Joseph M. Neal and Yavuz Gurkan
INTRODUCTION
Although most upper extremity regional anesthesia is accomplished by means of various approaches to the brachial plexus, there are occasions when individual terminal nerves or their branches are blocked selectively. There are generally three instances in which the anesthesiologist desires to perform these selective nerve blocks. First, some surgical sites are partially innervated by sensory nerves that are not part of the brachial plexus or not consistently anesthetized with plexus blocks. This chapter describes how and when to anesthetize the most common of these nerves—the supraclavicular, the suprascapular, and the intercostobrachial. The second indication is when the block of the entire brachial plexus block is not necessary for the planned procedure. In this case, selective upper extremity cutaneous anesthesia or analgesia may involve blocking terminal nerves (radial, median, or ulnar nerves) or their branches (lateral and medial antebrachial cutaneous nerves) distally at the elbow. A final and controversial indication for selective upper extremity nerve blocks is their use as a supplement to an incomplete brachial plexus block.
When considering the application of these various blocks, the reader is reminded that innervation of the upper extremity is often variable and overlapping. Therefore, when faced with the choice of performing a single nerve block versus blocking several adjacent nerves, it is advisable to err on the side of multiple blocks, particularly in those adjacent cutaneous areas that represent potential crossover innervation (Figures 1 and 2). The relevant anatomy will be covered with specific nerve block description.
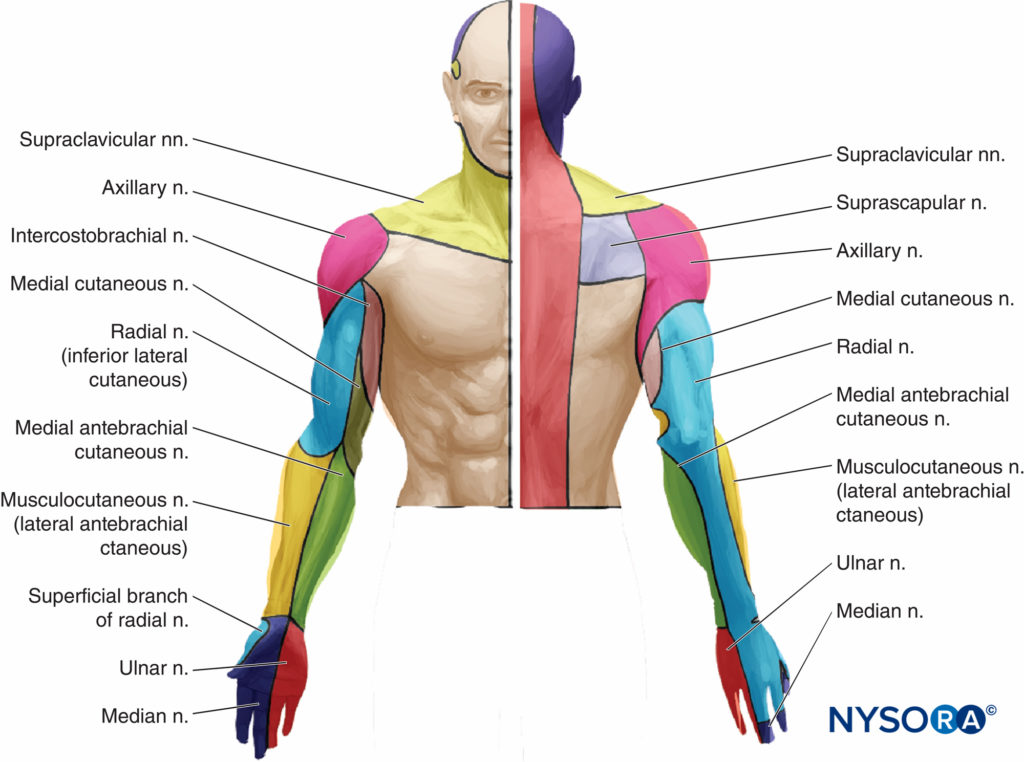
FIGURE 1. Cutaneous innervation of the upper extremity. Actual patients demonstrate large variation in the depicted pattern of innervation and significant crossover between nerves.
