1. INTRODUCTION
Pathology of muscles and tendons of the arm is not very common and clinically relevant. On the other hand, compressive neuropathies affecting the main nerve trunks of the upper limb, and especially the median nerve and the radial nerve, may present with a spectrum of confusing and, sometimes, ambiguous clinical pictures for the physician. These neuropathies are often related to anatomic constraints, may be acute or chronic, and require a thorough understanding of the pathophysiology and clinical correlation. Current improvements in US technology have contributed significantly to the more accurate diagnosis of these conditions.
2. CLINICAL AND US ANATOMY
The arm extends from the shoulder to the elbow. It is formed by two main compartments – anterior and posterior – separated by a plane passing through the humerus and the lateral and medial intermuscular septa, which are thick fibrous extensions of the brachial fascia attached to the medial and lateral supracondylar ridge of the humerus (Fig. 1). The anterior compartment (flexor compartment) contains three muscles – the coracobrachialis, the biceps brachii and the brachialis – and the musculocutaneous nerve. The posterior compartment (extensor compartment) houses the large triceps brachii muscle, consisting of three heads – long, lateral and medial – and the radial nerve. At the upper medial aspect of the arm, the main neurovascular bundle, consisting of the brachial artery, some veins and three nerves – median, ulnar and radial – courses in the neurovascular compartment, a groove delimited by a division of the medial intermuscular septum and bounded by the biceps anteriorly and the triceps posteriorly. A basic description of the normal and US anatomy of the anterior and posterior compartments is included here.
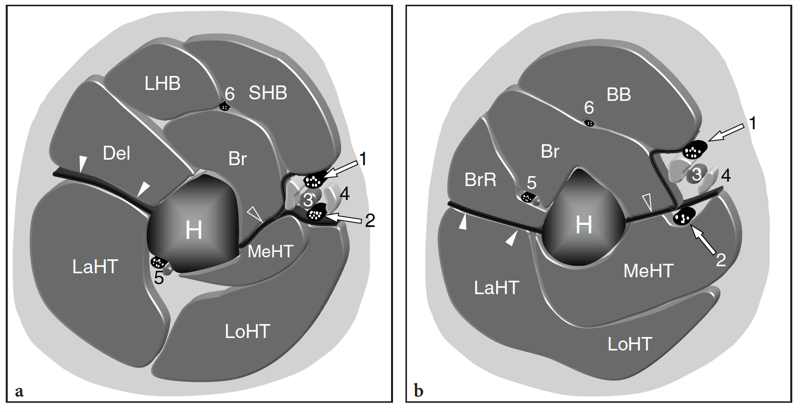
Fig. 1a,b. Schematic drawings of two cross-sectional planes through the proximal (a) and middle third (b) of the right arm illustrate the anatomic relationships among muscles, neurovascular structures and the humerus (H). Observe the lateral (white arrowheads) and medial (open arrowhead) intermuscular septa which separate the anterior and posterior compartments. On the medial aspect of the arm, the medial intermuscular septum divides into distinct anterior and posterior layers which form a third compartment of the arm – the neurovascular compartment – and together they separate the anterior compartment from the posterior compartment. The anterior compartment houses the brachialis (Br), the long head (LHB) and the short head (SHB) of the biceps brachii (BB) muscle. Between these muscles and the lateral intermuscular septum, the distal part of the deltoid (Del) is found proximally (a) and the brachioradialis muscle (BrR) distally (b). The coracobrachialis muscle is not shown. The posterior compartment contains the three muscle bellies of the triceps brachii muscle, namely the lateral head (LaHT), the long head (LoHT) and the medial head (MeHT). In the proximal neurovascular compartment (a), the median nerve (1) and the ulnar nerve (2) course next to the brachial artery (3) and the basilic vein (4). More distally (b), the ulnar nerve moves to the posterior compartment to descend tightly bound to the medial head of the triceps. In a the radial nerve (5) lies superfi cial to the midshaft of the humerus, in the so-called spiral groove. Similar to the ulnar nerve, also the radial nerve changes compartment while descending the arm. In fact, it passes from posterior to anterior to course (b) between the brachioradialis and the brachialis muscle in the distal third of the arm. In the anterior compartment, note the position of the last nerve of the arm, the musculocutaneous nerve (6), which lies between the biceps and the brachialis muscles.
3. ANTERIOR ARM
The anterior compartment of the arm houses three muscles: the coracobrachialis, the biceps brachii and the brachialis (Fig. 2). The coracobrachialis takes its origin from the tip of the coracoid process, medial to the insertion of the short head of the biceps, and continues down and laterally to insert onto the medial aspect of the middle third of the humeral shaft. The biceps brachii is formed by a combination of two muscle bellies: the long head and the short head. As already described, the long head originates from a long tendon which extends from the supraglenoid tubercle, the superior glenoid rim and labrum, curves over the humeral head and passes throughout the bicipital sulcus to continue in a fusiform muscle belly (Fig. 2b). The short head arises from the tip of the coracoid process from a straight tendon which is shorter than that of the long head but longer than the adjacent coracobrachialis tendon (Fig. 2b). At the distal arm, the two heads of the biceps unite to create a large muscle which is located superficial to the brachialis and ends in a long distal tendon which attaches into the radial tuberosity. The brachialis muscle is located between the distal biceps brachii and the humeral shaft (Fig. 2a). It originates from the distal half of the anterior face of the humerus and the intermuscular septa and descends more distally than the biceps brachii to continue in a short tendon which inserts into the coronoid process of the ulna and the ulnar tuberosis. From the biomechanical point of view, the coracobrachialis plays a role as an extensor and adductor of the arm, whereas the brachialis and the biceps brachii are powerful flexors of the forearm. Furthermore, the biceps brachii is a supinator of the forearm and a weak flexor of the arm. US examination of the anterior arm is best performed with the patient lying supine keeping the arm abducted (Fig. 3). Different degrees of internal and external rotation of the arm may be helpful in evaluating the anatomic structures placed more laterally and medially. Sweeping the probe down from the tip of the coracoid, transverse US images demonstrate the coracobrachialis muscle followed by the two heads of the biceps brachii (Fig. 3a–c). More distally, the biceps is seen overlying the deep brachialis muscle, which rests over the anterior humeral cortex (Fig. 3d,e). The lateral and medial intermuscular septa separate the anterior muscles from posterior lateral and medial heads of the triceps muscle.
