Learning objectives
- Define gestational diabetes
- Describe the complications associated with gestational diabetes
- Management of gestational diabetes
Definition and mechanisms
- Gestational diabetes is diabetes diagnosed for the first time during pregnancy, resulting in hyperglycemia affecting the pregnancy and baby’s health
- It can happen at any stage of pregnancy but most commonly develops in the second or third trimester
- Usually disappears after giving birth
- Occurs when the body cannot produce enough insulin to meet the extra needs in pregnancy
Signs and symptoms
Gestational diabetes does not usually cause any noticeable signs or symptoms
- Hyperglycemia
- Antenatal glycosuria
- Increased thirst
- More frequent urination
- Dry mouth
- Tiredness
- Blurred eyesight
- Genital itching or thrush
Complications
Maternal
- Gestational hypertension and pre-eclampsia
- Caesarean section
- Gestational diabetes in future pregnancies
- Type 2 diabetes
Fetal
- Excessive birth weight (i.e., >4.1 kg)
- Preterm birth
- Respiratory distress syndrome
- Hypoglycemia or jaundice
- Obesity and type 2 diabetes later in life
- Polyhydramnios
- Stillbirth
Risk factors
- Age >40 years
- Being overweight or obese (BMI >30 kg/m2)
- Prediabetes
- Gestational diabetes during a previous pregnancy
- Polycystic ovary syndrome
- Family history of diabetes
- Previously delivered a baby weighing ≥4.1 kg
- Black, Hispanic, American Indian, and Asian American ethnicity
Treatment
- Control blood glucose levels
- Changes in diet and being more active to lower blood glucose
- Medicine (i.e., tablets or insulin injections) if the above does not lower blood glucose enough
- Blood glucose testing kit to monitor the effects of treatment
- Close monitoring during pregnancy and birth to check for any potential complications
- Best to give birth before 41 weeks → induction of labor or caesarean section may be recommended if labor does not start naturally by this time
