Jui-An Lin, Thomas F. Bendtsen, Ana M. Lopez, and Hassanin Jalil
FACTS
- Indications: Hand and wrist surgery
- Transducer position: Transverse on the elbow
- Goal: Injection of local anesthetic within the vicinity of individual nerves (radial, median, and ulnar)
- Local anesthetic: 4–5 mL per nerve
GENERAL CONSIDERATIONS
Ultrasound imaging of individual nerves in the distal upper limb allows for reliable nerve block. The two main indications for a forearm block are a standalone technique for hand and/or wrist surgery and as a means of rescuing or supplementing an incomplete or failed proximal brachial plexus block. Advantages of rescue block are the reduction of the risk of vascular puncture and in the overall volume of local anesthetic used. There are a variety of locations where a practitioner could approach each of these nerves, most of which are similar in efficacy. In this section, we present the approach for each nerve at the level of the elbow (Figure 1).
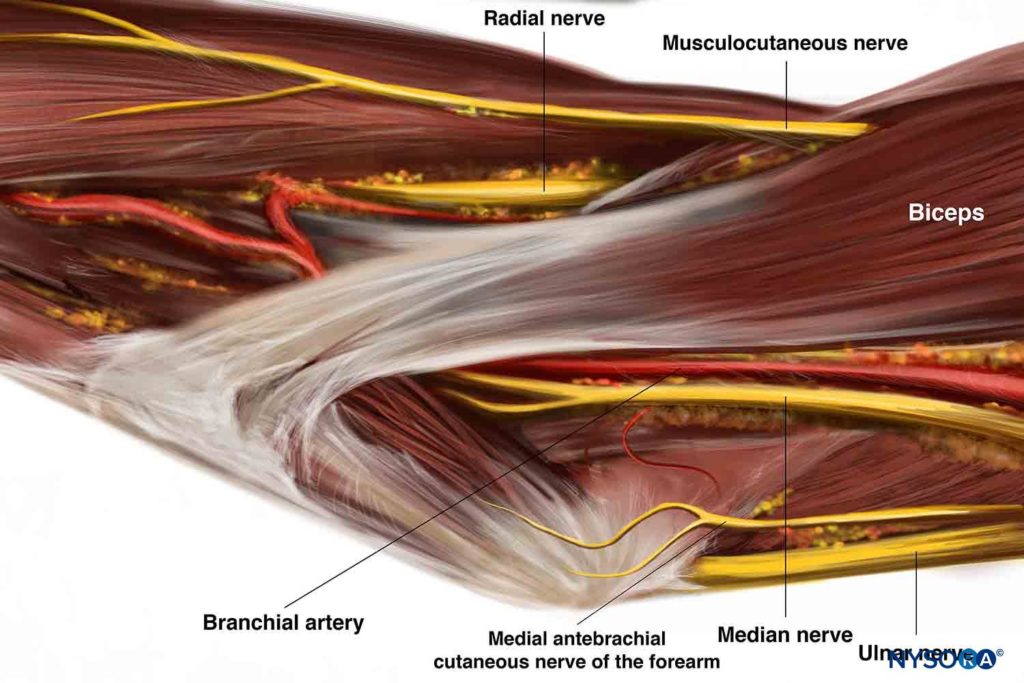
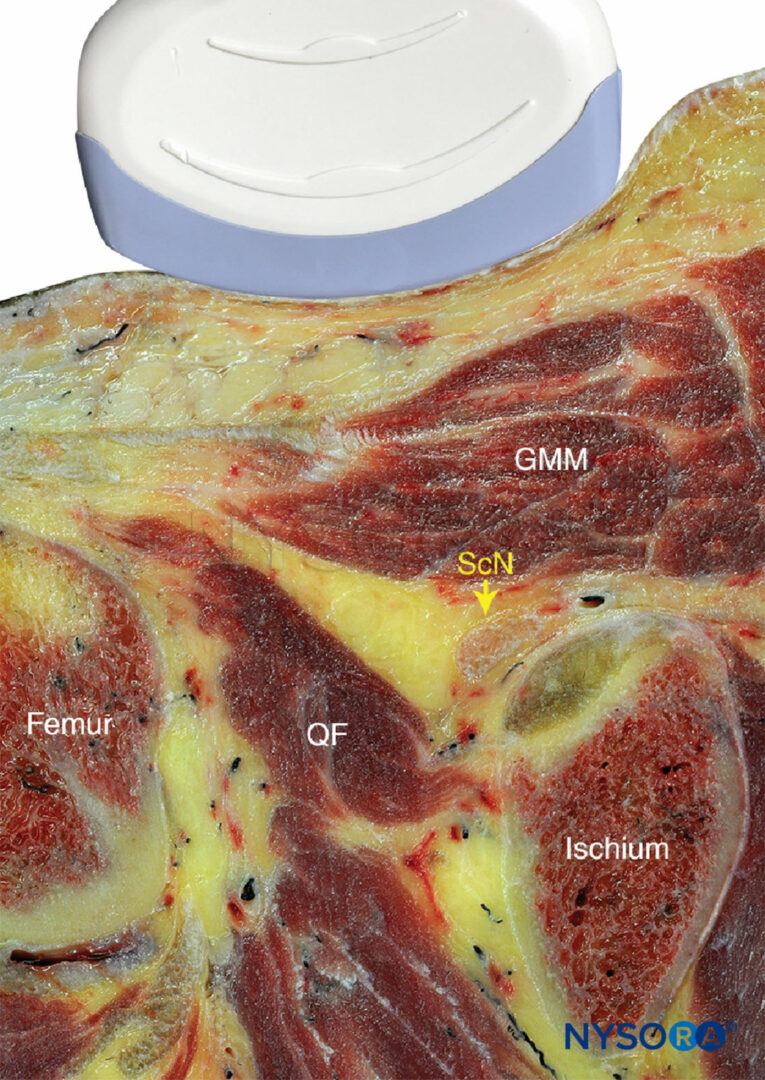
Figure 1. Anatomic relationship of the radial, median, ulnar, and musculocutaneous nerves, at the level of the elbow.
