Learning objectives
- Describe diabetes insipidus
- Recognize the symptoms and signs of diabetes insipidus
- Anesthetic management of a patient with diabetes insipidus
Definition and mechanisms
- Diabetes insipidus (DI) is a disorder of urinary concentration caused by a temporary or chronic deficiency of or insensitivity to antidiuretic hormone (ADH) or vasopressin
- The condition renders the kidneys unable to effectively autoregulate water balance, resulting in polyuria, polydipsia, and electrolyte abnormalities (e.g., hypernatremia, hypokalemia)
Classification
- Central DI or ADH deficiency: Reduced ADP secretion due to damage to the pituitary gland or hypothalamus or genetics
- Nephrogenic DI or ADH resistance: Normal ADP secretion, but the kidneys are unable to properly respond to ADH due to an inherited genetic disorder or chronic kidney disorder
- Gestational DI: A very rare condition that occurs during pregnancy when an enzyme made by the placenta destroys ADH
- Primary polydipsia (dipsogenic DI): Damage to the hypothalamic thirst center causes excessive fluid intake leading to polyuria
Signs and symptoms
| Adults | Children | Infants |
|---|---|---|
| Polyuria Polydipsia Nocturia Craving for ice water | Anorexia Growth defects Enuresis Sleep disturbance Fatigue | Irritability Chronic dehydration Growth retardation Neurologic disturbance Hyperthermia |
Clinical findings
- If the thirst mechanism is intact: Hydronephrosis and distended bladder due to excessive urinary volume
- If there is no access to free water or damage to the hypothalamic thirst center: Hypernatremia, dehydration, hypertonic encephalopathy, obtundation, coma, seizure, subarachnoid hemorrhage, and intracerebral hemorrhage
Complications
Dehydration, which may cause:
- Dry mouth
- Changes in skin elasticity
- Thirst
- Fatigue
Electrolyte imbalance, resulting in:
- Weakness
- Nausea
- Vomiting
- Loss of appetite
- Muscle cramps
- Confusion
Pathophysiology
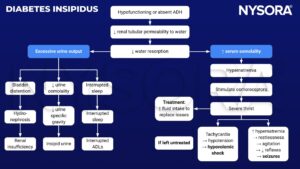
Treatment
There is no cure → treatments aim to relieve thirst, decrease urine output, and prevent dehydration
- Central and gestational DI: Desmopressin (DDAVP)
- Nephrogenic DI: Treat the underlying cause or use a thiazide, aspirin, or ibuprofen
- Primary polydipsia: Decrease fluid intake
Management
- Hypernatremia: ↑ MAC requirements
- Treat hypernatremia by estimating water deficit and replacing it with free water:
- Water deficit = total body water x (Serum Na [ ]/140-1)
- Volume depletion: Resuscitate with normal saline initially
- Central DI: DDAVP 1-2 mcg i.v. BID
- Nephrogenic DI: Hydrochlorothiazide/amiloride
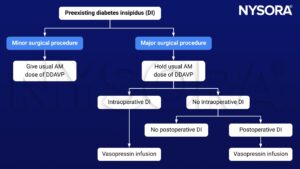
Keep in mind
- Avoid rapid overcorrection if chronic hypernatremia (goal = <10 mEq/day)
- Be careful of cerebral edema, water intoxication, and volume overload
Suggested reading
- Mutter CM, Smith T, Menze O, Zakharia M, Nguyen H. Diabetes Insipidus: Pathogenesis, Diagnosis, and Clinical Management. Cureus. 2021;13(2):e13523.
- Dharshan AC, Kohli-Seth R. Chapter 117. Diabetes Insipidus. In: Atchabahian A, Gupta R. eds. The Anesthesia Guide. McGraw Hill; 2013. Accessed January 17, 2023.
We would love to hear from you. If you should detect any errors, email us [email protected]