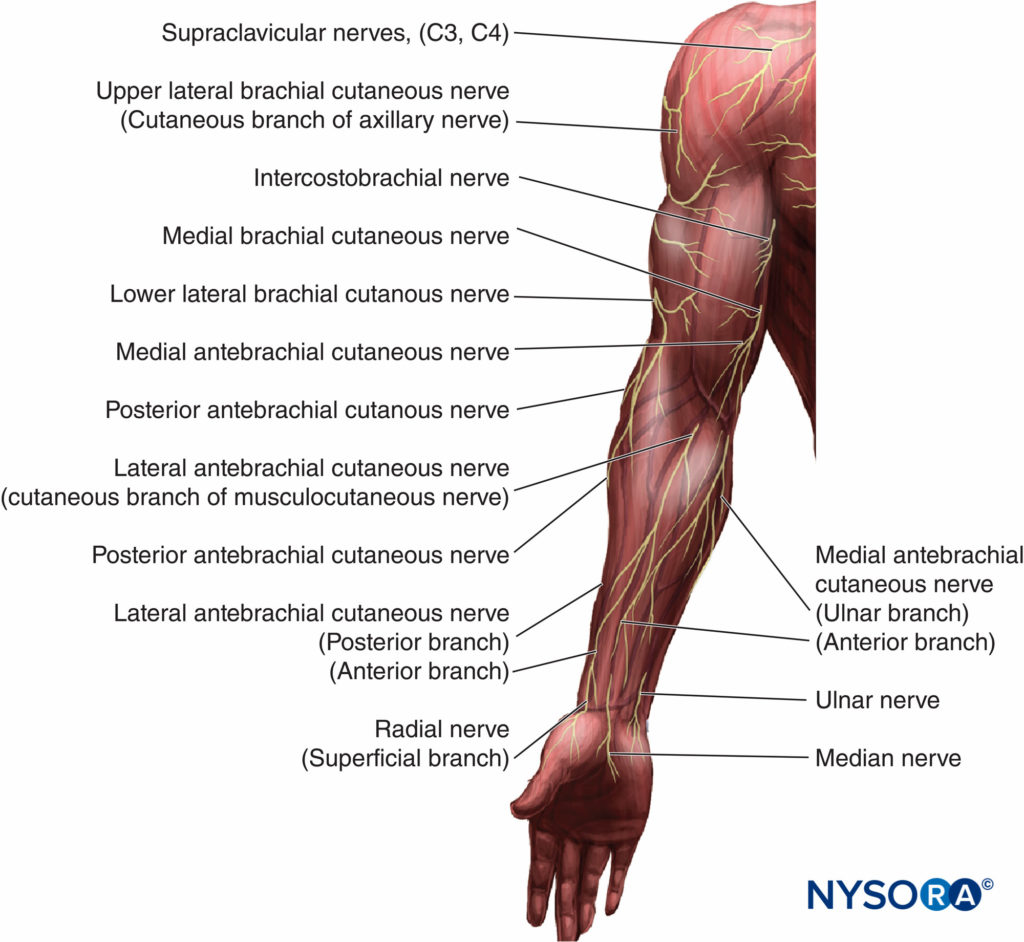
FIGURE 2. Idealized distribution of the cutaneous innervation of the upper arm and forearm.
Local Anesthetic and Adjuvant Selection
Local anesthetics for individual upper extremity nerve blocks are selected for their desired duration of anesthesia and/or analgesia. If intermediate-acting local anesthetics are selected (lidocaine or mepivacaine), the duration can be increased with either adjuvant epinephrine (2.5 mcg/mL). Neither adjuvant significantly increases duration if a long-acting local anesthetic such as bupivacaine or ropivacaine is chosen.
SUPRACLAVICULAR NERVE BLOCK INDICATIONS
The supraclavicular nerve provides sensory innervation to the “cape” of the shoulder (Figure 3). Commonly anesthetized as a component of cervical plexus block for carotid surgery, the supraclavicular nerve may also require block for surgery involving the shoulder or supraclavicular area. Local anesthetic spread in an interscalene plexus block often blocks the cervical plexus and therefore it is adequate to block the supraclavicular nerve, but the nerve is frequently not anesthetized with a supraclavicular brachial plexus block.
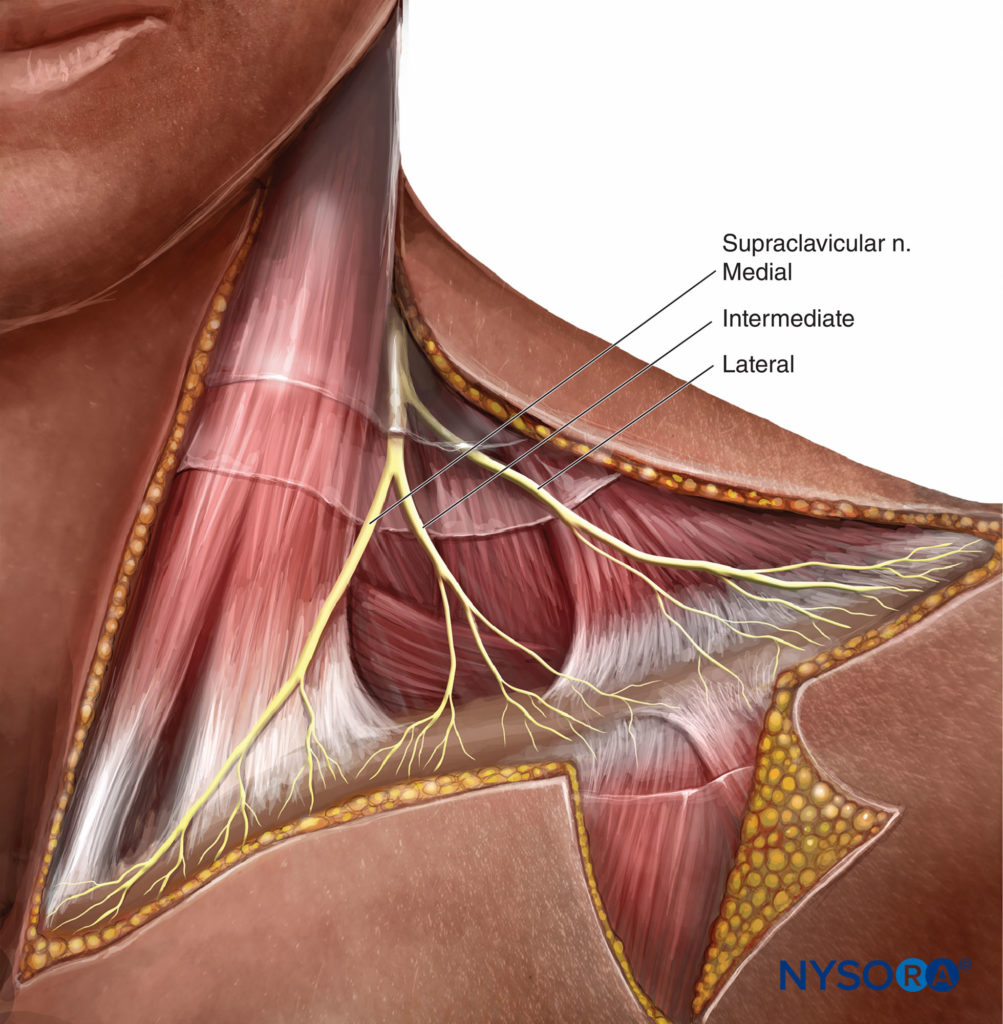
FIGURE 3. Supraclavicular nerves, derived from C3–C4 nerve roots, is not part of the brachial plexus, and provides sensory innervation of the shoulder “cape.”