Ultrasonographic assessment shows that a median nerve block using nerve stimulation alone is commonly associated with intraneural injection. Some authors have suggested additional indications for forearm blocks, in combination with a proximal brachial plexus block. Combining proximal and distal blocks allows for a decrease in onset time and improved block consistency. It is possible to use these blocks in the setting of wrist or hand surgery involving the bone to provide long-lasting analgesia without blocking the whole limb for many hours; this is done by combining a short-acting brachial plexus block with distal blocks around the elbow, according to the surgical procedure. If distal blocks are to be performed after a proximal brachial plexus block, it is of paramount importance to clearly visualize the needle tip at all times to avoid intraneural injection.
ULTRASOUND ANATOMY
The Radial Nerve
The radial nerve is best visualized above the lateral aspect of the elbow, lying in the interfascial plane between the brachioradialis and the brachialis muscles (Figure 2). The transducer is placed transversely on the anterolateral aspect of the distal arm, 3–4 cm above the elbow crease. The nerve appears as a hyperechoic, triangular or oval structure with the characteristic honeycomb appearance of a distal peripheral nerve. The nerve divides just distal to the elbow crease into the superficial (sensory) and deep (motor) branches. These smaller divisions of the radial nerve are more challenging to identify in the forearm; therefore, a single injection above the elbow is favored because it ensures block of both. The transducer can slide up and down the arm to better visualize the nerve and the musculature surrounding it. As the transducer is moved proximally, the nerve will be seen to travel posteriorly and closer to the humerus, to lie deep to the triceps muscle in the spiral groove (Figure 3).
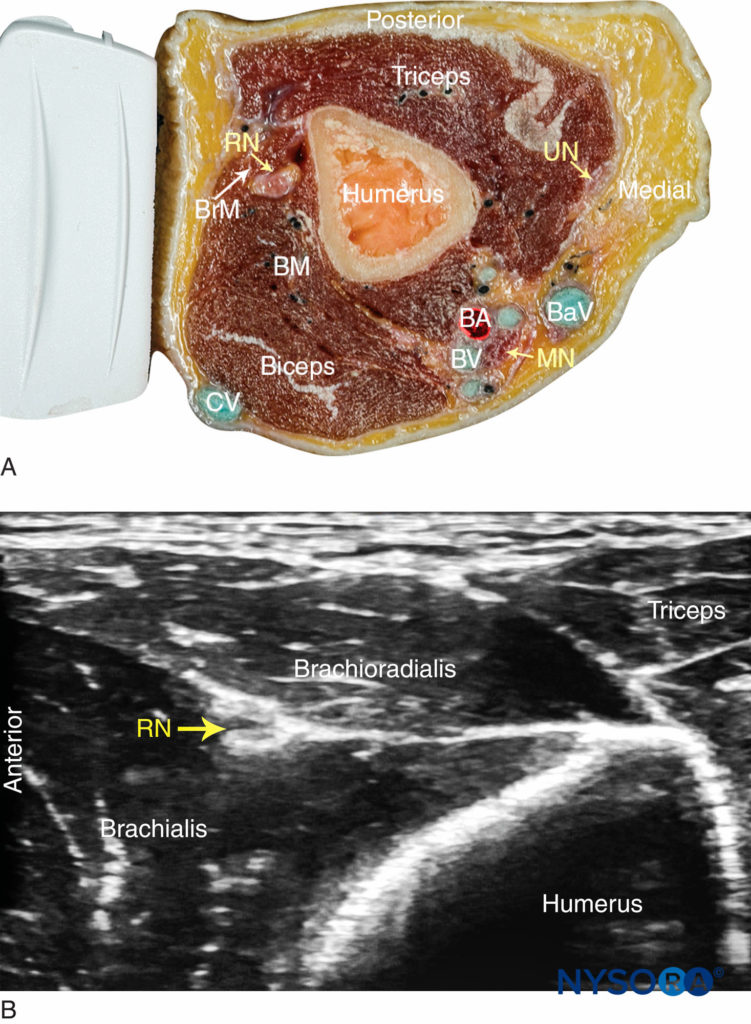
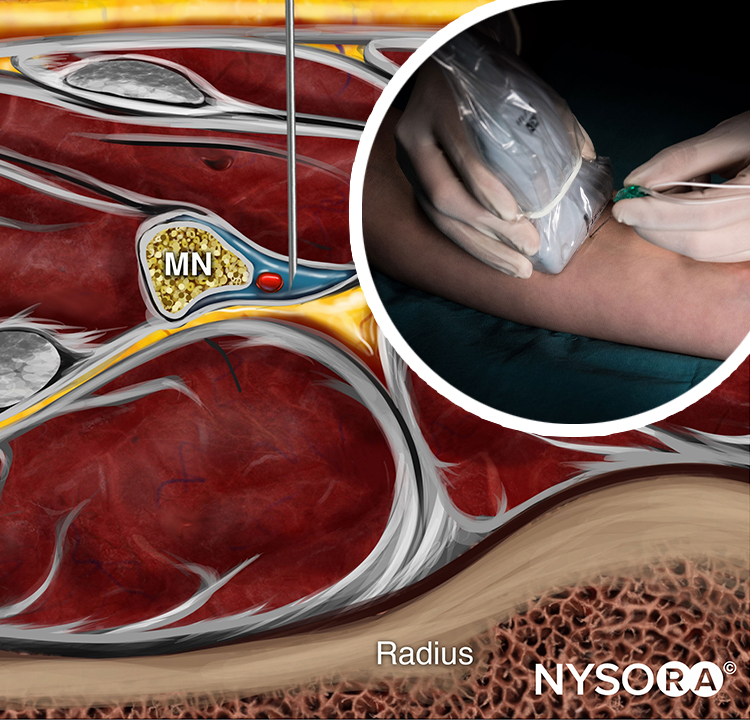
FIGURE 2. (A) Radial nerve (RN) anatomy at the distal third of the humerus. BrM, brachioradialis muscle; BM, brachialis muscle; BA, brachial artery; BV, brachial vein, BaV, basilic vein, CV, cephalic vein; UN, ulnar nerve; MN, median nerve. (B) Sonoanatomy of the radial nerve at the distal arm. The RN is located between the brachioradialis and the brachialis muscles.
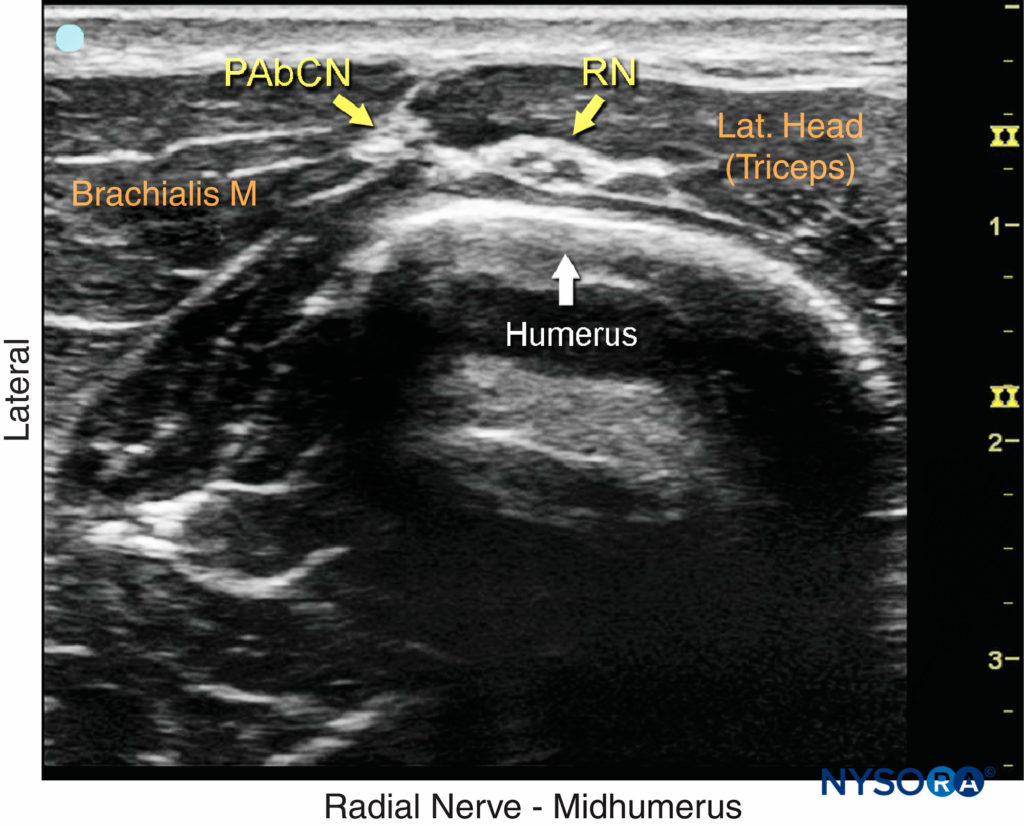
FIGURE 3. Sonoanatomy of the radial nerve (RN) in the spiral groove of the humerus. PAbCN, posterior antebrachial cutaneous nerve.