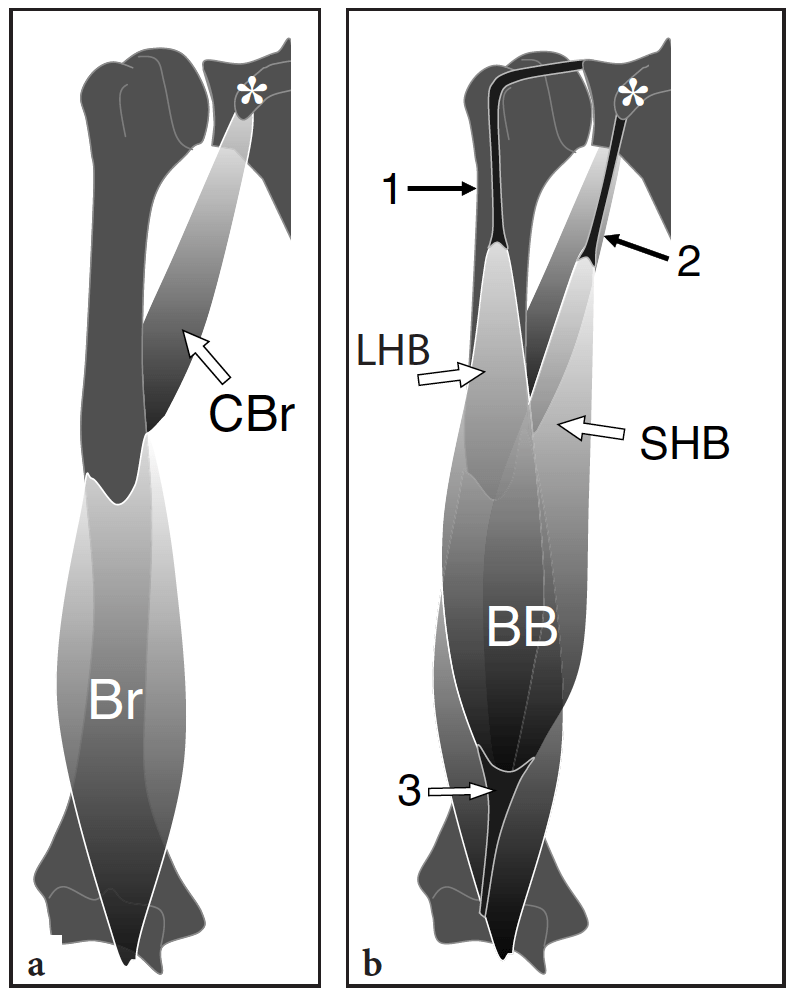
Fig. 2a,b. Schematic drawing of a coronal view of the anterior muscles of the arm. a The coracobrachialis muscle (CBr) takes its origin from the lateral aspect of the coracoid process (asterisk) of the scapula through a short tendon and inserts into the medial aspect of the middle third of the humeral shaft. The more distal brachialis muscle (BR) arises from the distal half of the anterior humerus to attach onto the anterior aspect of the coronoid process of the ulna. b More superficially, the biceps brachii (BB) muscle consists of the distal convergence of two bellies: the long head (LHB) and the short head (SHB). Observe the tendon of the long head (1) and the close relationship of the tendon of the short head (2) with the origin of the coracobrachialis. The biceps muscle is located superficial to the brachialis and continues downward in a long distal tendon (3) which inserts into the tuberosity of the radius.
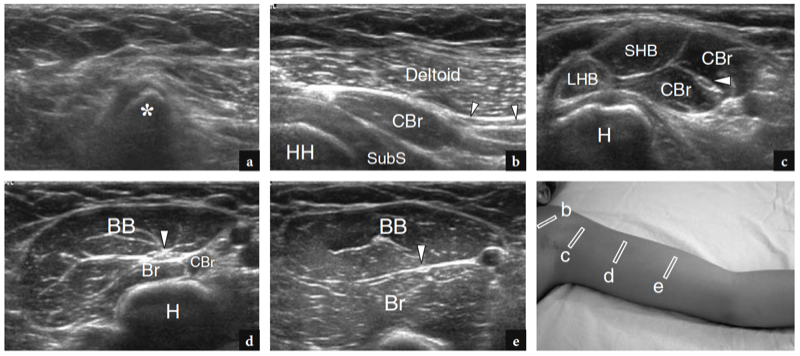
Fig. 3a–e. Anterior muscles and musculocutaneous nerve. a–e Series of transverse 12–5 MHz US images obtained from cranial (a) to caudal (e) over the anterior aspect of the arm. a The coracoid process (asterisk) of the scapula, which is the origin of the conjoined tendon of the coracobrachialis and the short head of the biceps, appears as a rounded hyperechoic structure with well-defined posterior acoustic shadowing. b The coracobrachialis muscle (CBr) can be found between the deltoid and the subscapularis (SubS). The musculocutaneous nerve (arrowheads) is recognized as a thin hypoechoic elongated structure running just superfi cial to the medial aspect of the coracobrachialis. HH, humeral head. c At the proximal arm, the long head (LHB) and the short head (SHB) of the biceps become progressively visible. The smaller belly of the long head lies lateral to the short head. On these planes, the musculocutaneous nerve (arrowhead) can be seen running inside the coracobrachialis muscle CBr. H, humerus. d At the mid-arm, the two heads of the biceps muscle (BB) fuse together. The musculocutaneous nerve lies among the distal part of the coracobrachialis (CBr), the proximal part of the brachialis (Br) and the biceps brachii (BB) muscles. H, humerus. e At the distal arm, the biceps brachii overlies the large brachialis muscle. The musculocutaneous nerve is found in the hyperechoic cleavage plane separating these two muscles. The photograph at the bottom right of the figure indicates probe positioning.
Among the four nerves of the arm (median, ulnar, radial and musculocutaneous), the musculocutaneous is the one crossing the anterior aspect of the arm (Fig. 4a). This nerve arises from the lateral cord of the brachial plexus (C5–C7 level). It pierces the coracobrachialis and then descends on the anterior aspect of the brachialis between this muscle and the biceps (Fig. 4b,c). On transverse US images, the musculocutaneous nerve can be recognized piercing the coracobrachialis (Fig. 3c). Its detection may be not straightforward in obese patients. After coursing between the brachialis and biceps brachii the nerve pierces the superficial fascia of the arm to enter the subcutaneous tissue and emerge above the elbow crease as the lateral cutaneous nerve of the forearm. The nerve then divides in two small terminal branches, anterior and posterior. The musculocutaneous nerve supplies the coracobrachialis, the biceps brachii and the brachialis and then distributes to the skin of the forearm as the lateral (antebrachial) cutaneous nerve. On the anterolateral aspect of the arm, the cephalic vein courses over the superficial fascia and the biceps muscle.
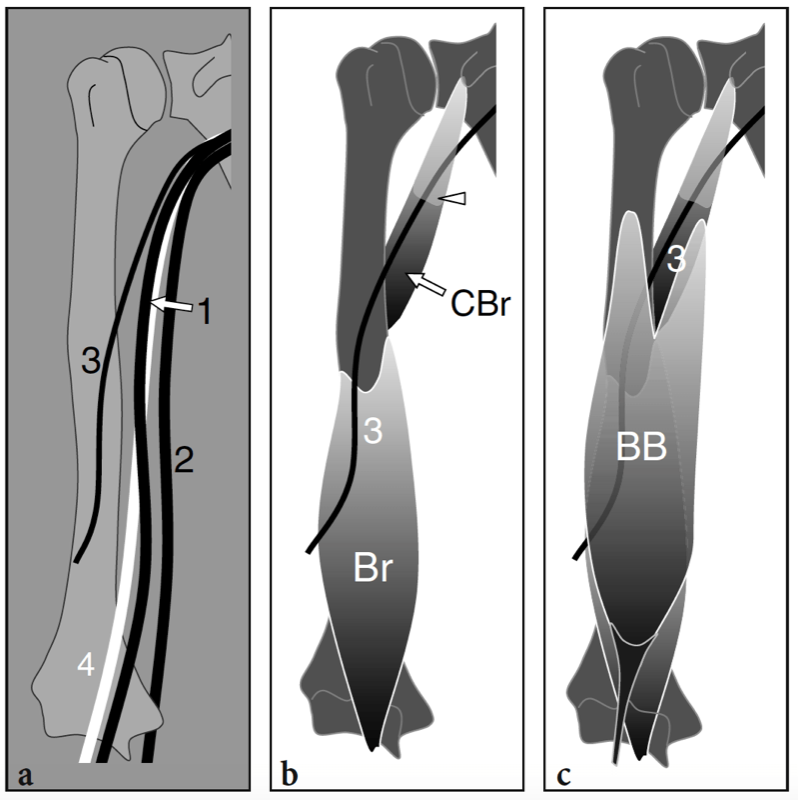
Fig. 4a–c. Neurovascular structures of the anterior and medial aspect of the arm. a Schematic drawing illustrates the median (1) and ulnar (2) nerves as they descend the bicipital fossa, a longitudinal groove delimited by the medial head of the triceps posteriorly and the biceps and brachialis muscles anteriorly. At the proximal arm, the median nerve courses lateral to the brachial artery (4) whereas, at the middle third of the arm, it crosses the artery to descend medial to it down to the antecubital fossa. b,c The musculocutaneous nerve (3) is seen piercing (arrowhead) the coracobrachialis muscle (CBr) to enter the anterior compartment of the arm where it lies between the posterior brachialis (Br) and the superficial biceps brachii (BB). At the distal arm, this nerve becomes subcutaneous a b c to divide into its terminal branches.