Anatomy
The supraclavicular nerve is derived from the ventral rami of the third and fourth cervical nerve roots (C3–C4); it is thus separate from the brachial plexus. The nerve becomes superficial as it penetrates the mid belly of the sternocleidomastoid muscle, thereafter forming three branches (Figure 3). These branches provide sensory innervation to the cape area, which spans from the midline to the deltoids, and from the second rib anteriorly to the top of the scapula posteriorly.
Technique
block of the supraclavicular nerve is accomplished with 5–10 mL of an intermediate- or long-acting local anesthetic, depending on analgesic requirements. Three milliliters is deposited with a 22- to 25-gauge sharp needle into the mid belly of the sternocleidomastoid. The remaining local anesthetic is then injected subcutaneously in a cephalad and caudad direction along the posterior border of the sternocleidomastoid.
Complications
Complications of the supraclavicular nerve block are uncommon. The external jugular vein should be avoided to prevent hematoma.
SUPRASCAPULAR NERVE BLOCK
Indications
Suprascapular nerve block (SSNB) can be used as an adjunct to arthroscopic shoulder surgery and total shoulder arthroplasty. When combined with general anesthesia for shoulder arthroscopy, SSNB improves analgesia, reduces opioid-related side effects, and hastens hospital discharge, although SSNB is not superior to interscalene block in this setting. For anterior open shoulder surgery, supplemental SSNB does not affect outcome when combined with interscalene block.
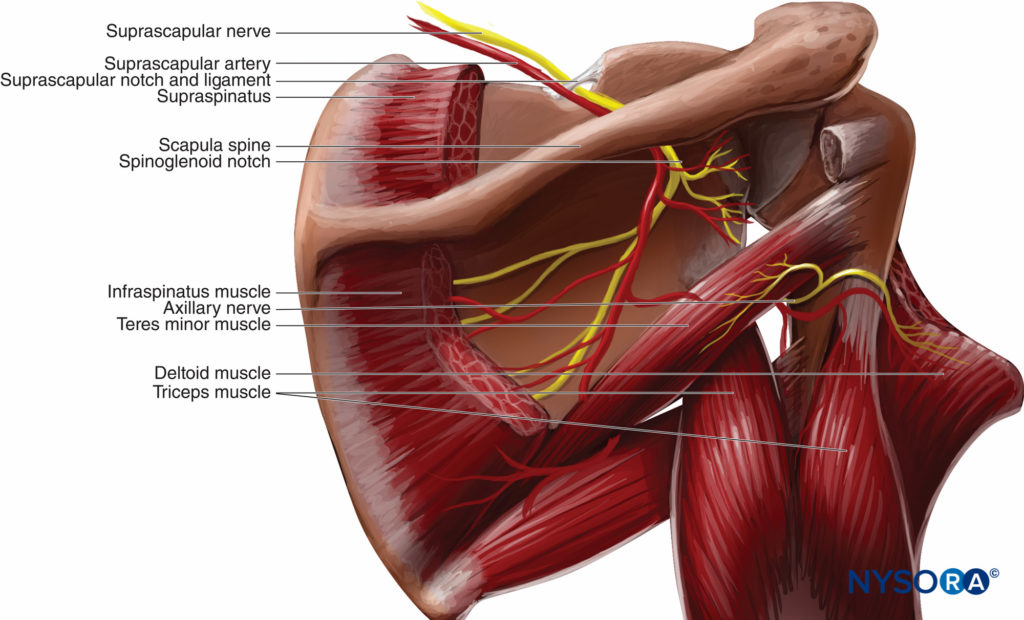
FIGURE 4. Suprascapular nerve block is accomplished by injecting local anesthetic in the suprascapular notch.
