FACTS
- Indications: Distal foot and toe surgery
- Transducer position: about the ankle; depends on the nerve to be blocked
- Goal: local anesthetic spread surrounding each individual nerve
- Local anesthetic: 3–5 mL per nerve
GENERAL CONSIDERATIONS
Using an ultrasound (US)-guided technique affords a practitioner the ability to reduce the volume of local anesthetic required for ankle block. Because the nerves involved are located relatively close to the surface, ankle nerve blocks are easy to perform; however, knowledge of the anatomy of the ankle is essential to ensure success.
ULTRASOUND ANATOMY
Ankle nerve block involves anesthetizing five separate nerves: two deep and three superficial nerves. The two deep nerves are the tibial nerve and the deep peroneal nerve, and the three superficial nerves are the superficial peroneal, sural, and saphenous nerves. All nerves, except the saphenous, are terminal branches of the sciatic nerve; the saphenous nerve is a sensory branch of the femoral nerve.
Tibial Nerve
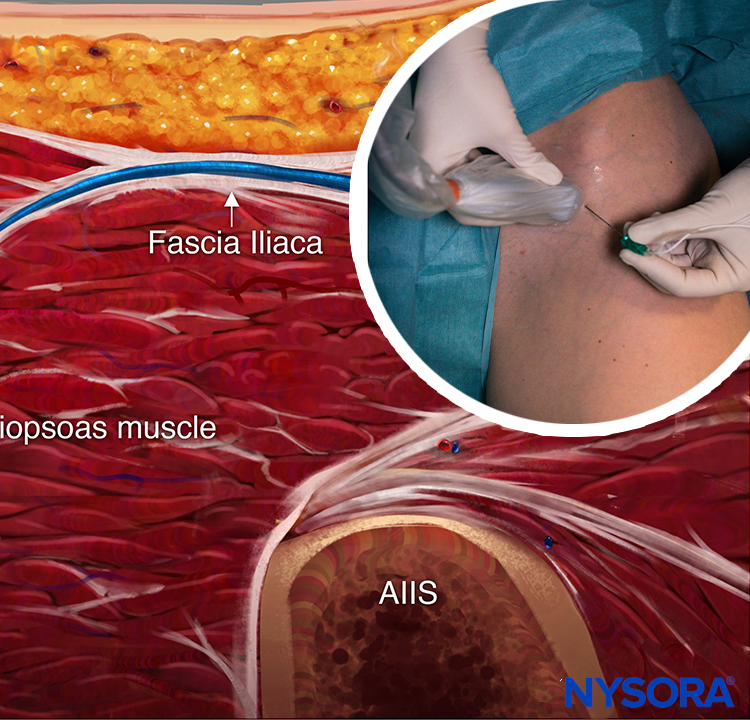
The tibial nerve is the largest of the five nerves at the ankle level and provides innervation to the heel and sole of the foot. With the linear transducer placed transversely at (or just proximal to) the level of the medial malleolus, the nerve can be seen immediately posterior to the posterior tibial artery (Figures 1, 2, and 3). Color Doppler can be very useful in locating the posterior tibial artery when it is not readily apparent. The nerve typically appears hyperechoic with honeycomb pattern. A useful mnemonic for the relevant structures in the vicinity is Tom, Dick ANd Harry, which refers to, from anterior to posterior, the tibialis posterior tendon, flexor digitorum longus tendon, artery/nerve/vein, and flexor hallucis longus tendon. These tendons can resemble the nerve in appearance, which can be confusing. The nerve’s intimate relationship with the artery should be kept in mind to avoid misidentification. If in doubt, track the structure proximally: tendons will turn into muscle bellies, whereas the nerve will not change in appearance.