The Median Nerve
The median nerve is imaged at the level of the elbow crease, as it is located superficially. The transducer is placed just above the crease and adjusted to obtain a clear view of the brachial artery. The median nerve lies on the medial side in close contact to the artery as a hyperechoic oval-shaped structure of about the same size of the artery (Figure 4). Scanning proximally, both the nerve and the artery can be easily followed up to the axilla as they course together, although changing the relative position to one another. Scanning distally to the elbow crease, the median nerve separates from the artery and lies deep to the pronator teres muscle and the flexor digitorum superficialis as it reaches the mid-forearm.
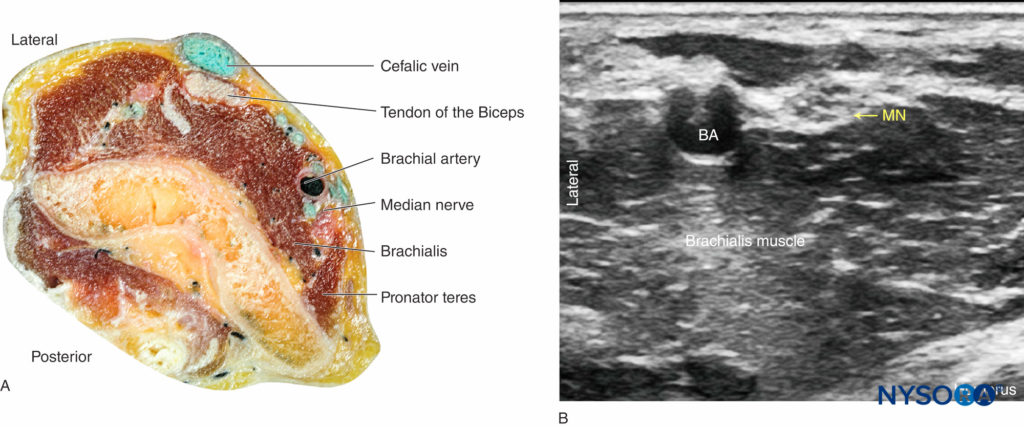
FIGURE 4 (A) Anatomy section of the distal arm at the level of the elbow. (B) Sonoanatomy of the median nerve proximally to the elbow crease.