Anatomy
The suprascapular nerve (C4–C5) branches from the superior trunk of the brachial plexus and, therefore, it is usually anesthetized by an interscalene block. It traverses the suprascapular notch and continues laterally along the superior border of the scapular spine (Figure 5). The supraclavicular nerve provides sensory innervation to 70% of the posterior-superior shoulder joint, the acromioclavicular joint, and a portion of the anterior axilla in up to 10% of patients. The suprascapular nerve provides motor innervation to the supraspinatus and infraspinatus muscles, but minimal if any cutaneous innervation over the scapula or posterior shoulder.
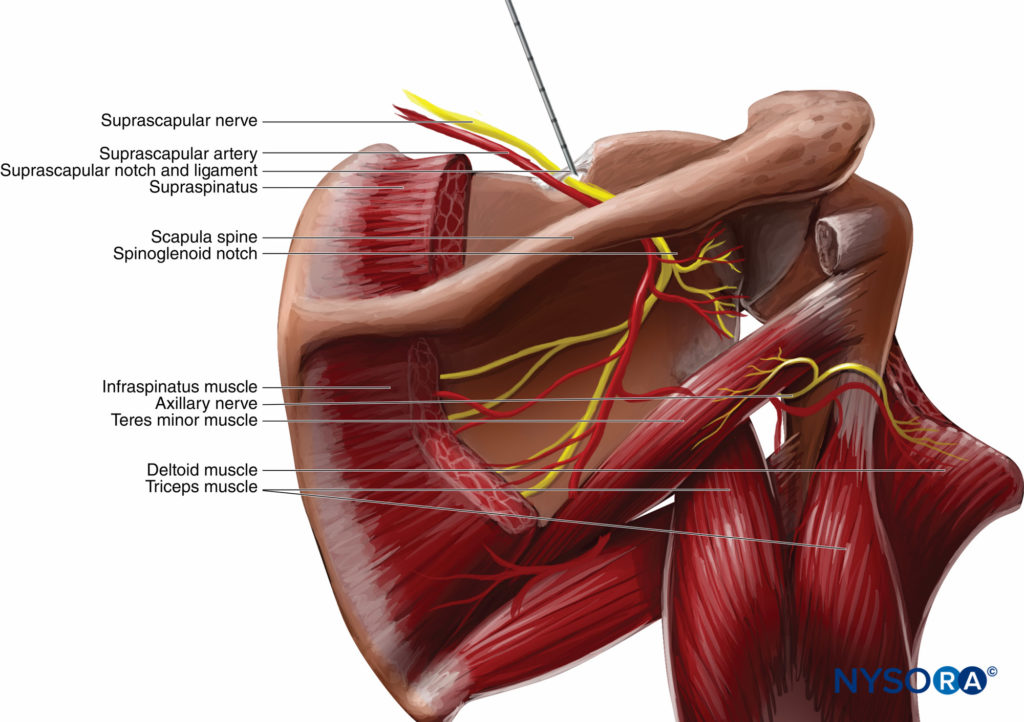
FIGURE 5. Suprascapular nerve block. The suprascapular nerve is blocked as it emerges from the suprascapular notch. Directing the needle caudally substantially reduces the risk of pneumothorax.
Technique
Surface landmarks are identified by drawing one line along the superior border of the scapular spine and then bisecting it with a second line drawn parallel with the vertebral spine. From where these two lines cross, the suprascapular notch underlies a point approximately 2–3 cm toward the middle of the upper/outer quadrant (see Figure 5). A 1.5-in. 22-gauge needle is placed at this entry mark and directed caudad in the sagittal plane until it contacts the scapular spine, followed by injection of 10 mL of a long-acting local anesthetic. If a peripheral nerve stimulator is used, the suprascapular nerve is identified by the motor response of external shoulder rotation.
Complications
Pneumothorax can result from a needle that passes through the suprascapular notch and enters the pleural space. This complication is largely avoidable by directing the needle in a caudad, rather than anterior, direction.
NYSORA Tips
- Suprascapular nerve block is a valuable analgesic adjunct for shoulder arthroscopy performed with the patient under general anesthesia.
- Suprascapular nerve block does not add value to open shoulder procedures in which an interscalene block is the primary anesthetic.
- Suprascapular nerve block is probably a valuable supplement to interscalene block during total shoulder arthroplasty or in the occasional patient who experiences pain at the anterior arthroscopic port site.
INTERCOSTOBRACHIAL NERVE BLOCK
Indications
The intercostobrachial nerve block is indicated for surgery involving the medial/posterior upper arm and/or for anterior arthroscopic port placement. A secondary indication is to alleviate the sensation resulting from a pneumatic tourniquet applied to the upper arm. Despite commonly held misperception, the intercostobrachial nerve block does not block the ischemic, compressive components that cause tourniquet pain; this is accomplished by brachial plexus block with supplemental intraoperative sedation—additional cutaneous anesthesia is not necessary.
