Learning objectives
- Describe osteogenesis imperfecta
- Recognize signs and symptoms of osteogenesis imperfecta
- Anesthetic management of a patient with osteogenesis imperfecta
Definition and mechanisms
- Osteogenesis imperfecta (OI), or brittle bone disease, is a group of genetic disorders present at birth, characterized by fragile bones that break easily
- The underlying mechanism is usually a connective tissue disorder caused by a lack of or poorly formed type I collagen
- In more than 90% of the cases, OI occurs due to mutations in the COL1A1 and COL1A2 genes
- Inherited in an autosomal dominant manner or de novo mutations
| Types | OI syndromic names | Clinical features | Radiographic or histological features |
|---|---|---|---|
| Type I | Nondeforming OI with blue sclera | Blue sclera Normal stature Fractures Hearing loss Presence of DI rare | Fractures |
| Type II | Perinatally lethal OI | Perinatal lethal Blue-gray sclera Small for gestational age Respiratory distress Limb deformities “Frog leg” positioning Soft calvarium | Multiple fractures “crumpled appearance” Beaded ribs Short thoracic cage Osteopenia Long bone deformities Limited calvarial mineralization |
| Type III | Progressively deforming OI | Severe phenotype Short stature Multiple fractures Progressive deformities Usually non-ambulatory May have DI Adolescent onset hearing loss | Osteopenia Multiple fractures Long bone deformity Thin ribs |
| Type IV | Common variable OI with normal sclera | Milder than OI III Typically ambulatory DI is common Adult onset hearing loss Normal-gray sclera | Intermediate appearance between OI II and III |
DI, dentinogenesis imperfecta
Signs and symptoms
Signs and symptoms vary from mild to severe
- Bones that break easily, brittle bones
- Bone deformity and pain
- Easy bruising
- Blue sclera
- Joint hypermobility
- Loose joints
- Muscle weakness
- Curved spine, kyphoscoliosis
- Short height
- Hearing loss
- Dentinogenesis imperfecta (weak, brittle, or discolored teeth)
- Difficulty breathing
- Triangle-shaped face
Complications
- Respiratory infections (e.g., pneumonia)
- Pulmonary valve insufficiency secondary to distortion of the ribcage
- Cardiovascular problems (e.g., valvular disease, aorta dissection)