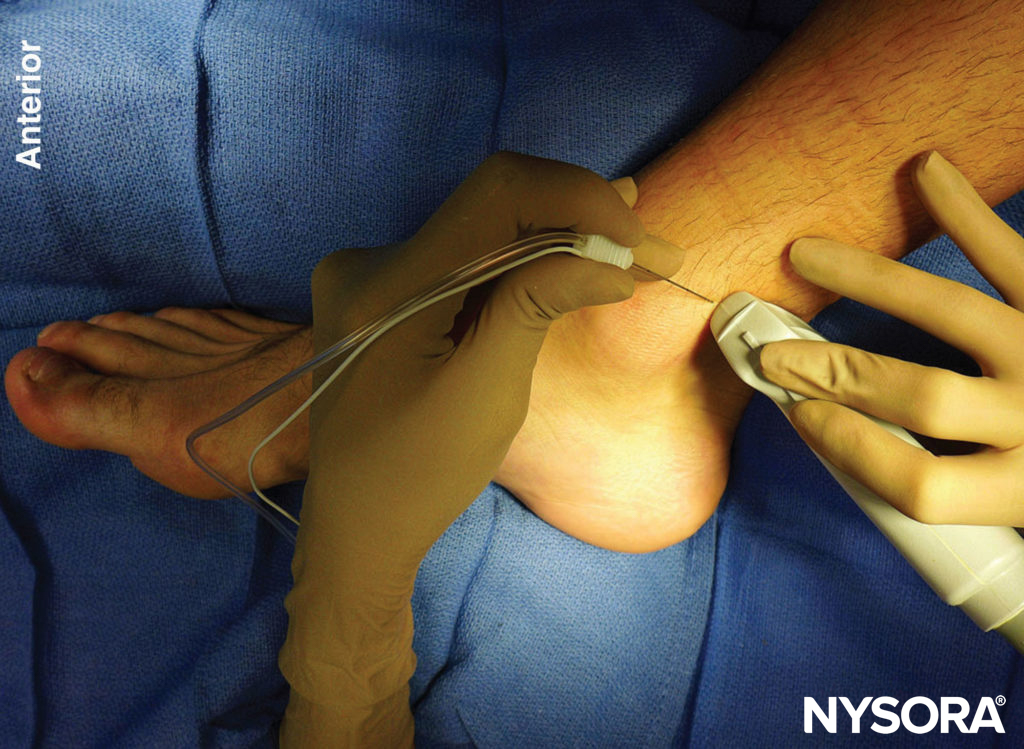
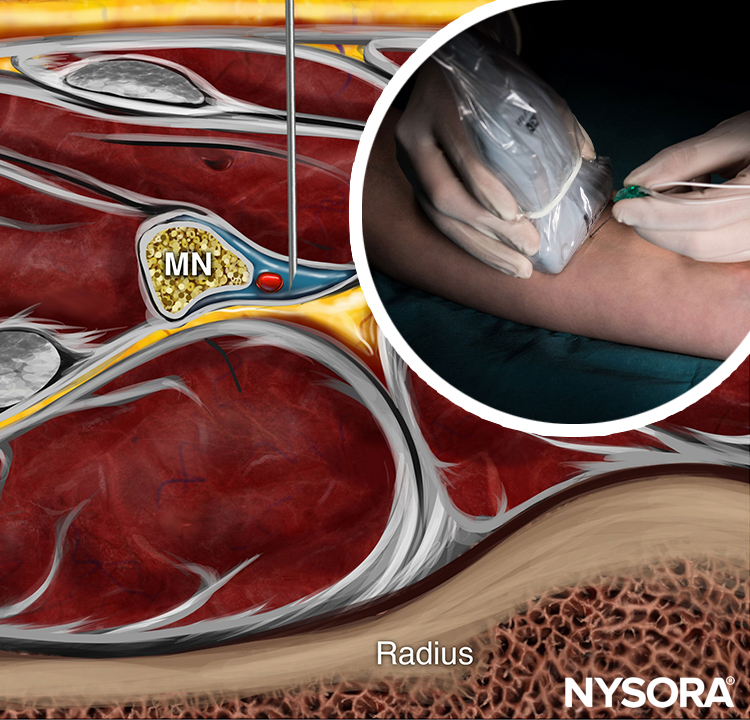
FIGURE 1. Transducer position and needle insertion for a nerve block of the tibial nerve using an in-plane technique.