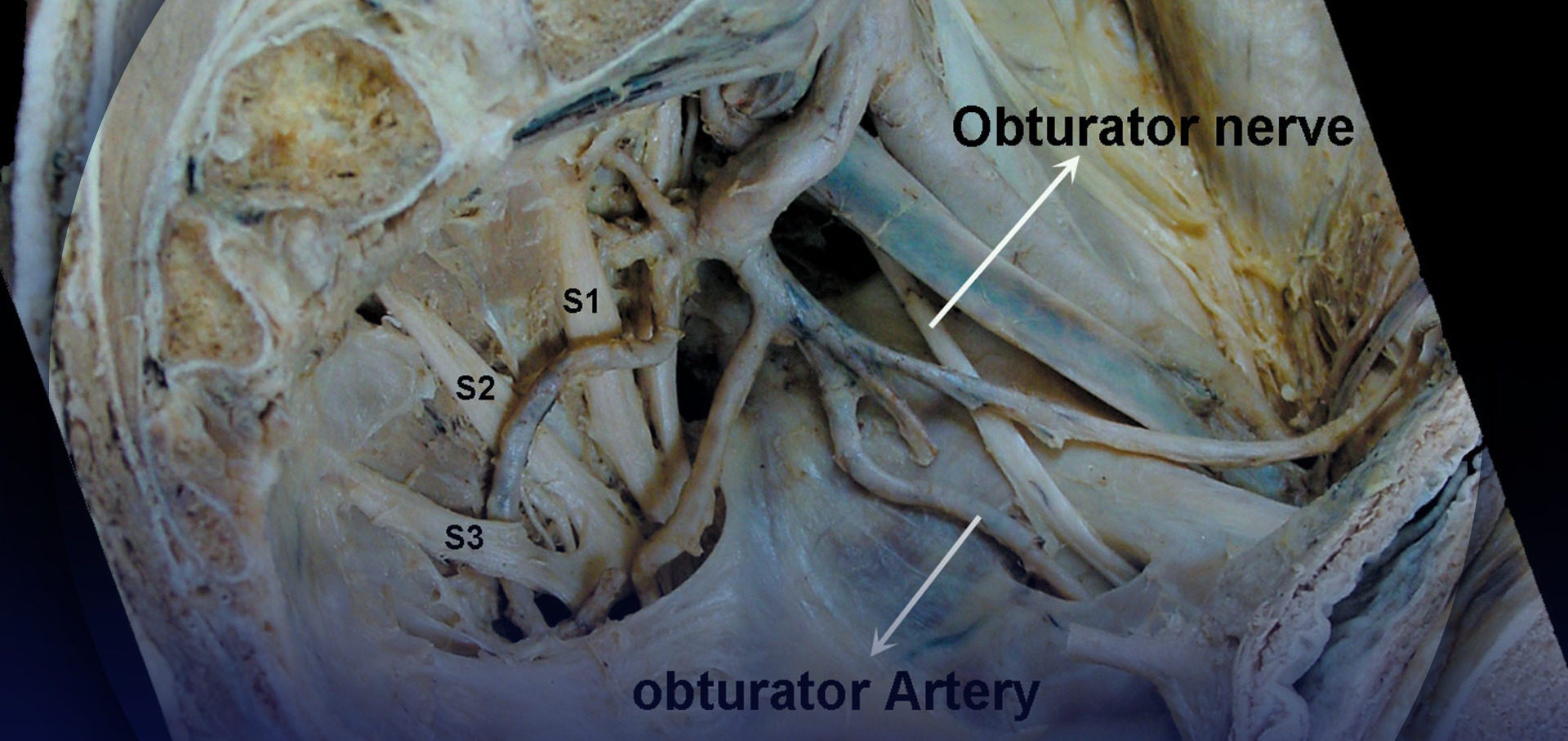
Anatomy
The intercostobrachial nerve arises from the second thoracic (T2 and occasionally T1) nerve root (see Figure 2). As such, it is not a component of the brachial plexus and is, therefore, not anesthetized by any brachial plexus approach. Along with the medial cutaneous nerve of the arm (an intermediary branch of the medial cord), the intercostobrachial nerve provides cutaneous sensation to the upper half of the medial/posterior arm. It also innervates a portion of the anterior axilla (see Figures 1 and 2).