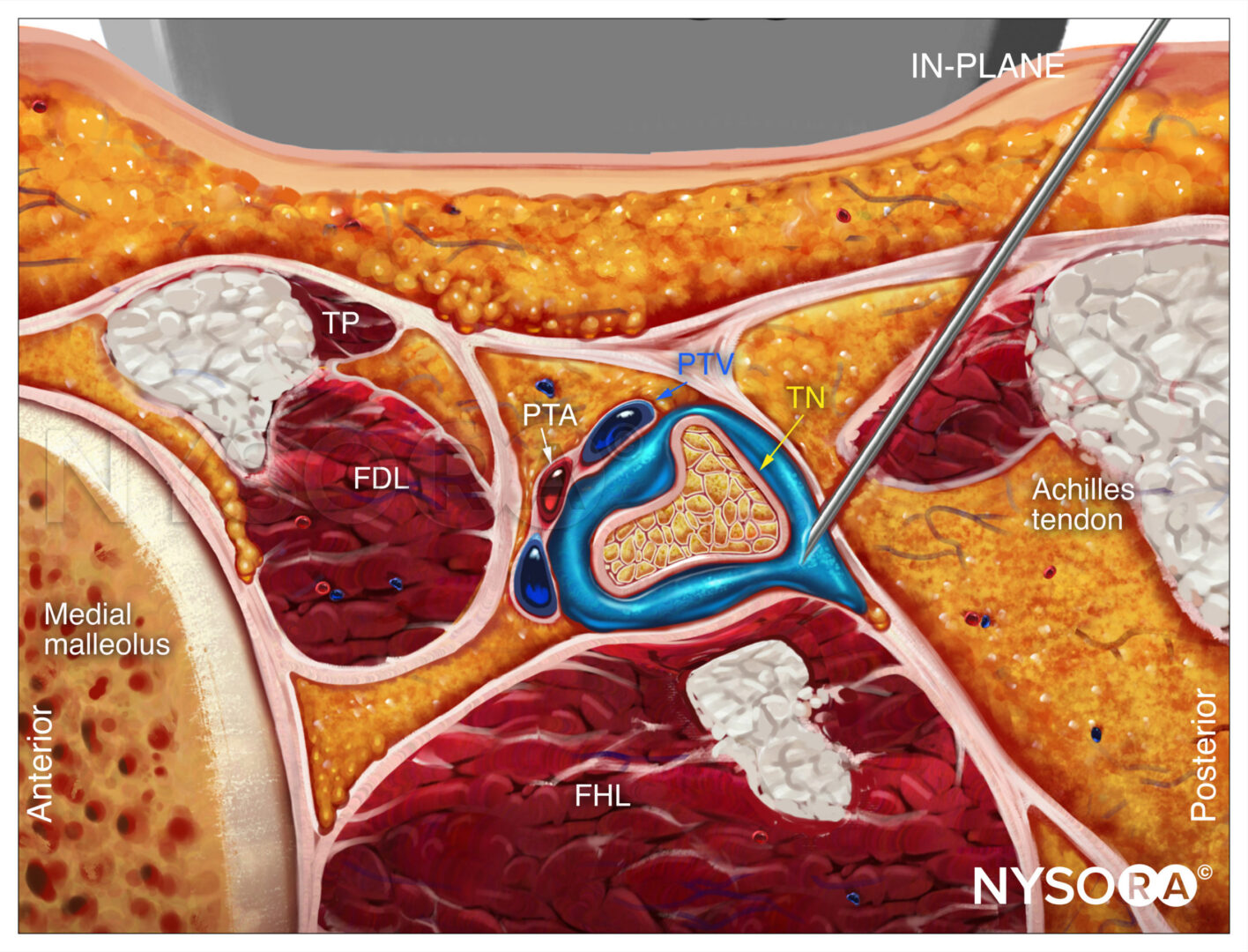
The Ulnar Nerve
The ulnar nerve is identified at the posteromedial aspect of the elbow, few centimeters proximally to the crease, as a hyperechoic oval “honeycomb” structure immediately underneath the brachial fascia and superficial to the triceps muscle (Figure 5). The ulnar nerve can be traced distally toward the ulnar notch, where it appears as a round hypoechoic structure diving into the bony ulnar sulcus before entering the forearm underneath the flexor carpi ulnaris muscle. Sliding the transducer proximally, the nerve can be easily traced back to the axilla along the medial aspect of the arm.
For a more comprehensive review of the innervation of the hand, see Functional Regional Anesthesia Anatomy.
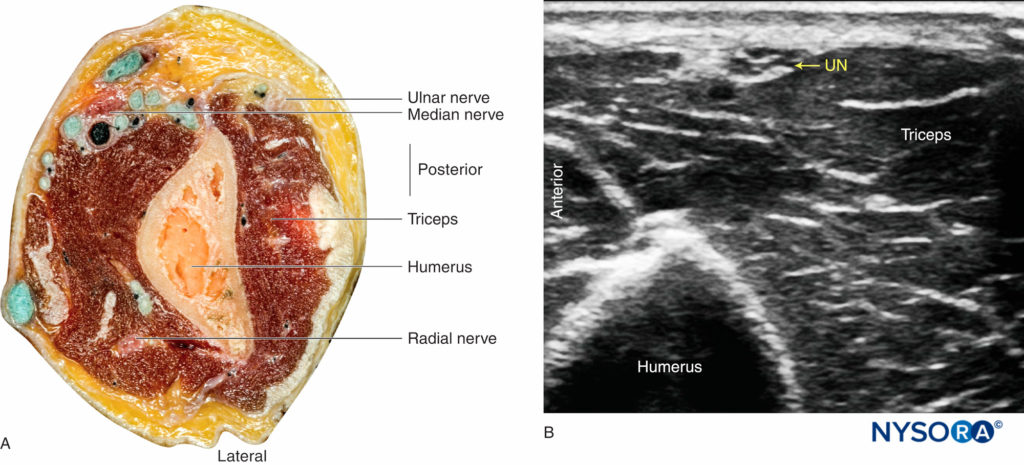
FIGURE 5 (A) Anatomy section of the distal arm at the level of the elbow. (B) Sonoanatomy of the ulnar nerve proximally to the elbow crease.