- Kidney stones
- Vision loss
Treatment
Treatment focuses on managing symptoms and increasing bone strength to prevent deformities and fractures
- Maintain a healthy lifestyle via exercise, eat a balanced diet sufficient in vitamin D and calcium, and avoid smoking
- Biphosphonate medicines
- Acute care of fractures
- Orthopedic treatment (e.g., bracing and splinting)
- Rodding surgery
- Physical and occupational therapy
- Assistive devices (e.g., leg braces and wheelchairs)
- Oral and dental care
Anesthetic concerns
| Types | Anesthetic concerns |
|---|---|
| Type I | Bone fractures during extremity manipulation (e.g., positioning, peripheral IV placements with tourniquet) Dental damage during oropharyngeal instrumentation Difficulty of hearing Hyperthermia or malignant hyperthermia Platelet dysfunction Capillary fragility |
| Type II | Most prenatally diagnosed pregnancies are terminated; patients rarely survive to adulthood |
| Type III | Bone fractures during extremity manipulation Posterior fossa compression syndromes due to basilar impression from cervical manipulation Pulmonary insufficiency or hypertension Cardiopulmonary failure Hyperthermia or malignant hyperthermia Platelet dysfunction Capillary fragility Postoperative pain control |
| Type IV | Bone fracture or dislocation Dental damage Posterior fossa compression syndromes Pulmonary insufficiency or hypertension Cardiopulmonary failure Hyperthermia or malignant hyperthermia Platelet dysfunction Postoperative pain control |
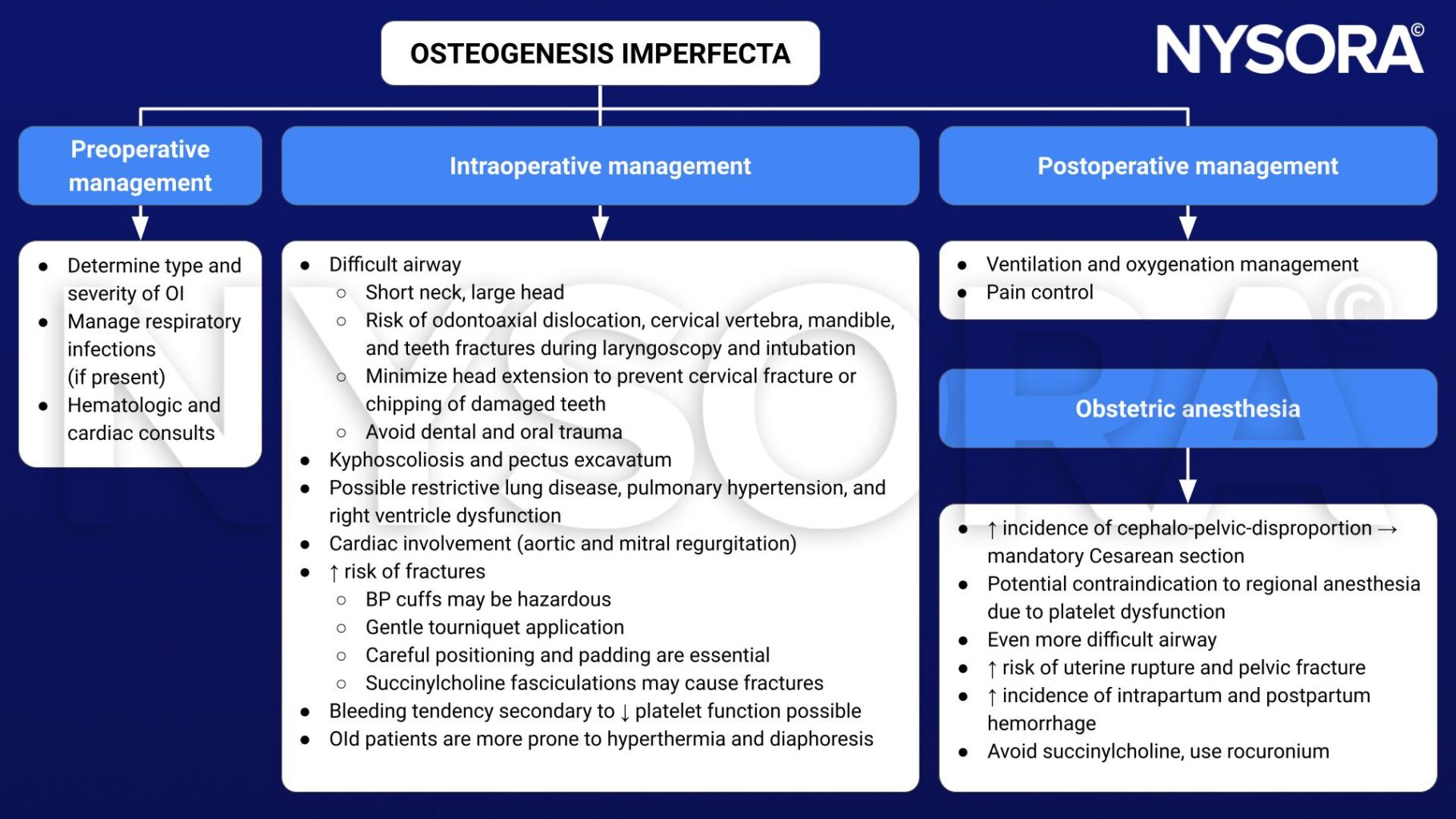
Management
Suggested reading
- Wang H, Huang X, Wu A, Li Q. Management of anesthesia in a patient with osteogenesis imperfecta and multiple fractures: a case report and review of the literature. Journal of International Medical Research. 2021;49(6).
- Gupta D, Purohit A. Anesthetic management in a patient with osteogenesis imperfecta for rush nail removal in femur. Anesth Essays Res. 2016;10(3):677-679.
- Frost EAM. Osteogenesis imperfecta and anesthetic implications. October 21, 2019. Accessed January 27, 2023. https://anesthesiaexperts.com/uncategorized/16596/#:~:text=In%20OI%2C%20the%20need%20for,or%20chipping%20of%20damaged%20teeth.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