FIGURE 2. Cross-sectional anatomy of the tibial nerve at the level of the ankle. Shown are the posterior tibial artery (PTA) and vein (PTV) behind the medial malleolus , the tibialis posterior (TP) and the flexor digitorum longus (FDL). The tibial nerve (TN) is just posterior to the posterior tibial vessels and superficial to the flexor hallucis longus muscle (FHL). (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
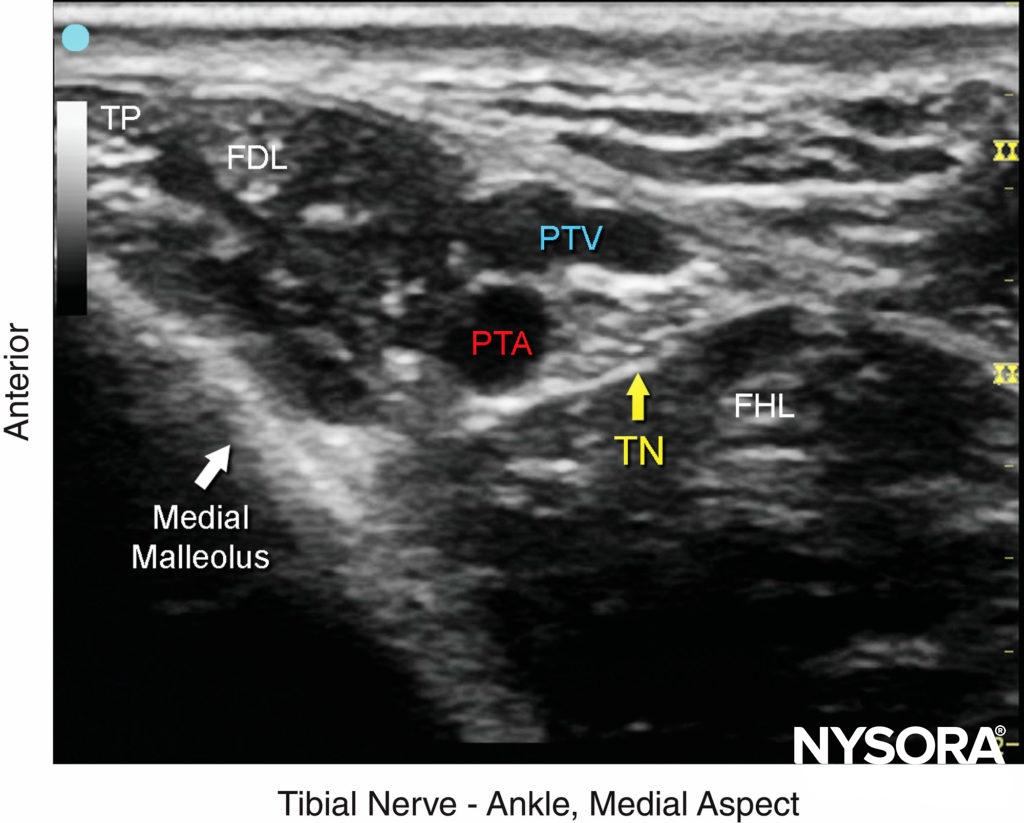
FIGURE 3. The tibial nerve (TN) is seen posterior and deep to the posterior tibial artery (PTA). TP, tibialis posterior; FDL, flexor digitorum longus; FHL, flexor hallucis longus; PTV, posterior tibial vein.