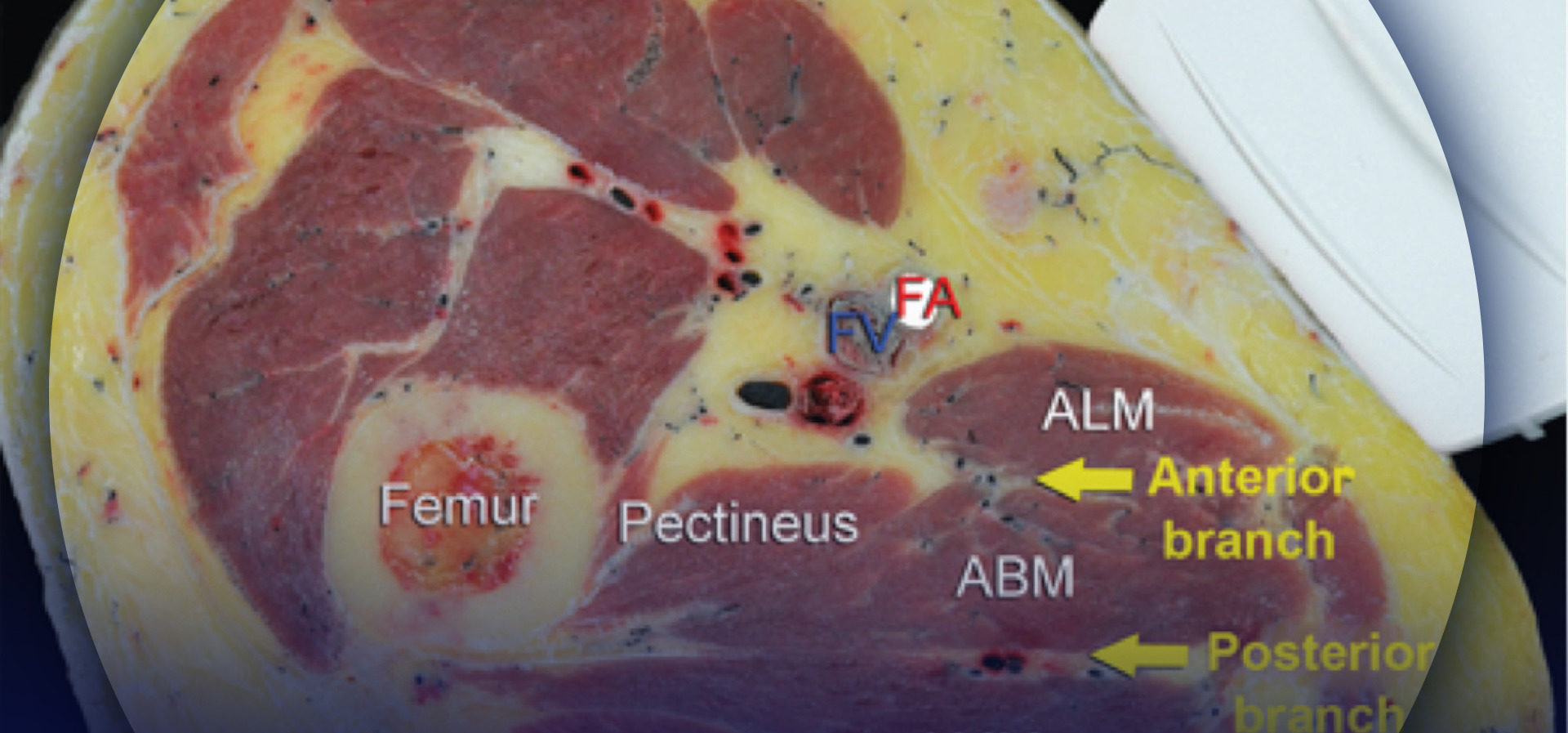
DISTRIBUTION OF ANESTHESIA
Anesthetizing the radial, median, and/or ulnar nerves provides sensory anesthesia and analgesia to the respective territories of the hand, forearm, and wrist. Note that the lateral cutaneous nerve of the forearm (a branch of the musculocutaneous nerve) supplies the lateral aspect of the forearm, and it may need to be blocked separately by a subcutaneous wheal distal to the elbow if lateral wrist surgery is planned. The same applies for the medial cutaneous nerve of the forearm (Figure 1). The use of a tourniquet, either on the arm or forearm, usually requires sedation and/or additional analgesia.
EQUIPMENT
The equipment recommended for a forearm block includes the following:
- Ultrasound machine with a linear transducer (8–14 MHz), sterile sleeve, and gel
- Standard nerve block tray
- Three 5 mL syringes containing local anesthetic
- A 2-in, 22- to 25-gauge, short-bevel, insulated stimulating needle (optional)
- Peripheral nerve stimulator (optional)
- Sterile gloves
- Pressure monitoring
NYSORA Tips
Because these are superficial blocks of the distal peripheral nerves, some practitioners choose to use a small-gauge (eg, 25-gauge) needle. When using a small-gauge needle, however, meticulous attention should be paid in order to avoid an intraneural injection, which is more likely with a smaller-diameter and sharp-tip design.