Some anatomic variants can be found at the anteromedial aspect of the arm. The most common vascular anomaly is the proximal division of the humeral artery in the radial and ulnar artery. Although this variant is not associated with clinical symptoms, it should be described in the US report as it can cause problems during attempted catheterization of the humeral artery. Another rare but potentially symptomatic variant is the supracondylar process of the humerus (Fig. 5a–c). This bone anomaly refers to a triangular spur-like process which arises 5–7 cm above the medial epicondyle and is typically oriented distally and medially ending with a beak-like apex (Sener et al. 1998). The supracondylar process is a primitive remnant present in climbing mammals encountered in approximately 1% of normal limbs. It is usually found in association with a ligament, commonly known as the ligament of Struthers, which joins its tip with the medial epicondyle. In these cases, the medial aspect of the humeral metaphysis and the ligament of Struthers form the boundaries of an osteofibrous tunnel which encircles the neurovascular bundle of the forearm (Fig. 5d). The radiographic appearance of the supracondylar process is characteristic but MR imaging is the technique of choice to image the ligament (Pecina et al. 2002). At US, transverse planes are the most adequate to display the supracondylar process. However, because this bony process is thin, difficulties may arise when the US beam is perpendicular to it. Tilting the probe anteriorly and posteriorly may be helpful to visualize it based on its posterior acoustic shadowing. The ligament may be even more difficult to see with US than the bony process. Once detected, a careful scanning technique is needed to rule out possible signs of entrapment of the median nerve and the brachial artery which course just deep to the ligament. A possible proximal bifurcation of the artery and, occasionally, of the nerve can be encountered together with supracondylar process (Gunther et al. 1993).
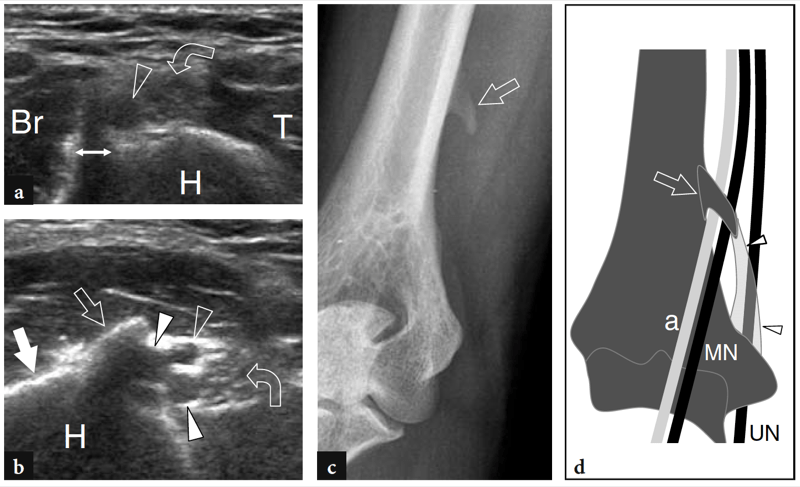
Fig. 5a–d. Supracondylar process and ligament of Struthers. a,b Transverse 12–5 MHz US images obtained over the supracondylar region in a patient referring a fi rm deep-seated local mass. a The brachial artery (open arrowhead) and the median nerve (curved arrow) are located just superficial to the medial aspect of the humeral shaft (H), between the brachialis (Br) and the triceps brachii (T) muscles. A small bony spur (double arrow) with posterior acoustic attenuation is shown anterior to the nerve and the artery. b More accurate probe positioning obtained by tilting the transducer anteriorly reveals a well-defined hyperechoic bony structure (open arrow) in continuity with the medial cortex of the humerus (white arrow) reflecting the supracondylar process. Note the close relationship of the bone process with the median nerve (curved arrow), the brachial artery (open arrowhead) and veins (white arrowheads). c Anteroposterior radiograph of the arm confirms the US diagnosis showing a typical supracondylar process (arrow). d Schematic drawing demonstrates the supracondylar process (arrow) and the ligament of Struthers (arrowheads) connecting it with the medial epicondyle. The brachial artery (a) and the median nerve (MN) can be seen passing through the supracondylar foramen, while the ulnar nerve (UN) lies outside it.
4. POSTERIOR ARM
The posterior compartment of the arm contains the large triceps muscle (Fig. 6). As its name indicates, the triceps consists of three heads: long, lateral and medial. The proximal tendon of the long head arises from the infraglenoid tubercle of the scapula and continues down with a large muscle belly located at the medial aspect of the arm (Fig. 6a); the lateral head and the medial head take their origin from the posterior aspect of the humerus, the first superior, the second inferior to the spiral groove of the radial nerve (Fig. 6b,c). Distally, the long and the lateral heads of the triceps converge to insert into a flat tendon that attaches to the olecranon process; the medial head inserts, for the most part, directly into the olecranon, but also on the medial aspect of the distal triceps tendon. The triceps muscle is a powerful extensor of the forearm; because the long head crosses the shoulder joint, it also plays a role as an extensor and adductor of the arm. For an adequate evaluation of the posterior arm, the patient is asked to sit on the bed with the examiner behind him/her. A slight degree of elbow flexion may be useful to stretch the distal myotendinous junction and the triceps tendon. Alternatively, the patient can lie prone, but this position is less comfortable, particularly for elderly subjects. Transverse US images are first obtained over the lateral aspect of the arm to display the lateral head (Fig. 7a,b). Visualization of the superficial long head and the deep medial head is obtained by shifting the transducer more medially (Fig. 7c–e).
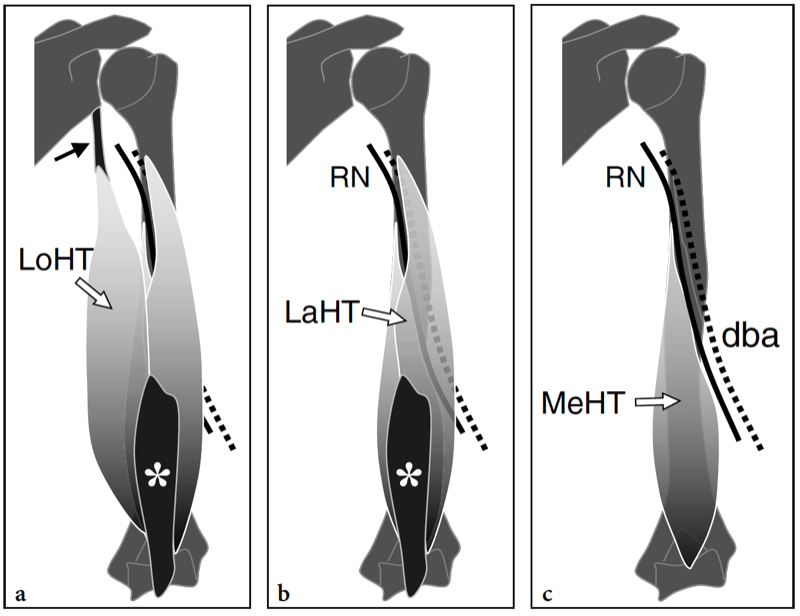
Fig. 6a–c. Schematic drawing of a coronal view of the posterior compartment of the arm illustrates the anatomy of the triceps brachii muscle and the radial nerve from surface (a) to depth (c). a–c The relationships among the three muscle bellies of the triceps – the long head (LoHT), the lateral head (LaHT) and the medial head (MeHT) – are shown. The bellies of the triceps muscle have separate origins and coalesce distally in a strong common tendon (asterisk) which inserts onto the posterior aspect of the olecranon. The long head arises from the infraglenoid tubercle through a strong tendon (black arrow), while the lateral and medial heads take their origin from the posterior aspect of the humeral shaft, the fi rst above, the second below the spiral groove. Note the radial nerve (RN, black line) and the satellite deep brachial artery (dba, dashed line) which course from medial to lateral inside the spiral groove, between the two heads.