- Early delivery may also be recommended if there are health concerns for the mother or baby, or if the blood glucose levels are not well controlled
Management
- Goal: Avoid maternal hypoglycemia or hyperglycemia (which can increase the risk of neonatal hypoglycemia), safe management of glycemic control, effective analgesia for labor
- Availability of appropriate equipment to monitor and treat hypoglycemia or hyperglycemia (e.g., glucometer, infusion pumps, 20% glucose) in the delivery units and obstetric theaters
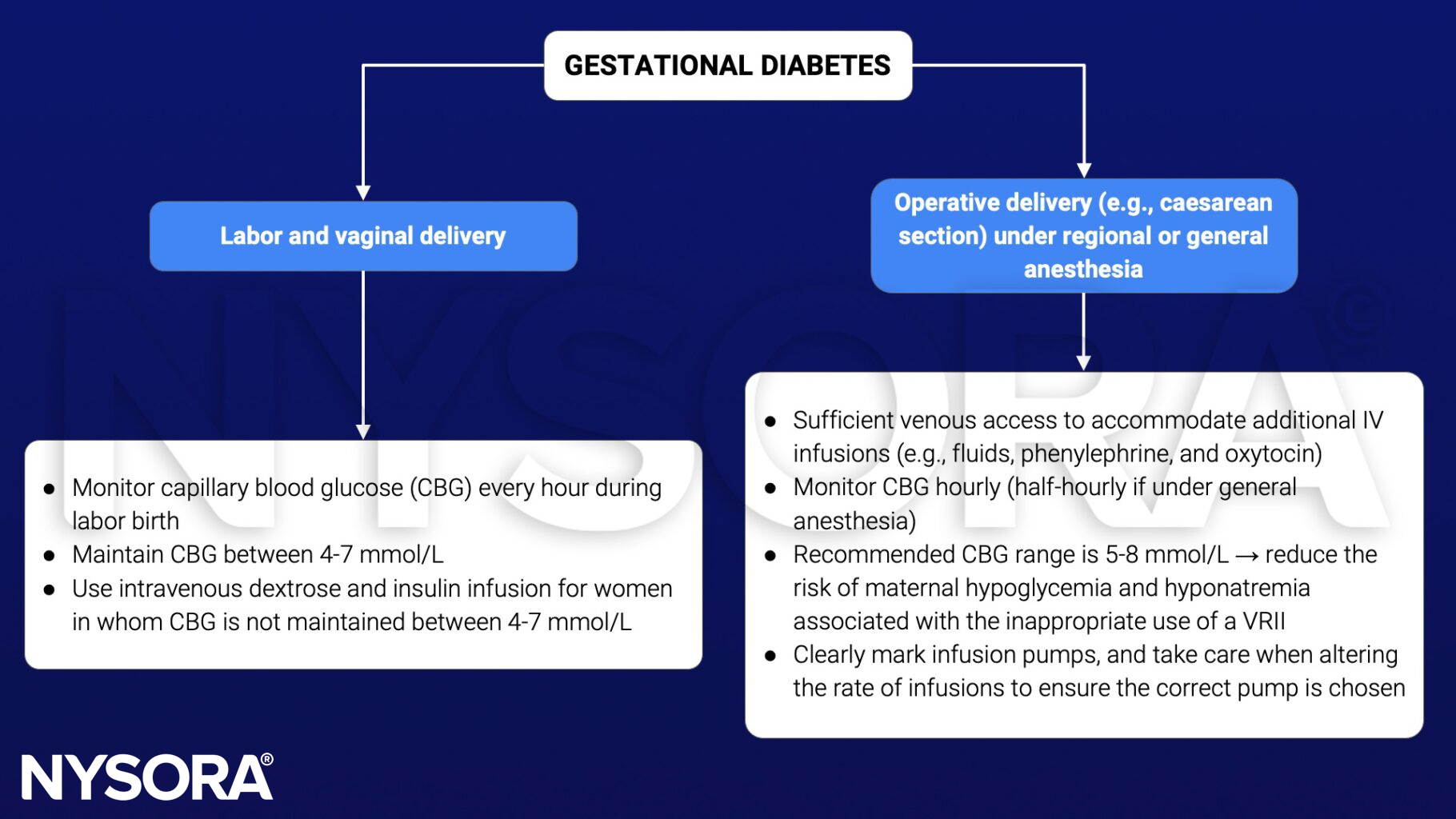
Variable rate intravenous insulin infusion (VRII) to maintain glycemic control
- Used when the target CBG range is not achieved by modification of the patient’s usual medications
- Glucose-containing substrate fluid alongside the IV insulin infusion to prevent gluconeogenesis, lipolysis, and ketoacidosis
- 5% glucose in 0.9% saline with premixed 0.15% (20 mmol/L) KCl or 0.30% (40 mmol/L) KCl to reduce the risk of developing hyponatremia
- Continue basal insulin after starting a VRII
See also pre-eclampsia considerations
See also caesarean section considerations
Prevention
- Eat healthy foods (high in fiber, low in fat and calories)
- Keep active
- Start pregnancy at a healthy weight
- Do not gain more weight than recommended during pregnancy
Suggested reading
- Yap Y, Modi A, Lucas N. The peripartum management of diabetes. BJA Educ. 2020;20(1):5-9.
Clinical updates
Rogers et al. (Anesthesiology, 2025) highlight that gestational diabetes mellitus (GDM) now affects a substantial proportion of pregnancies and requires tighter intrapartum glucose control (target 70–110 mg/dl) to reduce neonatal hypoglycemia, macrosomia, and stillbirth risk. The review emphasizes that anesthesiologists must increasingly manage IV insulin–dextrose protocols, recognize the growing use and limitations of continuous glucose monitoring during labor and cesarean delivery, and maintain a high index of suspicion for euglycemic diabetic ketoacidosis, which can occur even in GDM.
- Read more about this topic HERE.









