Explore NYSORA knowledge base for free:

Gold-Standard Content

Test out 7 days for free!

Regular content updates and user-experience upgrades...and more!
Join the community of over 30,000 professionals worldwide and see for yourself why NYSORA’s US-Guided Interventional Pain APP is the first and the most authoritative guide to ultrasound and nerve blocks.

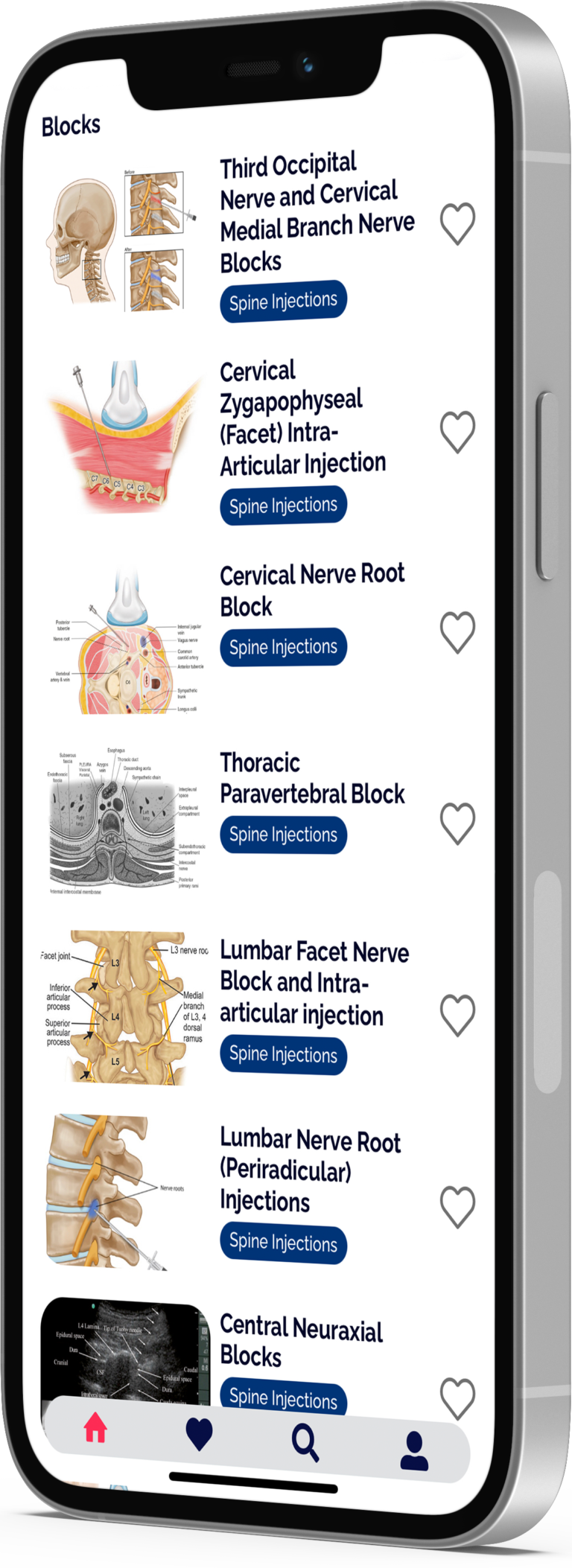
Gain access to the most authoritative guide on US-guided interventional chronic pain interventions, including: Spine Injections, Abdominal and Pelvic Blocks, Peripheral Nerve Blocks, Diagnostic and Musculoskeletal Ultrasound, Diagnostic Neurosonology, Joint Injections, Nerve Blocks, Interventional Headache Treatment, Stimulation Procedures and more…
Subscribe and get full access! With annual subscription subscribers will receive a proof of payment for education reimbursement. You also save 15% if you choose the annual subscription instead of monthly!