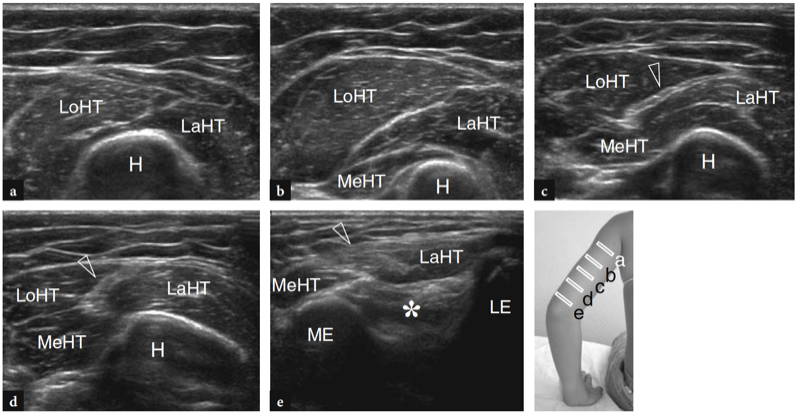
Fig. 7a–e. Triceps muscle. a–e Series of transverse 12–5 MHz US images obtained from cranial (a) to caudal (e) over the posterior aspect of the arm. a At the proximal arm, the long (LoHT) and the lateral head (LaHT) of the triceps can be demonstrated superficial to the humerus (H). The long head is located medial to the lateral head. b Sweeping the probe down from the level illustrated in a, the medial head (MeHT) can be seen arising from the posterior aspect of the humerus. It is the deepest component of the triceps. c At the middle arm, the three heads of the triceps dispose in two layers: superficial (including the long and lateral heads) and deep (consisting of the medial head). In the superficial layer, the eccentric distal aponeurosis of the long head is seen separating this muscle belly from the lateral head. d Moving the probe down toward the distal third of the arm, the conjoined tendon (arrowhead) of the long and the lateral heads is progressively appreciated. Observe the superficial position of this tendon relative to the deep medial head. e A more distal image over the olecranon fossa (asterisk) shows the distal triceps tendon (arrowhead) and the distal myotendinous junction of the medial and lateral heads. ME, medial epicondyle; LE, lateral epicondyle. The photograph at the bottom right of the figure indicates probe positioning.
The radial nerve originates from the posterior cord of the brachial plexus (C5–C8) and supplies the extensor muscles of the upper limb (i.e., the triceps, the lateral part of the brachialis, the brachioradialis, the forearm extensors) and the skin of the dorsal forearm and dorsolateral aspect of the hand. After leaving the axilla, this nerve enters the arm at the posterolateral aspect of the humeral shaft alongside the brachial artery, first between the coracobrachialis and the teres major and then between the bellies of the medial and lateral heads of the triceps. Then, it winds closely around the posterolateral aspect of the humeral shaft, passing in the spiral groove between the long and the lateral heads of the triceps accompanied by the deep brachial artery and vein (Fig. 6). More distally, the radial nerve pierces the lateral intermuscular septum and enters the anterior compartment of the arm coursing between the brachialis and brachioradialis muscles. Transverse US scans obtained with the patient seated in front of the examiner with the arm in internal rotation are the best to demonstrate the radial nerve, which courses adjacent to the bone along the posterolateral aspect of the humeral shaft (Fig. 8). The brachial artery, the coracobrachialis and the teres major muscles are useful landmarks to identify the radial nerve proximally in the arm. At the midhumerus, the normal radial nerve has a more oval, flattened cross-sectional profile within the spiral groove, as a result of its close relationship with the bone, and exhibits a well-defined fascicular echotexture (Bodner et al. 2001). The deep brachial artery is a useful landmark to identify it. In normal subjects, the measured diameters of the nerve in this area are 4.0–4.2 mm (LL) and 2.3–3.5 mm (AP) (Bodner et al. 2001).
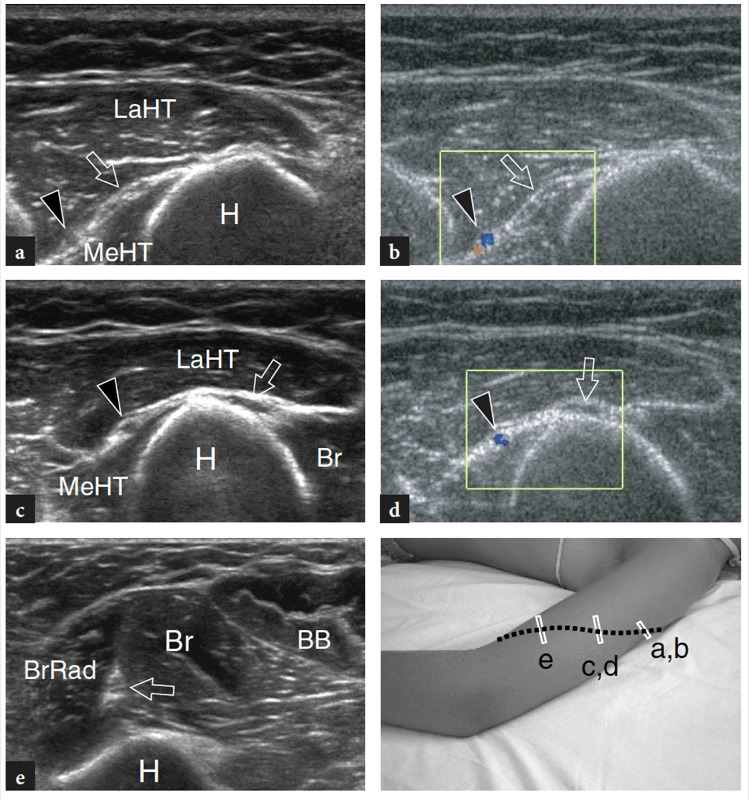
Fig. 8a–e. Radial nerve. a,b Transverse a gray-scale and b color Doppler 12–5 MHz US images obtained over the radial nerve at the proximal arm reveal the radial nerve (arrow) and the deep brachial artery (black arrowhead) running between the deep medial head (MeHT) and the more lateral and superficial lateral head (LaHT) of the triceps. H, humerus. c,d Transverse c grayscale and d color Doppler 12–5 MHz US images obtained at the middle third of the arm over the spiral groove of the humerus demonstrate the radial nerve (arrow) accompanied by the deep brachial artery (black arrowhead) crossing the humeral shaft in close contact with the bone. Br, brachialis muscle. e Transverse gray-scale 12–5 MHz US image obtained over the anterolateral aspect of the distal arm displays the radial nerve (arrow) running between the posterolateral brachioradialis (BrRad) and the anteromedial brachialis (Br). BB, biceps brachii muscle. The photograph at the bottom right of the figure indicates probe positioning over the course (dashed line) of the radial nerve.
