Learning objectives
- Describe the physiological changes associated with pregnancy and their anesthetic implications
- Describe the anesthetic implications of commonly used medications
- Manage obstetric patients presenting for non-obstetric surgery
Background
- Non-obstetric surgery may be required at any trimester during pregnancy, which carries the unique challenge of caring simultaneously for two patients
- Understanding the physiological changes of pregnancy is essential for safe anesthesia
- Most common indications: Acute appendicitis, cholecystitis, trauma, and surgery for maternal malignancies
- Main risks: Fetal loss, premature labor, and delivery
Physiological changes & implications
| System | Physiological change | anesthetic implications |
|---|---|---|
| Cardiovascular | Increased cardiac output by up to 50% Increased uterine perfusion up to 10% of cardiac output Decreased systemic vascular resistance, pulmonary vascular resistance, and arterial pressure Aortocaval compression from 13 weeks | Uterine perfusion not autoregulated Hypotension common under regional and general anesthesia Supine hypotensive syndrome requires left lateral tilt |
| Respiratory | Increased minute ventilation Respiratory alkalosis Decreased expiratory reserve volume, residual volume, and functional residual capacity Ventilation/perfusion mismatch Increased oxygen consumption Upward displacement of diaphragm Increased thoracic diameter Mucosal edema | Potential hypoxemia in the supine and Trendelenburg positions Breathing more diaphragmatic than thoracic Difficult laryngoscopy and intubation; bleeding during attempts |
| Central nervous system | Epidural vein engorgement Decreased epidural space volume Increased sensitivity to opioids and sedatives | More extensive local anesthetic spread |
| Hematological | 30% red cell volume increase Increased white blood cell count 50% plasma volume increase Increased coagulation factors Decreased albumin and colloid osmotic pressure | Dilutional anemia Thromboembolic complications Edema, decreased protein binding of drugs |
| Gastrointestinal | Increased intragastric pressure Decreased barrier pressure | Increased aspiration risk Antacid prophylaxis, RSI after 18 weeks gestation |
| Renal | Increased renal plasma flow and glomerular filtration rate Decreased reabsorptive capacity | Normal urea and creatinine may mask impaired renal function Glycosuria and proteinuria |
Medication side-effects & anesthetic implications
| Medication | Side-effects and anesthetic implications |
|---|---|
| Volatile agents | Decreased MAC, reduced uterine tone, hypotension |
| Nitrous oxide | Prolonged exposure may inhibit DNA synthesis; avoid in the first trimester |
| Succinylcholine | Reduced plasma cholinesterase, possible prolonged action |
| Non-depolarizing neuromuscular blocking agents | Quaternary ammonium compounds do not cross the placenta |
| Local anaesthetics | Reduced protein-binding, increased risk of toxicity; use lower intrathecal doses in late pregnancy |
| Opioids | Increased maternal sensitivity, fetal withdrawal, intrauterine growth restriction with chronic use |
| Non-steroidal anti-inflammatory drugs | Premature ductus arteriosus closure, avoid after 28 weeks; ketorolac contraindicated |
| Warfarin | Teratogenic, crosses the placenta |
| Heparin | Does not cross the placenta |
| Atropine | Fetal tachycardia, crosses the placenta |
| Glycopyrrolate | Quaternary ammonium compound, does not cross the placenta |
| Phenytoin, carbamazepine, sodium valproate | Congenital malformations (neural tube defects) |
| Magnesium sulphate | Muscle weakness, interaction with neuromuscular blocking agents |
| ACE inhibitors | Intrauterine growth restriction, oligohydramnios, renal impairment |
| Beta-blockers | Intrauterine growth restriction, neonatal hypoglycemia, bradycardia |
| Thiazides | Neonatal thrombocytopenia |
| Beta-2-agonists: ritodrine, terbutaline, salbutamol | Tachyarrhythmias, pulmonary edema, hypokalemia, hyperglycemia |
| Oxytocin receptor antagonists: atosiban | Nausea, vomiting, fewer side-effects than beta-2-agonists |
| Calcium-channel blockers: nifedipine | Hypotension, fewer side-effects than beta-2-agonists |
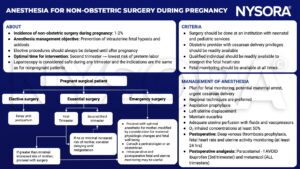
Management
Suggested reading
- Haggerty E, Daly J. Anaesthesia and non-obstetric surgery in pregnancy. BJA Education. 2021;21(2):42-3.
- Nejdlova M, Johnson T. Anaesthesia for non-obstetric procedures during pregnancy. Continuing Education in Anaesthesia Critical Care & Pain. 2012;12(4):203-6.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







