Learning objectives
- Describe the risk factors and pathophysiology of TRALI
- Diagnose and manage TRALI
- Prevent TRALI
Background
- Transfusion-related acute lung injury (TRALI) is a transfusion reaction characterized by an acute, noncardiogenic pulmonary edema associated with hypoxia
- The leading cause of death from transfusion
- Caused by damage to pulmonary vasculature due to the immune response to antibodies or proinflammatory factors from the transfusion product that bind to antigens of the recipient
- Symptoms include acute dyspnea, fever, hypotension, and tachycardia
Risk factors
- Mechanical ventilation
- Sepsis
- Massive transfusion
- Coronary artery bypass graft
- End-stage liver disease
- Positive fluid balance
- Critically ill patient
- Blood products with high plasma contents
Pathophysiology
- Two-hit hypothesis:
- Threshold hypothesis
- No first hit, a threshold must be overcome to induce TRALI
- Threshold depends on the susceptibility of the patient and the quantity of antibodies/proinflammatory factors in the transfusion product
Diagnosis
- Diagnostic criteria:
- Symptoms develop during or within 6 hours of transfusion without any risk factors for developing acute lung injuries (sepsis from pneumonia, aspiration, shock)
- Clinical findings:
- Exudative bilateral infiltrates on chest radiograph
- No evidence of pulmonary vascular overload
- Hypoxemia: SpO2 <90% on room air, ratio of partial oxygen pressure to fractional inspired oxygen concentration <300 mmHg
- Possible TRALI: Other risk factors for acute lung injury
- Delayed TRALI: 6 – 72 hours after transfusion
Differential diagnosis
- Septic transfusion reaction: Signs of sepsis
- Anaphylactic transfusion reaction: Laryngeal and bronchial edema
- Transfusion-related circulatory overload: Increased pulmonary artery occlusion pressure (>18 mmHg)
Treatment
- There is no treatment, management is supportive
- Stop transfusion
- Additional oxygen
- Restrictive tidal volume ventilation
- Diuretics may be considered
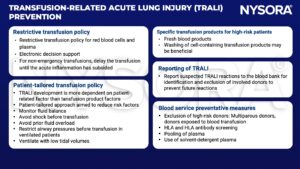
Prevention
Suggested reading
- Cho MS, Modi P, Sharma S. Transfusion-related Acute Lung Injury. [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507846/
- Vlaar AP, Juffermans NP. Transfusion-related acute lung injury: a clinical review. Lancet. 2013;382(9896):984-994.
We would love to hear from you. If you should detect any errors, email us [email protected]