5. NEUROVASCULAR BUNDLE
On the medial aspect of the arm, the brachial (humeral) artery and satellite veins (including the basilic vein and its tributaries), the median nerve and the ulnar nerve form the neurovascular compartment of the arm. This compartment is delimited on each side by a division of the medial intermuscular septum in an anterior layer covering the biceps and a posterior layer covering the triceps. The neurovascular bundle descends deep to the superficial fascia on the medial aspect of the arm in the so-called bicipital fossa, bordered by the coracobrachialis and the short head of the biceps laterally, and then the medial head of the triceps brachii posteriorly. At the proximal third of the arm, the median nerve is located superficial to the humeral artery and deep to the short head of the biceps, whereas the ulnar nerve lies posterior to the humeral artery, between it and the medial intermuscular septum (Fig. 9a,b). More causally, at the middle third of the arm, the median nerve crosses the artery to course along its medial aspect downward to enter the antecubital fossa (Fig. 9c–e). On the other hand, the ulnar nerve pierces the septum to enter the posterior compartment and here descends tightly bound to the medial head of the triceps to reach the cubital tunnel (Fig. 9d). The fascia of the medial head joins the medial intermuscular septum to form a thick band over the ulnar nerve. During their course through the arm, the median and ulnar nerves do not give off secondary branches. Transverse US images accurately disclose the relationships of the median and ulnar nerves with the humeral artery. Adequate pressure with the probe over the bicipital fossa may cause complete collapse of the veins and make the detection of the nerves easier. If distinguishing one nerve from the other is problematic, the examiner should remember that the median nerve runs adjacent to the brachial artery, whereas the ulnar nerve courses in close relationship with the triceps. As an alternative, a trick of the trade is scanning at the cubital tunnel level (where the ulnar nerve is easy to recognize) or in the antecubital fossa (where the median nerve can be readily identified on the medial side of the brachial artery) and then moving the probe up over the nerve on transverse planes.
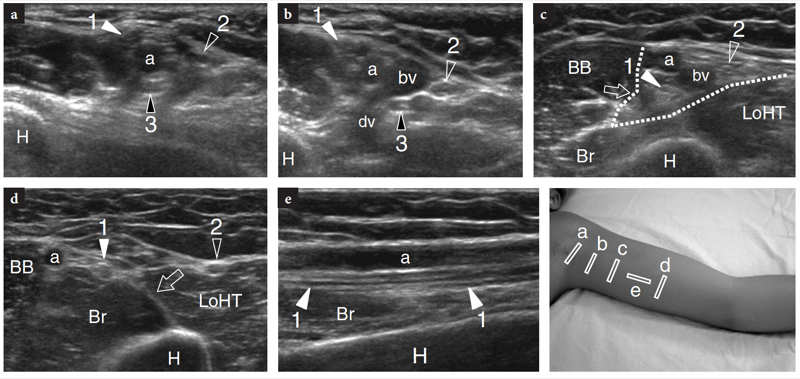
Fig. 9a–e. Neurovascular bundle of the arm. a–d Series of transverse 12–5 MHz US images obtained from cranial (a) to caudal (d) over the bicipital fossa. a At the proximal arm, the median (1, white arrowhead), ulnar (2, void arrowhead) and radial (3, black arrowhead) nerves are arranged all around the brachial artery (a). Based on the position of the artery, the median nerve is located anterior to it, the ulnar nerve posterior and the radial nerve more lateral and deep. H, humerus. b Slight more distally, note the confluence of the deep brachial vein (dv) with the basilic vein (bv). c At the middle third of the arm, the median nerve passes deep to the artery. Both median and ulnar nerves are located within a triangular fat-filled hyperechoic space delimited by a division of the medial intermuscular septum (dotted lines), between the anterior biceps brachii (BB) and the brachialis (Br) muscles and the posterior long head of the triceps (LoHT). d At the distal third of the arm, the median nerve reaches the medial side of the brachial artery and the ulnar nerve runs within the posterior compartment in close contact with the triceps. Note the posterior position of the ulnar nerve relative to the medial intermuscular septum (arrow). e Longitudinal 12–5 MHz US image over the bicipital fossa demonstrates the median nerve running parallel and deep to the brachial artery. On its long axis, the nerve exhibits parallel linear echoes corresponding to the nerve fascicles. The photograph at the bottom right of the figure indicates probe positioning.
6. ARM PATHOLOGY
Although musculoskeletal disorders affecting the muscles and tendons are unusual in the arm, there are peculiar pathologic conditions affecting the nerves of the upper limb along their course through the bicipital sulcus and the spiral groove area. These conditions include compressive neuropathies or traumatic injuries, which involve the median and the radial nerves more frequently than the ulnar and the musculocutaneous nerves. Anatomic constraints, related to the proximity of these nerves to the bone or the brachial artery, and variants, play a role as predisposing causes for nerve disease. In this clinical setting, US serves as an adjunct to electrodiagnostic testing and clinical evaluation for patient’s investigation. This technique also provides the surgeon with important information concerning surgical exploration and reconstruction.
7. ANTERIOR ARM: BICIPITAL SULCUS PATHOLOGY
Because the ulnar nerve is relatively unconstrained in the proximal arm, it is only exceptionally involved in entrapment syndromes at this site. In general, compression of this nerve in the upper arm relates to space-occupying lesions, such as large aneurysms of the brachial artery or anomalous muscles (e.g., chondroepitrochlearis muscle). On the other hand, the median nerve is subject to compression at different levels in the upper arm. Penetrating trauma during falls or glass wounds are most often responsible for nerve injury (Fig. 10). In these cases, the proximity of nerves and vessels in the bicipital sulcus leads to complex injuries with contemporary involvement of the median nerve, the brachial artery and veins, and possibly the ulnar nerve. Given the complexity of these traumas, it is not unusual to find patients sutured for vascular bleeding at the first surgical look and then submitted to US examination for a missed nerve transection. In the preoperative assessment of complete nerve tears, US is an accurate means to identify the level of the tear and to map the location of the nerve ends, that may be displaced and retracted from the site of the injury, based on the identification of hypoechoic stump neuromas. In this application, US has shown some advantages over MR imaging as a result of its higher spatial resolution capabilities for imaging a restricted area in which many nerves and vessels run close together. A peculiar type of iatrogenic median nerve injury can be observed at the midhumerus following brachial artery catheterization. In addition to traumas, compression of the median nerve in the bicipital sulcus may also occur at the distal humerus if a bony spur and ligament is present. When a mass is palpable over the bicipital sulcus, US is able to distinguish a neurogenic tumor from other soft tissue neoplasms based on the continuity of the mass with the parent nerve (Fig. 11). Furthermore, US may identify with certainty which is the nerve of origin (the median, the ulnar) of a neurogenic mass: an assessment not always easy on MR imaging, especially for large-sized tumors.
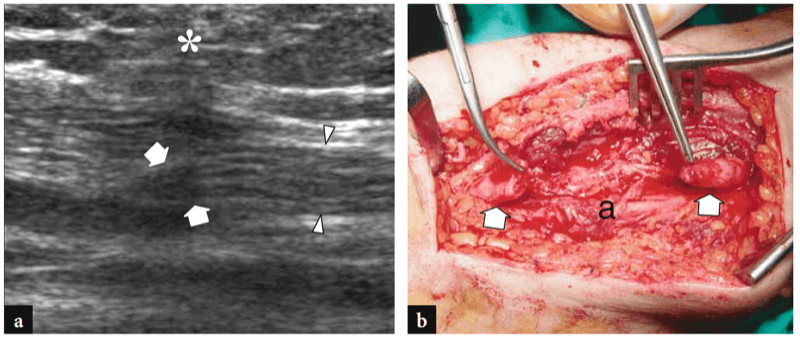
Fig. 10a,b. Median nerve transection at the middle third of the arm in a 14-year-old girl following a glass wound. a Long-axis 15–7 MHz US image over the bicipital sulcus demonstrates the median nerve (arrowheads) ending abruptly (arrows) at the level of the penetrating trauma. Note the heterogeneous appearance (asterisk) of the overlying subcutaneous tissue. In this particular case, the distal stump of the nerve was identified approximately 4 cm below. b Gross surgical view confirms the complete transection of the median nerve and the gap intervening between the stumps (arrows) measured preoperatively with US. The brachial artery (a) was undamaged.