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
Typically, the block is performed with the patient in the supine position. For the radial nerve block, the arm could also be flexed at the elbow, and the hand is placed on the patient’s abdomen (see Figure 6a). This position allows for the most practical application of the transducer. The median and ulnar nerves are blocked with the arm abducted. (see Figures 7a and 8a).
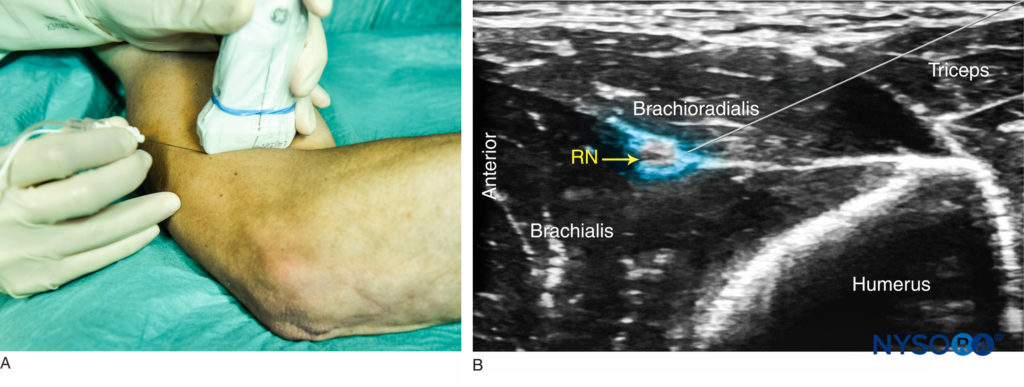
FIGURE 6. (A) Position of the arm, probe, and needle for radial nerve block. (B) Distribution of local anesthetic (blue-shaded area) for RN block above the elbow.
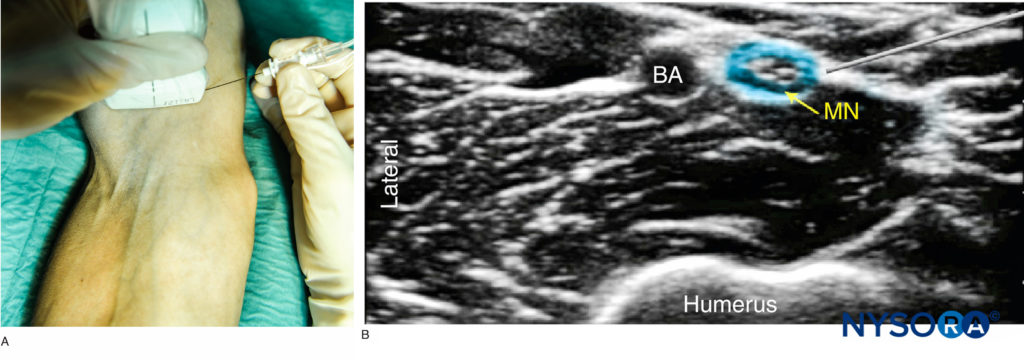
FIGURE 7. (A) Position of the arm, probe and needle for median nerve block proximal to the elbow. (B) Distribution of local anesthetic (blue-shaded area) for MN block. BA, brachial artery.
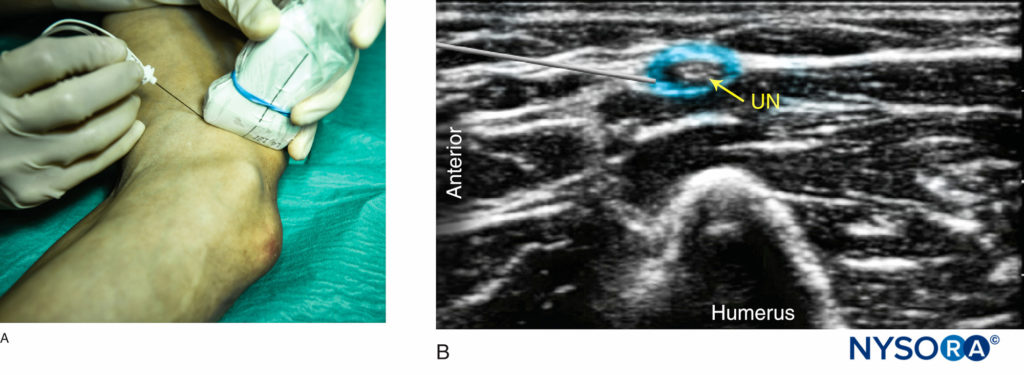
FIGURE 8.(A) Position of the arm, probe and needle for ulnar nerve block proximal to the elbow. (B) Distribution of local anesthetic (blue-shaded area) for UN block.
