With surgical techniques advancing and the stakes for neurological outcomes rising, intraoperative monitoring (IOM) of the central and peripheral nervous systems is now essential. In a comprehensive 2024 review in the British Journal of Anaesthesia, Ryalino et al. break down the latest modalities, from raw EEG to transcranial Doppler (TCD), helping anesthesiologists navigate real-time neurophysiological data to protect patients’ brains and spinal cords.
Why intraoperative monitoring matters
- Protects against irreversible neurological damage
- Facilitates early detection of ischemia or nerve injury
- Supports titration of anesthetic depth and analgesia
- Informs shunt placement during carotid procedures
- Aids in reducing postoperative complications like delirium
-
Electroencephalography (EEG)
Raw EEG: the basics
EEG records cortical electrical activity via scalp electrodes, capturing voltage changes from synchronized neuronal firing, especially from pyramidal neurons.
Key frequency bands:
- Delta (0.5–4 Hz): deep anesthesia, coma
- Theta (4–8 Hz): sedation, sleep stages
- Alpha (8–13 Hz): relaxed wakefulness, seen in propofol sedation
- Beta (13–30 Hz): alertness; may increase with nociceptive arousal
Burst suppression:
- Alternating isoelectric periods and bursts of activity
- Indicates profound brain inactivation
- Associated with overdosage, deep hypothermia, or brain injury
Clinical uses:
- Seizure detection (esp. in awake craniotomies)
- Detection of cerebral ischemia (e.g., during carotid clamping)
- Titration of hypnotic agents
Processed EEG (pEEG): tools & limitations
Commonly used pEEG devices include:
- BIS
- SedLine
- qCON/qNOX (Fresenius-Kabi)
Indices guide depth of anesthesia, but:
- Are drug- and age-sensitive
- May miss burst suppression
- Should always be interpreted with the raw EEG
-
Intraoperative neurophysiological monitoring (IONM)
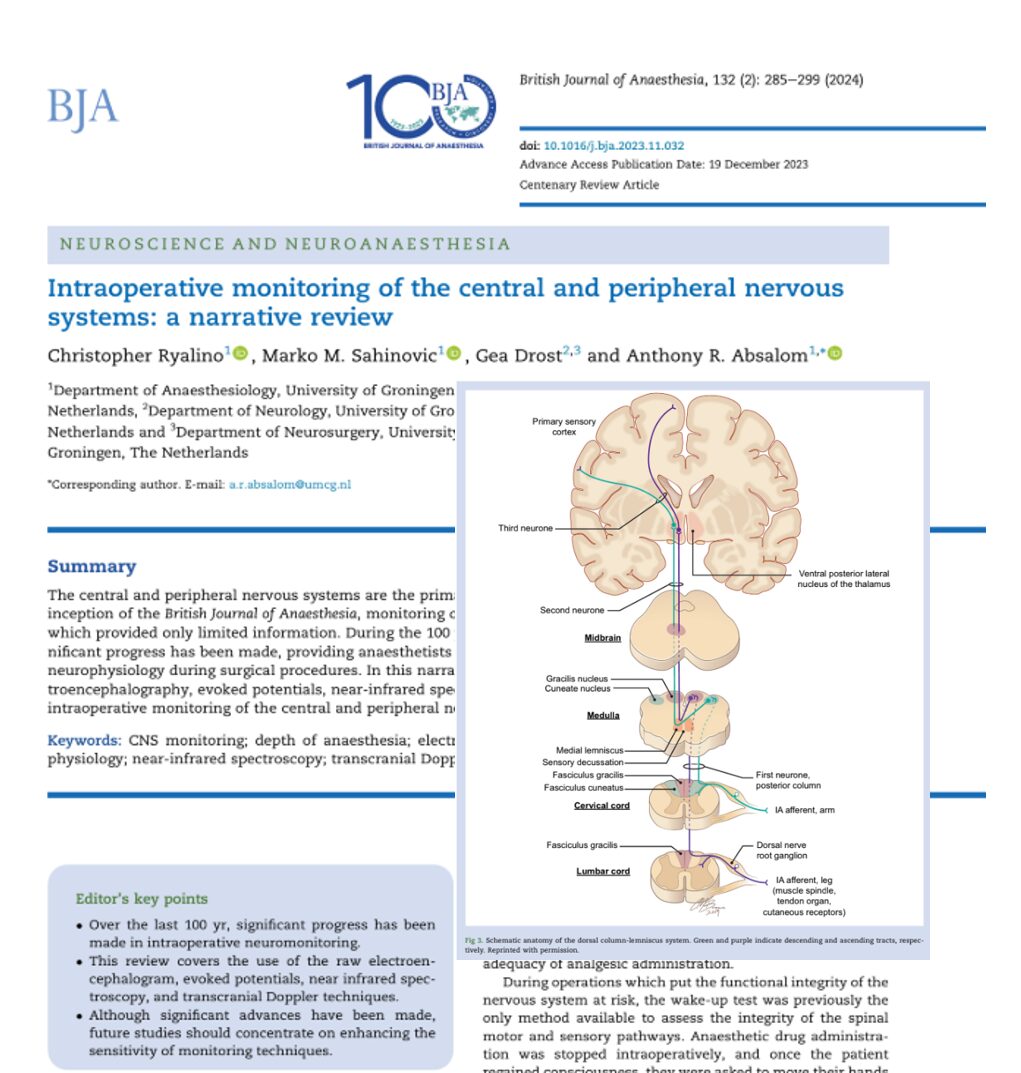
IONM assesses the integrity of spinal and cranial pathways during surgery.
