Learning objectives
- Describe the pathophysiology and symptoms of croup
- Diagnose croup and assess its severity
- Manage patients presenting with croup
Background
- Laryngotracheobronchitis or croup refers to inflammation of the larynx, trachea, and bronchi
- Common cause of cough, stridor, and hoarseness in children with a fever
- Most children experiencing croup recover without complications
- Rarely, croup can be lethal to infants
- Most often caused by a viral infection (parainfluenza, RSV, rhinovirus, enterovirus, influenza, adenovirus)
- More common in boys compared to girls
Pathophysiology
- Inhalation of virus infecting nasal and pharyngeal mucosal epithelia, further spreading to the subglottic space
- In children, the subglottic space is the most narrow part of the airway
- The inability of the cricoid to expand causes significant narrowing subglottic region secondary to the inflamed mucosa
- When the patient cries or becomes agitated, further dynamic obstruction can occur
Signs & symptoms
- Usually history of 1-3 days of rhinorrhea, nasal congestion, and fever
- Barky or seal-like cough
- Hoarse voice
- High-pitched inspiratory stridor
- Wheezing
- Crackles
- Air trapping
- Tachypnea
- Cyanosis
Diagnosis
- Mostly clinical diagnosis
- Abrupt onset of barky cough, stridor, and hoarseness
- Often dyspnea and fever
- Overt inspiratory stridor in the neck on auscultation
- Steeple sign on radiography (usually not necessary)
- Laboratory studies are rarely needed
- Laryngoscopy when alternate diagnoses are suspected (perform with caution when epiglottitis is suspected)
Differential diagnosis
| Condition | Typical age range | Clinical presentation | Diagnostic tests |
|---|---|---|---|
| Croup | 6 months to 3 years | Acute onset of barking cough, stridor, and hoarseness | None required |
| Bacterial tracheitis | <6 years | High fever, barking cough, respiratory distress, and rapid deterioration | Neck radiography (irregular tracheal mucosa) and complete blood count |
| Epiglottitis | 3 to 12 years | Acute onset of dysphagia, odynophagia, drooling, high fever, anxiety, and muffled voice | Neck radiography (thickened epiglottis) and complete blood count |
| Foreign bodyaspiration | <3 years | Acute onset of choking and/or drooling | Acute onset of choking and/or drooling |
| Hemangioma | <6 months | Stridor worse with crying | Airway endoscopy |
| Large airway lesions (subglottic stenosis, laryngeal cleft, tracheomalacia, laryngomalacia) | <6 months to 4.5 years | Recurrent episodes of barking cough and stridor | Airway endoscopy |
| Neoplasm | No age predilection | Progressive airway symptoms | Lateral neck radiography and CT |
| Peritonsillar abscess | 6 months to 3.5 years | Sore throat, fever, “hot potato” voice | Neck radiography, neck CT, and complete blood count |
| Retropharyngeal abscess | 2 to 4 years | Fever, drooling, dysphagia, odynophagia, and neck pain | Neck radiography (bulging posterior pharyngeal wall), neck CT, and CBC |
| Thermal injury/smoke inhalation | No age predilection | Exposure to heat, smoke, or chemical | Direct laryngoscopy |
Severity scoring
Westley Croup Score:
| Clinical sign | Score | |
|---|---|---|
| Level of consciousness | Normal (including sleep) | 0 |
| Disoriented | 5 | |
| Cyanosis | None | 0 |
| With agitation | 4 | |
| At rest | 5 | |
| Stridor | None | 0 |
| When agitated | 1 | |
| At rest | 2 | |
| Air entry | Normal | 0 |
| Decreased | 1 | |
| Markedly decreased | 2 | |
| Retractions | None | 0 |
| Mild | 1 | |
| Moderate | 2 | |
| Severe | 3 |
Total score:
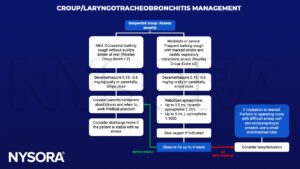
- ≤2: Mild
- 3 – 7: Moderate
- 8 – 11: Severe
- ≥12: Impending respiratory failure
Complications
- Hospitalization
- Secondary bacterial infection
- Pneumothorax
- Otitis media
- Dehydration
- Lymphadenitis
Management
Suggested reading
- Ernest S, Khandhar PB. Laryngotracheobronchitis. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519531/
- Smith DK, McDermott AJ, Sullivan JF. Croup: Diagnosis and Management. Am Fam Physician. 2018;97(9):575-580.
- Maloney E, Meakin GH. Acute stridor in children. Continuing Education in Anaesthesia Critical Care & Pain. 2007;7(6):183-6.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com