Join the community of over 30,000 professionals worldwide and see for yourself why NYSORA’s US-Guided Interventional Pain APP is the first and the most authoritative guide to ultrasound and nerve blocks.
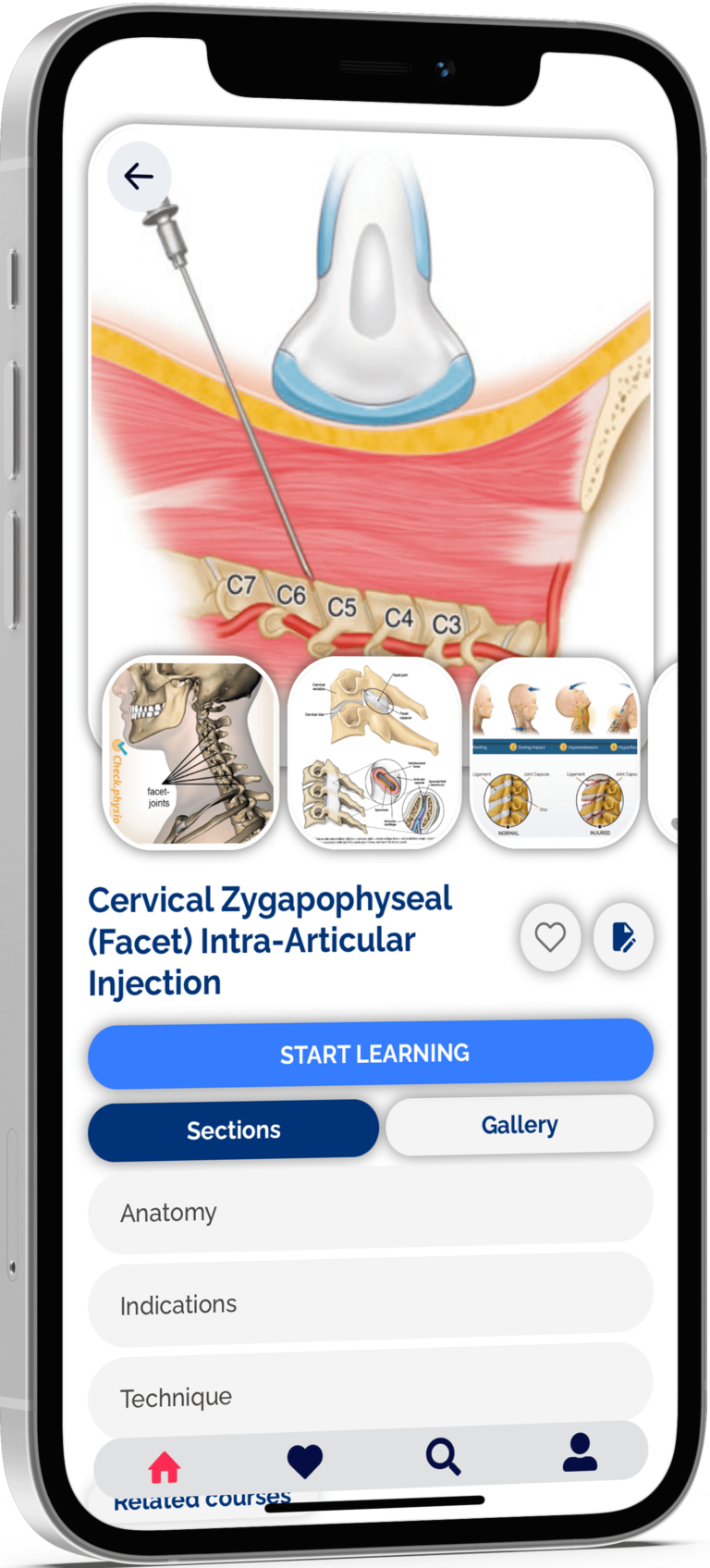
Clear images, illustrations, ultrasound images, functional anatomy, and ultrasound-guided pain and MSK procedures
Review and perform interventional chronic pain interventions, including joint injections, and US-guided stimulation procedures
Featuring tried-and-true US-guided Pain blocks techniques used by practitioners worldwide
Based on the world’s leading authority on ultrasound, Dr. Samer Narouze’s book “Atlas of Ultrasound-Guided Procedures in Interventional Pain Management” NYSORA’s Ultrasound-Guided Pain Blocks App describes the most practical and applicable techniques of ultrasound-guided pain medicine.