Common modalities:
- Somatosensory-evoked potentials (SSEPs): Ascending dorsal column pathway
- Motor-evoked potentials (MEPs): Descending corticospinal tract
- Brainstem auditory-evoked potentials (BAEPs): Brainstem and cranial nerves
- Free-running EMG: Real-time muscle activity
Anesthesia tips for IONM
- Use TIVA with propofol—it preserves evoked responses better than volatile agents.
- Avoid neuromuscular blockers after intubation—especially for MEPs.
- Avoid bolus dosing of hypnotics or opioids—steady plasma levels prevent signal suppression.
- Use target-controlled infusions (TCI) to stabilize anesthesia depth.
- Place bite blocks when MEPs are used—to prevent injury during jaw contractions.
-
Near-infrared spectroscopy (NIRS)
NIRS measures regional cerebral oxygenation (ScO₂) non-invasively.
How it works:
- Detects differences in absorption between oxy- and deoxyhemoglobin
- Uses assumptions (e.g., 70:30 venous-to-arterial ratio)
Common thresholds for intervention:
- Absolute ScO₂ <55%
- 20% drop from baseline
Clinical uses:
- Cardiac surgery (esp. aortic arch or pediatric cases)
- Carotid endarterectomy
- Sitting beach chair position surgeries
Advantages:
- Easy to apply
- Real-time data
- No specialist needed
Limitations:
- Affected by extracranial tissues
- Influenced by skin color, hematomas, dye, and COHb
- Device-dependent; no standardisation of thresholds
-
Transcranial Doppler (TCD)
TCD uses ultrasound to measure cerebral blood flow velocity (CBFV) in large arteries.
Applications:
- Carotid clamping: >90% drop in CBFV = high stroke risk
- Hyperperfusion syndrome detection after endarterectomy
- Emboli detection in cardiac/aortic surgeries
- Perfusion monitoring during bypass
Interpretation tips:
- MCA velocity 35–90 cm/s = normal range
- The Lindegaard index (MCA/ICA velocity ratio) helps differentiate hyperemia from vasospasm
Limitations:
- Operator dependent
- Insonation angle matters
- Not all patients have usable acoustic windows
- Provides large-vessel flow only—not microcirculation

Key takeaways for anesthesiologists
- Choose anesthesia carefully for IONM—TIVA with TCI is best.
- Use multimodal monitoring in high-risk cases (EEG + NIRS or TCD).
- Train in EEG interpretation—raw EEG reveals what indices can’t.
- NIRS and TCD offer value, but have technical and physiological limitations.
- Interpret signals in context—consider surgical events, drugs, and physiology before reacting.
Final thoughts
Neuromonitoring is no longer a niche tool—it’s an essential pillar of modern anesthetic practice. As the evidence base evolves and technology advances, anesthesiologists must stay engaged, informed, and trained to leverage these systems for safer, smarter surgeries.
Reference: Ryalino C et al. Intraoperative monitoring of the central and peripheral nervous systems: a narrative review. Br J Anaesth. 2024;132:285-299.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant App. Prefer a physical copy? Get the latest literature and guidelines in book format. For an interactive digital experience, check out the Anesthesia Updates Module on NYSORA360!