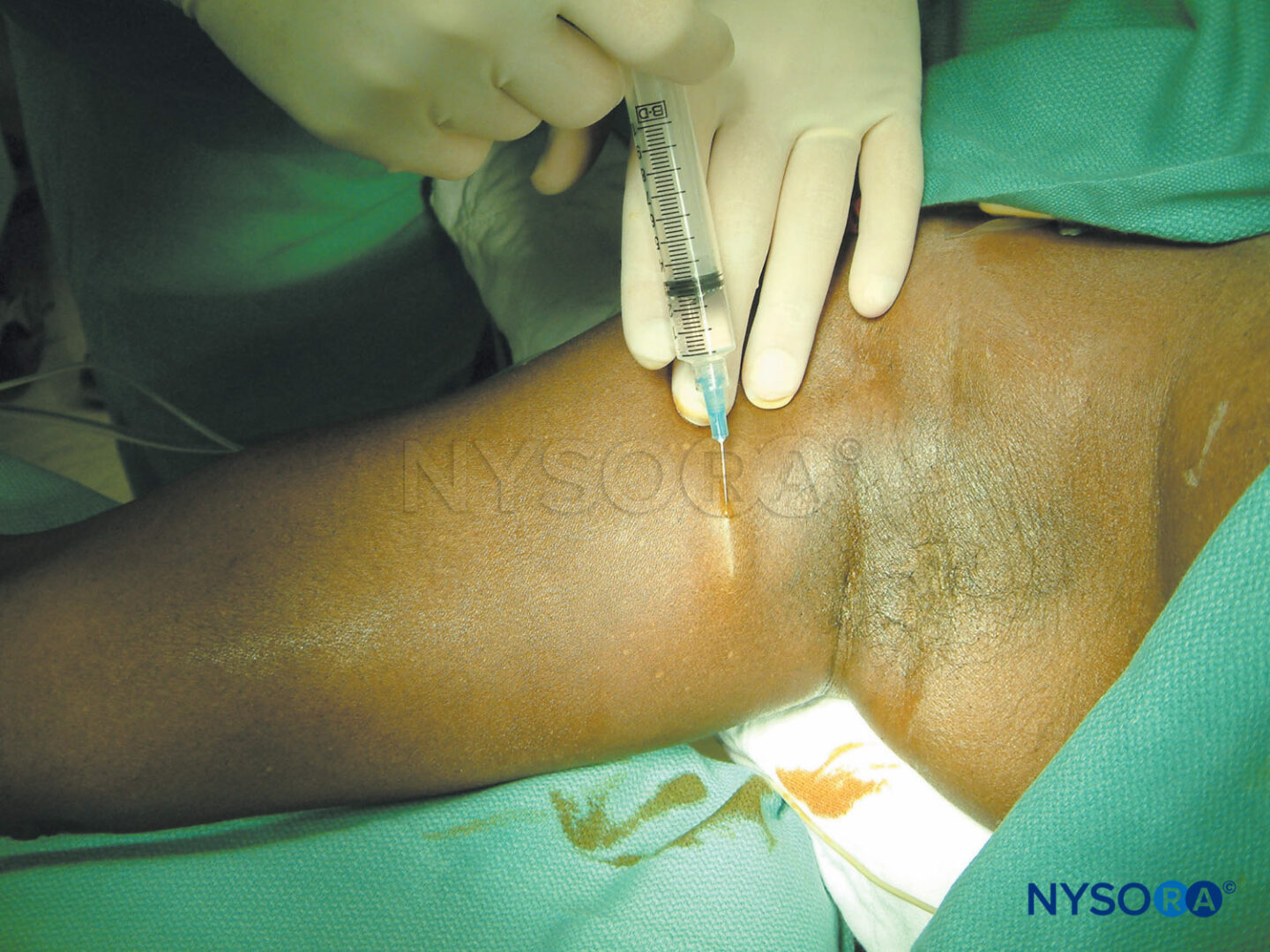
Technique
The intercostobrachial is anesthetized by depositing 5 mL of local anesthetic subcutaneously superiorly and inferiorly along the axillary crease via a 1.5-in. 25-gauge needle (Figure 6).

FIGURE 6. Intercostobrachial nerve block. The intercostobrachial nerve is anesthetized by subcutaneous injection of 3–5 mL local anesthetic along the axillary crease.
Complications
Because of its superficial placement, complications of the intercostobrachial nerve block are virtually nonexistent.
NYSORA Tips
- The intercostobrachial nerve block is a useful supplement to any brachial plexus block when surgery involves the upper medial/posterior arm, a pneumatic tourniquet, and/or an anterior arthroscopic port.
LATERAL AND MEDIAL ANTEBRACHIAL CUTANEOUS NERVE BLOCK
Indications
Local anesthetic block of the lateral and medial antebrachial cutaneous nerves is indicated for superficial surgery of the forearm, such as arteriovenous fistula surgery, or as a supplement to incomplete brachial plexus block.
Anatomy
The lateral antebrachial cutaneous nerve of the forearm (LAC) is the primary cutaneous branch of the musculocutaneous nerve. It provides cutaneous innervation to the lateral (radial) half of the volar forearm. The medial antebrachial cutaneous nerve of the forearm (MAC) is an intermediary branch of the medial cord. It provides cutaneous innervation to the medial (ulnar) half of the volar forearm, an area commonly misperceived as innervated by the ulnar nerve (see Figures 1 and 2).
Technique
Considering the unpredictable overlap of forearm cutaneous innervation, it is advisable to perform both LAC and MAC nerve blocks when forearm anesthesia is desired. Blocking the LAC is accomplished with two local anesthetic injections placed along the intercondylar line. The first 5 mL of local anesthetic is injected just deep to the lateral margin of the biceps tendon; the second 5 mL area injected subcutaneously and lateral from the first injection site, along the elbow crease (Figure 7). The MAC is blocked by injecting a half-ring of 5–7 mL local anesthetic about a quarter of the arm’s length above the medial elbow (Figure 7). When LAC and/or MAC nerve blocks are supplemental to a previous incomplete brachial plexus block, the additional 15–20 mL of local anesthetic should be well tolerated by patients if injected 20–30 minutes after the primary block.
