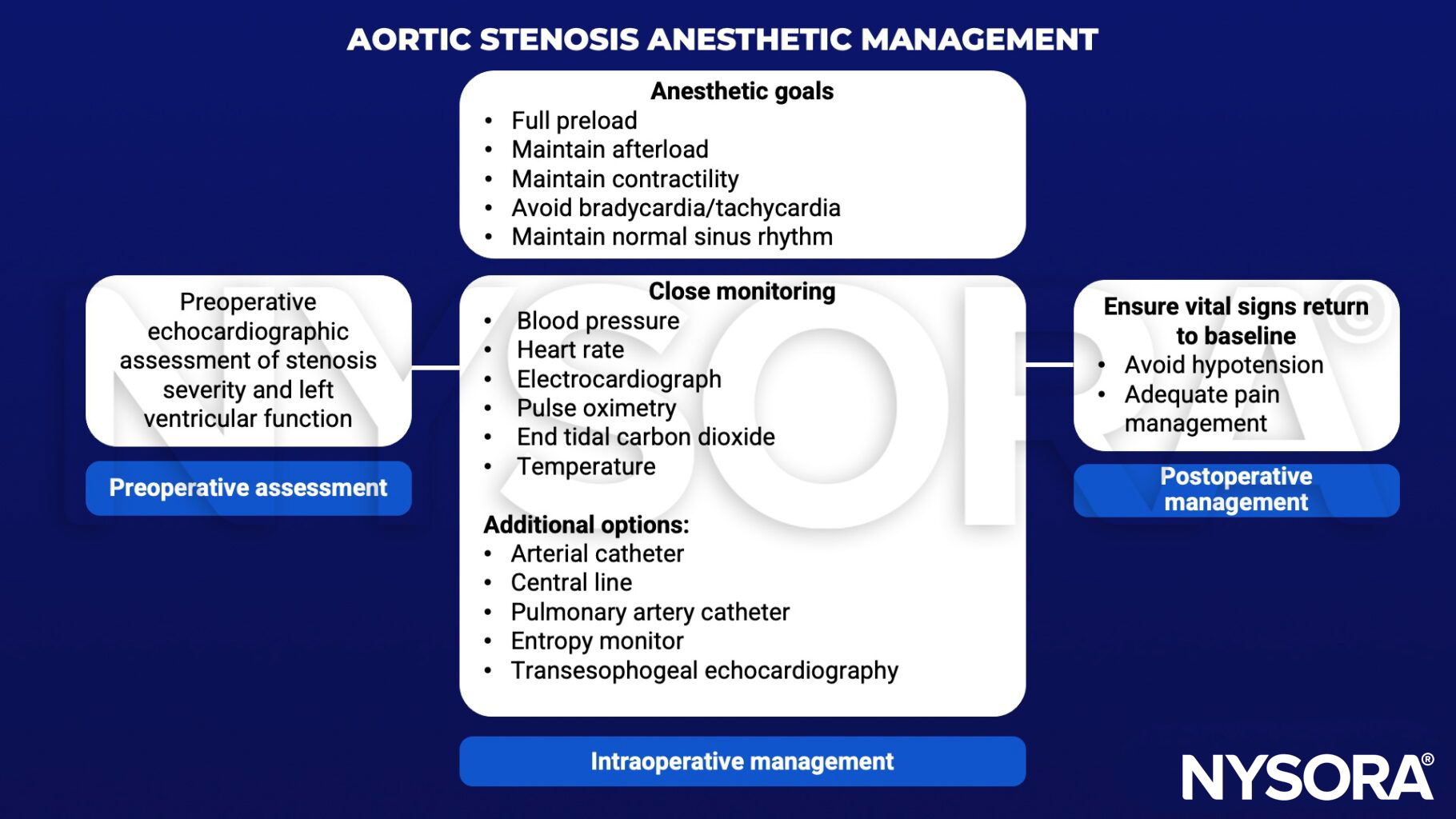
Keep in mind
- All necessary medications and equipment to ensure stable vital signals and treat irregularities must be available during the procedure
Suggested reading
- Schneider AC. A review of aortic stenosis: an anesthetic perspective. J Anesth Crit Care Open Access. 2018;10(6):262‒264.
- Baumgartner H Chair, Hung J Co-Chair, Bermejo J, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2017;18(3):254-275.
- Brown J, Morgan-Hughes NJ. Aortic stenosis and non-cardiac surgery. Continuing Education in Anaesthesia Critical Care & Pain. 2005;5(1):1-4.
Clinical updates
Van Herreweghe et al. (RAPM, 2025) report a retrospective series of 35 patients with moderate or severe aortic stenosis undergoing lower-limb orthopedic surgery under low-dose, isobaric spinal anesthesia. Despite historical concerns, spinal anesthesia was not associated with cardiac arrest, ICU admission, or 30-day mortality; hypotension occurred but was modest, treatable with vasopressors, and not clearly related to AS severity. These findings suggest carefully titrated low-dose spinal anesthesia may be a reasonable alternative to general anesthesia in selected AS patients.
- Read more about the study HERE.
Samadzadeh Tabrizi et al. (J Cardiothorac Vasc Anesth, 2024) systematically reviewed 61 studies that included more than 3,200 patients with aortic stenosis who underwent neuraxial anesthesia for noncardiac, obstetric, or cardiac procedures. Across heterogeneous techniques and severities, hypotension requiring vasopressors was the most common complication, but no intraoperative cardiovascular collapse was reported, and overall 30-day mortality was low. The authors conclude that aortic stenosis should not be considered an absolute contraindication to neuraxial anesthesia, though careful patient selection, invasive monitoring in severe/symptomatic disease, and prospective comparative trials remain needed.
- Read more about the study HERE.