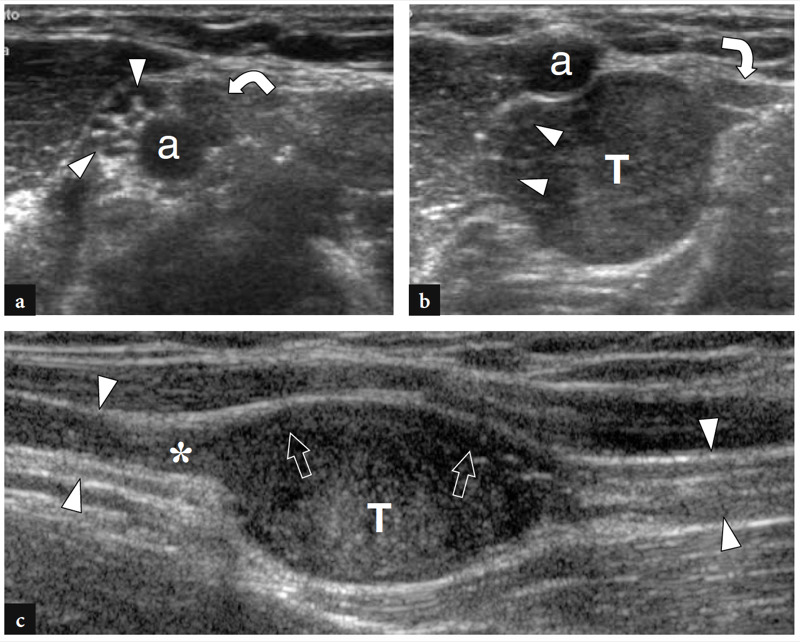
Fig. 11a–c. Schwannoma of the median nerve at the bicipital fossa. a,b Transverse 15–7 MHz US images obtained a just proximal to the tumor and b at the tumor level demonstrate an eccentric solid hypoechoic mass (T) in continuity with the fascicles of the median nerve (arrowheads). In b, note the brachial artery (a) and the ulnar nerve (curved arrow) displaced by the bulk of the tumor. c, Longitudinal 12–5 MHz US image depicts the tumor (T) connected at both ends with the median nerve (arrowheads). At its proximal end, the mass is in continuity with a swollen fascicle (asterisk), whereas the other fascicles (straight arrows) remain unaffected and appear displaced at the periphery of the mass. After surgical resection, pathologic examination revealed a schwannoma.
8. MEDIAN NEUROPATHY FOLLOWING BRACHIAL ARTERY CATHETERIZATION
In routine outpatients or in cases in which the femoral approach is not appropriate, the percutaneous brachial approach is a well-established alternative. The brachial approach is safe with a low complication rate. Nevertheless, the close proximity of the brachial artery to the median nerve, the mobility of the brachial artery in the arm, as well as the winding unpredictable course of the nerve, which lies at first lateral to the artery and then crosses to its medial side, allow the possibility of incidental median nerve injury during a catheterization procedure. This complication seems more likely in patients under anticoagulation therapy (Chuang et al. 2002). Clinically, the onset of a neuralgic tingling sensation and paresthesias radiating from the elbow to the first three fingers suggests nerve irritation and damage. Needle injury may result in epineurial hemorrhage leading to compression of the fascicles and impaired nerve function (Macon and Futrell 1973). US and Doppler imaging are useful to identify the hematoma enclosed in the epineurium and the displaced fascicles (Chuang et al. 2002). In this setting, US may have a role in distinguishing an epineurial hemorrhage from a traumatic neuroma, an extrinsic collection or a pseudoaneurysm of the brachial artery. In epineurial hemorrhage, the collection is typically aligned between the artery and the fascicles, which are eccentrically displaced (Fig. 12). On the contrary, traumatic neuromas appear as fusiform hypoechoic areas encasing most nerve fascicles but not displacing them. Extrinsic collections are usually larger in size and may cause major nerve displacement. Finally, pseudoaneurysms appear as pulsatile sacs in continuity with the injured artery by means of a neck. Color Doppler imaging can help the diagnosis by showing whirling blood flow within the sac and “to-and-fro” waveforms at the arterial neck indicating communication with the artery (Fig. 13). In patients with onset of neuralgic symptoms, US can successfully guide the percutaneous aspiration of the hematoma to obtain an early decompression of the fascicles (Chuang et al. 2002).
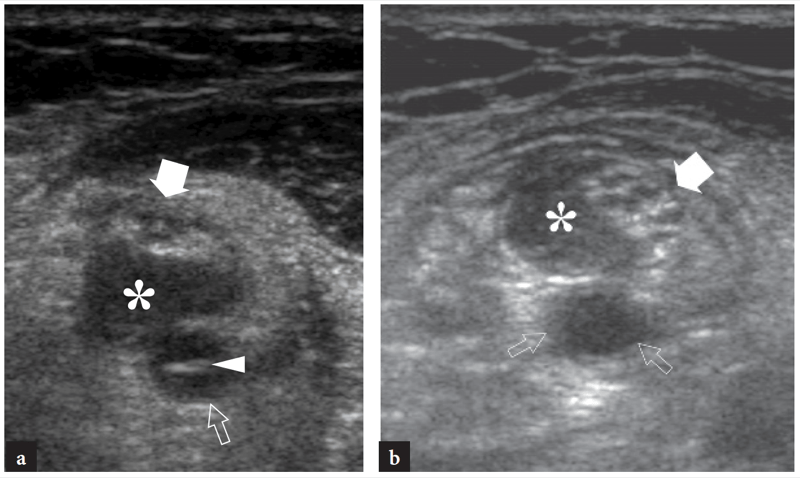
Fig. 12a,b. Epineurial hematoma of the median nerve in a patient with vertebrobasilar insufficiency who underwent brachial artery catheterization for carotid and vertebral artery evaluation and developed symptoms of median neuropathy after the angiographic procedure. a,b Transverse 15–7 MHz US images obtained at the puncture site reveal a small hematoma (asterisk) intervening between the brachial artery (small arrows) and the displaced fascicles of the median nerve (large arrow). In a, an intimal flap (arrowhead) floating within the arterial lumen is visible.
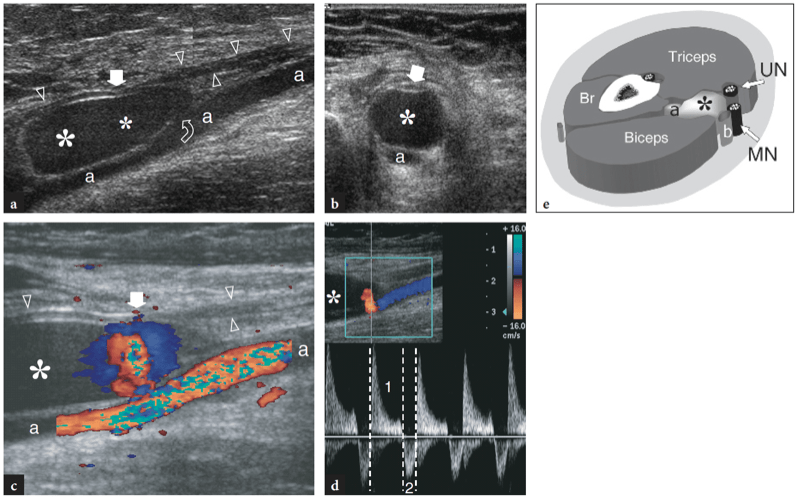
Fig. 13a–e. Postangiographic pseudoaneurysm of the brachial artery in patient presenting with a pulsatile lump in the bicipital fossa and clinical signs of median neuropathy. a Longitudinal and b transverse gray-scale 12–5 MHz US images obtained over the brachial artery (a) demonstrate the hypoechoic sac (asterisks) of the pseudoaneurysm in continuity with the artery by means of a thin neck (curved arrow). The median nerve (arrowheads) appears markedly flattened (arrow) over the pseudoaneurysm reflecting extrinsic compression. c Longitudinal color Doppler 12–5 MHz US image reveals whirling flow within the sac in continuity with the artery. d Spectral Doppler analysis obtained in the communicating tract displays bidirectional velocities as the forward flow in systole (1) is ejected in diastole (2). e Schematic drawing illustrates the relationships of the pseudoaneurysms (asterisk) of the brachial artery (a) with the median (MN) and ulnar (UN) nerves. b, basilic vein; Br, brachialis.