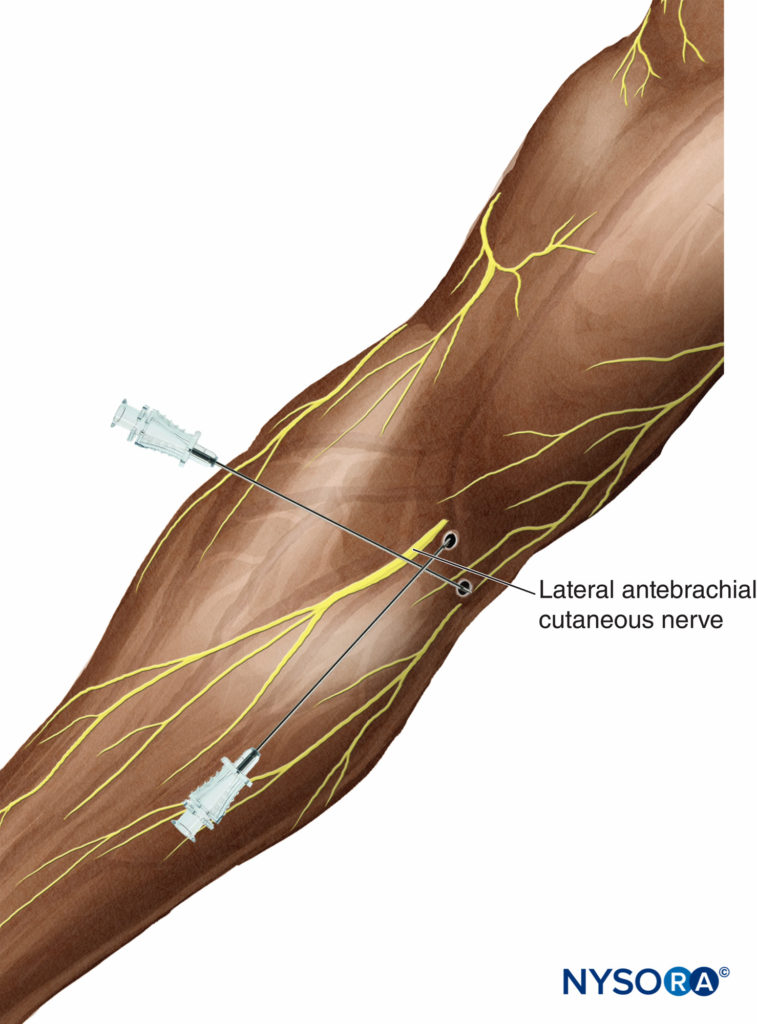
FIGURE 7. Blocks of the lateral and medial antebrachial cutaneous nerve. Anesthesia for lateral antebrachial cutaneous nerve requires two injections. The first deposits 5 mL local anesthetic just lateral to the border of the biceps tendon. A second 5 mL is then injected subcutaneously and lateral from the first injection site.
Complications
Techniques for anesthetizing the LAC and MAC nerves involveonly superficial injection of local anesthetic; thus the risk of nerve injury is very low. For this reason, these blocks may be preferable to selective elbow or wrist blocks as a supplement to incomplete brachial plexus anesthesia involving volar forearm cutaneous distribution.
NYSORA Tips
- Medial and lateral antebrachial cutaneous nerve blocks are useful techniques for superficial volar forearm procedures, such as arteriovenous fistula creation.
- The nerve blocks also represent a reasonable alternative for supplementation when proximal brachial plexus block is incomplete.
SELECTIVE NERVE BLOCKS AT THE ELBOW
Indications
Proximal techniques of brachial plexus block are often superior to selective nerve block at the elbow because the latter are more difficult to perform, are more time-consuming and uncomfortable, and potentially carry a greater risk of complications.
For instance, the practitioner may rather choose the midhumeral brachial plexus block, where selective application of clonidine or low concentration of long-acting local anesthetics to the median and ulnar nerves prolongs analgesia without concomitant prolongation of motor block. Another reason to avoid selective elbow blocks is the commonly misunderstood cutaneous innervation of the forearm. For example, block of the musculocutaneous nerve must be performed in the axilla to render motor block of the biceps and brachioradialis muscles. But anesthetizing the cutaneous distribution of the musculocutaneous nerve is best accomplished with a LAC nerve block. Anesthetizing the skin of the medial forearm requires block of the MAC nerve, not the ulnar nerve at the elbow. A third issue is to avoid elbow blocks to supplement incomplete brachial plexus blocks because this practice theoretically increases the risk of anesthesia-related nerve injury.
Indeed, the only indication for elbow approaches is to block forearm flexor and extensor muscles when the surgeon desires immobility of the fingers. Selective nerve blocks can sometimes be used also for pain treatment of minor trauma or surgery. Some authors have even reported selective catheterization to avoid unnecessary motor block or numbness of the uninvolved parts of the upper extremity.
Radial Nerve block
Anatomy
The radial nerve supplies sensation to the dorsum of the forearm and hand (see Figures 1 and 2); it also innervates the musculature of the dorsal forearm. The radial nerve descends the posterior arm, traversing from the medial to the lateral side. At the epicondyles, the radial nerve lies relatively deep between the brachialis and brachioradialis muscles (Figure 8).
FIGURE 8. Radial and median nerves are approached at the level of the epicondyles. The radial nerve is found approximately 1.5 cm lateral to the biceps tendon. The median nerve is more superficial and identified by a needle placed just medial to the brachial artery.