GOAL
The goal of a forearm block is to place the needle tip adjacent to the nerve(s) of choice and to deposit 4–5 mL of local anesthetic within the fascial sheath enclosing the nerve. It is unnecessary to completely surround the entire nerve in a circumferential pattern, although this can enhance the speed of block onset. As with all peripheral blocks, it is imperative to avoid high opening injection pressure in order to decrease the risk of intrafascicular injection.
TECHNIQUE
The Radial Nerve
The skin is disinfected and the transducer positioned so as to identify the radial nerve. The needle is inserted in plane, with the goal of traversing the brachioradialis muscle and placing the tip next to the radial nerve (Figure 6a). If nerve stimulation is used, a wrist or finger extension response should be elicited when the needle is within proximity of the nerve. After negative aspiration, 4–5 mL of local anesthetic is injected (Figure 6b). If the spread is inadequate, slight adjustments can be made and a further 2–3 mL of local anesthetic administered. It is also possible to block the branches of the radial nerve in the forearm. Anterior to the elbow joint, the radial nerve can be visualized between the extensor carpi radialis muscles (longus and brevis) and brachioradialis. The superficial branch can then be seen clearly at the proximal forearm covered by the brachioradialis. The deep branch is more difficult to image, as it emerges at the level of the radial neck and passes into the posterior compartment by passing between the two heads of the supinator muscle.
The Median Nerve
With the arm abducted and the palm facing up, the skin of the anterior and medial side of the elbow is disinfected and the transducer positioned transversely on the antecubital fossa. The median nerve should be identified on the medial side of the artery. If it is not immediately visualized, the transducer should be positioned slightly more medially and the brachial artery identified using color Doppler ultrasound. The needle is inserted in-plane from either side of the transducer, although a medial to lateral approach is usually more convenient to avoid the artery that lies lateral to the nerve. (Figure 7a). After negative aspiration, 4–5 mL of local anesthetic is injected (Figure 7b). If the spread is inadequate, slight adjustments can be made and a further 2–3 mL of local anesthetic administered.
The Ulnar Nerve
The transducer is then positioned more medially until the ulnar nerve is identified. The needle is inserted in-plane from either side of the transducer (the anterior to posterior side is often more ergonomic) (Figure 8a). After negative aspiration, 4–5 mL of local anesthetic is injected (Figure 8b). If the spread of local anesthetic is inadequate, slight adjustments can be made and a further 2–3 mL administered.
TIPS
- When in doubt, nerve stimulation (0.5–1.0 mA) can be used to confirm the localization of the correct nerve.
- The out-of-plane approach can also be used for all three blocks.
REFERENCES
- Dufour E, Cymerman A, Nourry G, et al: An ultrasonographic assessment of nerve stimulation-guided median nerve block at the elbow: a local anesthetic spread, nerve size, and clinical efficacy study. Anesth Analg 2010;111:561–567.
- Fredrickson MJ, Ting FS, Chinchanwala S, Boland MR: Concomitant infraclavicular plus distal median, radial, and ulnar nerve block accelerates upper extremity anaesthesia and improves block consistency compared with infraclavicular block alone. Br J Anaesth 2011;107:236–242.
- Dufeu N, Marchand-Maillet F, Atchabahian A, et al: Efficacy and safety of ultrasound-guided distal blocks for analgesia without motor block after ambulatory hand surgery. J Hand Surg Am 2014;39:737–743.
- Anagnostopoulou S, Saranteas T, Chantzi C, Dimitriou V, Karabinis A, Kostopanagiotou G: Ultrasound identification of the radial nerve and its divisions. Is rescue nerve block at or below the elbow possible? Anaesth Intensive Care 2008;36:457–459.
- Eichenberger U, Stockli S, Marhofer P, et al: Minimal local anesthetic volume for peripheral nerve block: a new ultrasound-guided, nerve dimension-based method. Reg Anesth Pain Med 2009;34:242–246.
- Gray AT, Schafhalter-Zoppoth I: Ultrasound guidance for ulnar nerve block in the forearm. Reg Anesth Pain Med 2003;28:335–339.
- Lurf M, Leixnering M: Sensory block without a motor block: ultrasound-guided placement if pain catheters in forearm. Acta Anaesthesiol Scand 2010;54:257–258.
- McCartney CJ, Xu D, Constantinescu C, Abbas S, Chan VW: Ultrasound examination of peripheral nerves in the forearm. Reg Anesth Pain Med 2007;32:434–439.
- Schafhalter-Zoppoth I, Gray AT: The musculocutaneous nerve: ultrasound appearance for peripheral nerve block. Reg Anesth Pain Med 2005;30:385–390.
- Spence BC, Sites BD, Beach ML: Ultrasound-guided musculocutaneous nerve block: a description of a novel technique. Reg Anesth Pain Med 2005;30:198–201.