9. SUPRACONDYLAR PROCESS SYNDROME
In individuals with a supracondylar process, the median nerve and, in rare instances, the ulnar nerve can be compressed in an osteofibrous tunnel created by a firm fibrous band with a vertical course, commonly referred to as the “ligament of Struthers”, which joins the anomalous bony process and the medial epicondyle. Clinically, this condition typically affects young sportsmen as a result of intense muscular activity in the elbow and forearm and may start with pain and numbness in the first three fingers and weakness of forearm muscles innervated by the median nerve (Sener et al. 1998). US can demonstrate the relationship of the median nerve with the anomalous bone and ligament. Although not yet reported in the radiological literature, displacement of the nerve by these structures may represent an indicator of entrapment. Therapy includes excision of the ligament of Struthers and ablation of the supracondylar process. The brachial artery can also be compressed by an anomalous insertion of the pronator teres muscle into the supracondylar process (Talha et al. 1987).
10. POSTERIOR ARM: SPIRAL GROOVE SYNDROME
Within the spiral groove, the close relationship of the radial nerve with the humeral cortex and its fixity as it penetrates the lateral intermuscular septum makes it vulnerable to extrinsic pressure. Clinically, radial nerve entrapment at the middle arm is characterized by combined features of both superficial radial nerve and posterior interosseous nerve palsy. Radial nerve palsy essentially results in wrist-drop due to denervation of the forearm extensors, whereas the triceps muscle (acting on forearm extension) is usually spared because its innervation arises above. Sensory loss over the dorsolateral forearm and hand maybe associated. The main causes of radial nerve compression in the spiral groove include axillary crutches, pressure on a wheelchair armrest and improper positioning of the arm such as occurs when an individual falls asleep leaning against a hard surface following drug- or alcohol-induced stupor, the so-called Saturday night palsy. Strenuous physical activity has also been implicated as a possible cause of radial nerve injury in patients with fibrous bands arising from either the lateral or long head of the triceps. Most of these cases recover fully within a few days or weeks. Recovery may be delayed by several months and occasionally may be incomplete. In a more severe traumatic setting, and especially in patients with closed traction injuries, usually associated with fractures of the midshaft of the humerus, there may be direct contusion and laceration of the nerve by fracture fragments. In general, the surgical outcome of radial nerves lacerated by tidy wounds or traction is better than that of nerves damaged by humeral fractures. A severe traction rupture of the radial nerve, with a gap between the stumps exceeding 10 cm, is best treated by musculotendinous flexor-to-extensor transfer. Furthermore, if the interval since injury exceeds 1 year, transfer is more likely to improve function (Shergill et al. 2001).
Somewhat similar to other sites of nerve entrapment, the main signs of radial nerve impingement in the spiral groove are a swollen nerve with a uniformly hypoechoic appearance and loss of the fascicular pattern (Bodner et al. 1999, 2001). In entrapment syndromes due to fibrous bands arising from the adjacent bellies of the triceps, abrupt changes in the nerve cross-sectional area at the site of compression and direct visualization of the constricting fibrous band can be seen with US (Fig. 14). In contusion traumas, the nerve fascicles may appear focally swollen and hypoechoic and the fat space surrounding the nerve thickened and diffusely hyperechoic (Fig. 15). In malaligned or fragmented fractures of the midshaft of the humerus, the radial nerve can be seen displaced on the edge of fracture fragments or pinched in between them (Fig. 16) (Bodner et al. 1999, 2001; Peer et al. 2001; Martinoli et al. 2004). In addition, it may appear encased or displaced by a hypertrophied callus and scar tissue. In the postoperative setting, the radial nerve may be stretched over orthopedic hardware for osteosynthesis. In patients with onset of progressive radial nerve palsy after internal fixation of a humeral shaft fracture with a compression plate, the conflict of the nerve with the metallic plate can be nicely depicted and US may be helpful in deciding whether early surgical treatment has to be instituted (Peer et al. 2001; Martinoli et al. 2004). In these cases, US reveals the dislocation of the compression plate and the thinning or thickening of the nerve which rides on the detached proximal end of the plate (Fig. 17). These findings indicate the need for a second surgical look for recovery of the nerve function. Space-occupying masses arising in the spiral groove are rare and may be nonpalpable even if large due to their deep location. Similar to the bicipital fossa, neurogenic tumors involving the radial nerve can be encountered in the spiral groove area (Fig. 18).
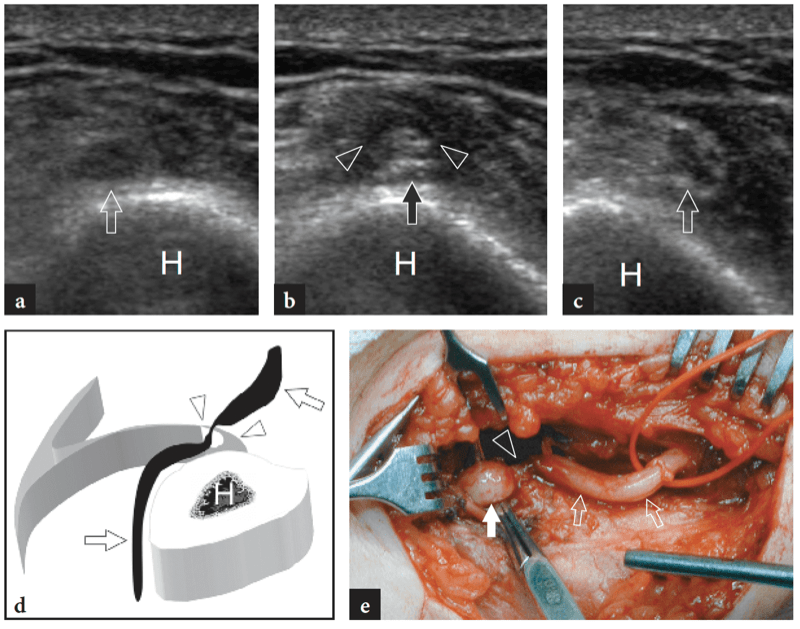
Fig. 14a–e. Radial nerve entrapment secondary to a constricting fibrous band in the spiral groove area. a–c Series of transverse 12–5 MHz US images obtained a just proximal to, b at the level of and c just distal to the compression point with d schematic drawing correlation. In b an abrupt flattening of the radial nerve (arrow) compared with its swollen, hypoechoic appearance visible a proximally and c distally is observed under an arc-shaped hypoechoic fibrous band (arrowheads). H, humerus. e Gross operative view showing, after release of the fibrous band, the site of constriction (arrowhead) of the radial nerve (open arrows). Note the swollen nerve portion (white arrow) ahead of the compression point.