Technique
The patient is positioned supine for radial nerve block with the arm supinated and abducted. Selective block of the radial nerve is accomplished by placing a needle approximately 1.5 cm lateral to the biceps tendon at the level of the epicondyles (see Figure 8). Three to 5 mL of local anesthetic is injected when a paresthesia to the hand is elicited. If using a peripheral nerve stimulator, one seeks the motor response of wrist extension.
Median Nerve Block
Anatomy
The median nerve provides sensation to the radial palm, the proximal fingers from the thumb to the long finger, and motor control to the forearm flexors (see Figures 1 and 2). It passes the elbow joint just medial to the brachial artery and in front of the brachialis muscle.
Technique
Median nerve block at the elbow is accomplished with a 1.5-in. needle that is placed just medial to the brachial artery at the level of the epicondyles (see Figure 8). Either a motor response that consists of wrist flexion and/or thumb opposition or a paresthesia to the thumb or index finger is sought before injecting 3–5 mL of local anesthetic.
Ulnar Nerve Block
Anatomy
The ulnar nerve at the elbow is located superficially in the ulnar groove (Figure 9). At this level, block of the ulnar nerve results in anesthesia of the little finger and motor block of the intrinsic muscles of the hand.

FIGURE 9. Ulnar nerve block at the elbow. The forearm is flexed, the ulnar groove identified, and a needle is placed 1 cm proximal to the epicondyles and directed distally.
Technique
The patient is placed supine for ulnar nerve block, and the forearm is flexed at the elbow (see Figure 9). After identification of the ulnar groove, a short needle is placed approximately 1 cm proximal to the epicondyles and directed distally. The desired endpoint is paresthesia to the little finger or a motor response consisting of finger flexion, thumb adduction, and/or ulnar deviation of the wrist. It is suggested that only 2–3 mL of local anesthetic be injected to avoid excessive pressure within the tight fascial space of the ulnar groove and thereby lessen the possibility of compromising neural blood flow.
Complications
Selective nerve blocks at the elbow may cause hematoma if brachial artery is punctured during procedure.
NYSORA Tips
- Selective nerve blocks at the elbow can be recommended for hand surgery when forearm motor block is desired and motor block of the proximal brachial plexus block is not desired.
- Selective nerve blocks at the elbow to supplement incomplete proximal brachial plexus should be practiced with caution.
PERIOPERATIVE MANAGEMENT
Because cutaneous nerve blocks of the upper extremity require only small amounts of local anesthetic, which are typically injected subcutaneously and not close to major vessels, they can be placed with standard American Society of Anesthesiologists (ASA) monitoring. Patients should be informed to protect their insensate limb from external pressure or temperature extremes. Finally, the advent of ultrasound-guidance has substantially facilitated performance of cutaneous blocks.
SUMMARY
Selective upper extremity nerve blocks can be useful supplements to brachial plexus blocks. Supraclavicular, suprascapular, and intercostobrachial nerve blocks are valuable adjuncts to the anesthesia and/or analgesia primarily provided by a plexus block or general anesthesia. The LAC and MAC nerve blocks can provide either primary anesthesia for superficial forearm operations or supplement an incomplete plexus block. Selective elbow blocks are inferior alternatives to brachial plexus blocks. Their use as a supplement to incomplete plexus block should be carefully considered.
REFERENCES
- Neal JM, Hebl JR, Gerancher JC, Hogan QH: Brachial plexus anesthesia: essentials of our current understanding. Reg Anesth Pain Med 2002; 27:402–428.
- Ritchie E, Tong D, Chung F, et al: Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modelity? Anesth Analg 1997;84:1306–1312
- Singelyn RJ, Lhotel L, Fabre B: Pain relief after arthroscopic shoulder surgery: acomparison of intraarticular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg 2004;99: 589–592.
- Neal JM, McDonald SB, Larkin KL, Polissar NL: Suprascapular nerve block prolongs analgesia after nonarthroscopic shoulder surgery, but does not improve outcome. Anesth Analg 2003;96:982–986.
- Finucane BT, Yilling F: Safety of supplementing axillary plexus blocks. Anesthesiology 1989;70:401–403.
- Iskandar H, Guillaume E, Dixmerias F, et al: The enhancement of sensory block by clonidine selectively added to mepivacaine after midhumeral block. Anesth Analg 2001;93:771–775.
- Bouaziz H, Narchi P, Mercier FJ, et al: The use of selective axillary nerve block for outpatient hand surgery. Anesth Analg 1998;86:746–748.
- Frenkel O, Herring AA, Fischer J, Carnell J, Nagdev A. Supracondylar radial nerve block for treatment of distal radius fractures in the emergency department. J Emerg Med. 201;41(4):386–388.
- Lurf M, Leixnering M. Ultrasound-guided ulnar nerve catheter placement in the forearm for postoperative pain relief and physiotherapy. Acta Anaesthesiol Scand. 2009;53(2):261–263.
- McCartney CJ, Xu D, Constantinescu C, et al:. Ultrasound examination of peripheral nerves in the forearm. Reg Anesth Pain Med. 2007;32(5): 434–439.