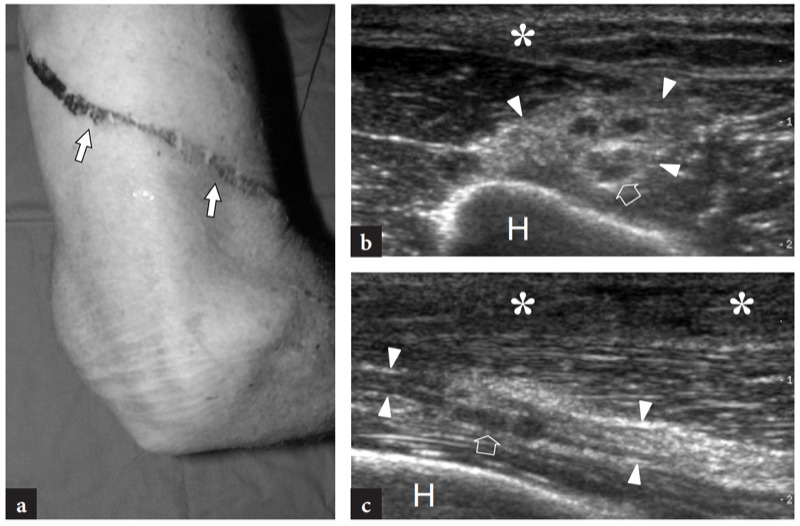
Fig. 15a–c. Severe radial neuropathy after contusion trauma on a metallic grid. a Photograph over the posterolateral aspect of the arm showing a deep linear abrasion (arrows) on the patient’s skin following traumatic contact on a metallic wire during a fall. b Transverse and c longitudinal 12–5 MHz US images over the spiral groove area reveal echotextural abnormalities (asterisks) of the subcutaneous tissue related to the contusion trauma. Over the humeral shaft (H), the radial nerve (arrowheads) exhibits a thickened epineurium and some abnormally swollen fascicles (arrow) reflecting a contusion trauma.
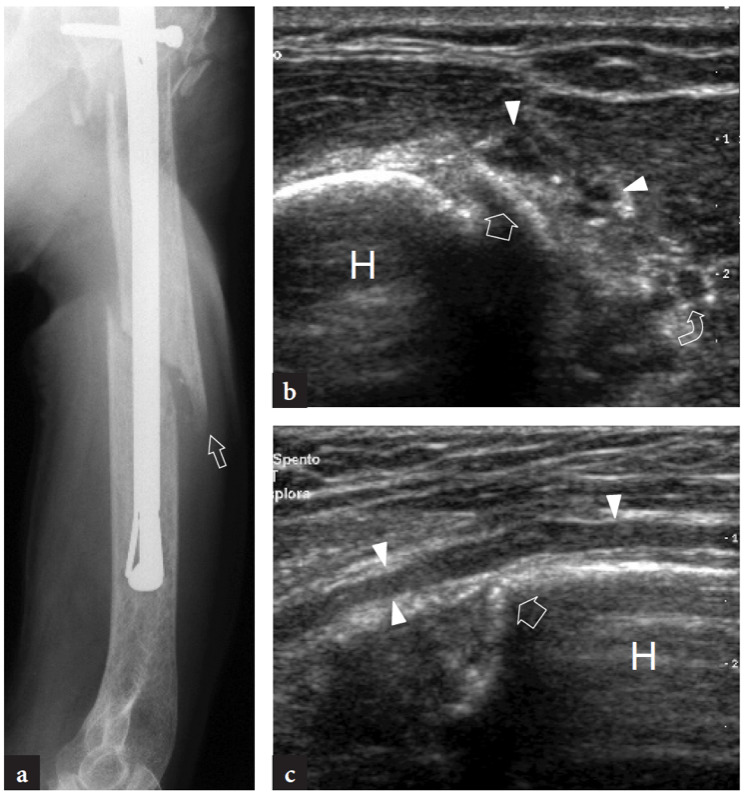
Fig. 16a–c. Radial nerve entrapment in the spiral groove by a displaced fracture fragment. a Radiograph shows a fracture of the humeral shaft treated with osteosynthesis. Note the displacement of the disrupted proximal part of the bone (arrow). b Longitudinal and c transverse 12–5 MHz US images reveal the radial nerve (arrowheads) that rides on the tip (arrow) of the fracture edge (arrow) of the humerus (H). Although continuous at the area of the fractured bone, the nerve appears swollen and hypoechoic as a possible result of stretching and contusion injury. Curved arrow, deep brachial artery.
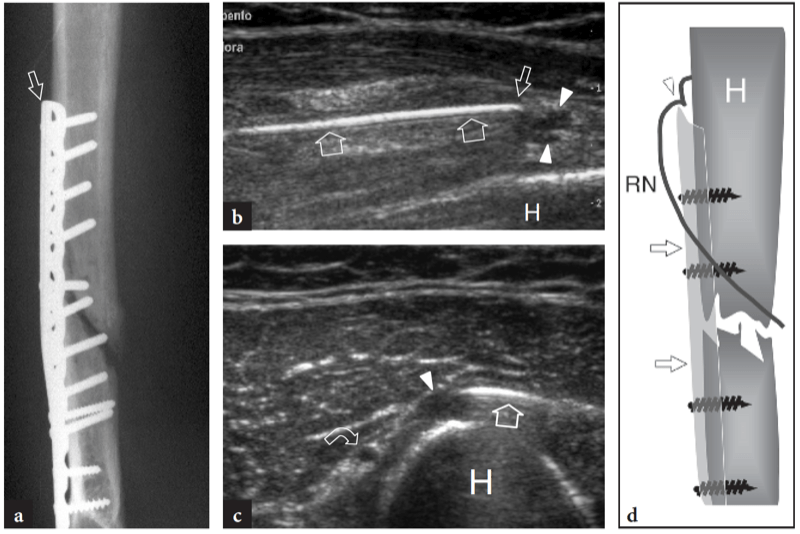
Fig. 17a–c. Radial nerve entrapment in the spiral groove after repair of a midshaft fracture of the humerus. a Radiograph reveals osteosynthesis for a humeral shaft fracture. Observe the elevation of the proximal edge (arrow) of the compression plate over the humeral cortex. b Longitudinal and c transverse 12–5 MHz US images show the radial nerve (arrowheads) stretched and flattened across the tip (small arrow) of the loose metallic plate (large arrow). At US, the compression plate can be distinguished from the underlying humerus (H) based on the presence of the reverberation artifacts of metals. Curved arrow, deep brachial artery. d Correlative schematic drawing of the same case illustrates the conflict of the nerve (RN) with the tip (arrowhead) of the plate (arrows).
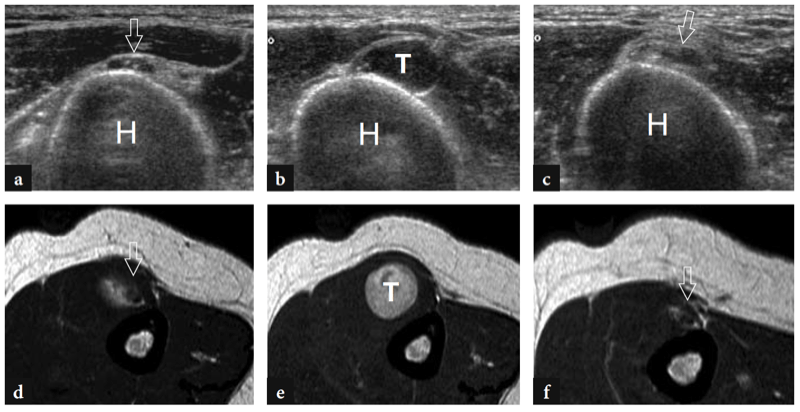
Fig. 18a–f. Schwannoma of the radial nerve at the spiral groove. a–c Transverse 12–5 MHz US images obtained a just proximal to the tumor, b at the tumor level and c just distal to the tumor with d–f T2-weighted MR imaging correlation demonstrate a hyperintense solid mass (T) in continuity with the fascicles of the radial nerve (arrows). Note the close proximity of the mass and the parent nerve with the humerus (H).