Deep Peroneal Nerve
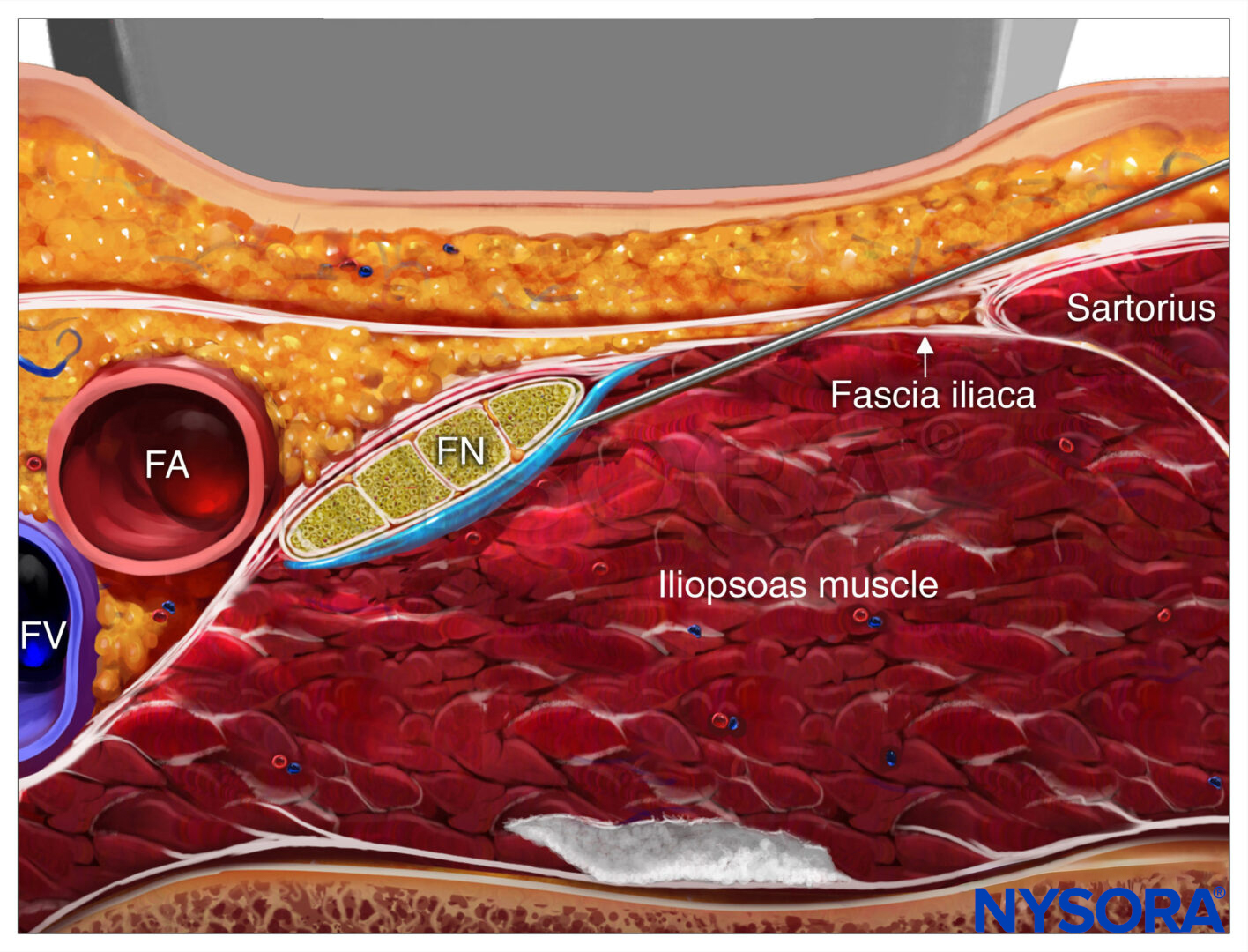
This branch of the common peroneal nerve innervates the ankle extensor muscles, the ankle joint and the web space between the first and second toes. As it approaches the ankle, the nerve crosses the anterior tibial artery from a medial to lateral position. A transducer placed in the transverse orientation at the level of the extensor retinaculum will show the nerve lying immediately lateral to the artery, on the surface of the tibia (Figures 4, 5, and 6). In some individuals the nerve courses along the medial side of the artery. The nerve usually appears hypoechoic with a hyperechoic rim, but it is small and often difficult to distinguish from the surrounding tissue.

FIGURE 4. Transducer position and needle insertion to nerve block the deep peroneal nerve at the level of the ankle.
(Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
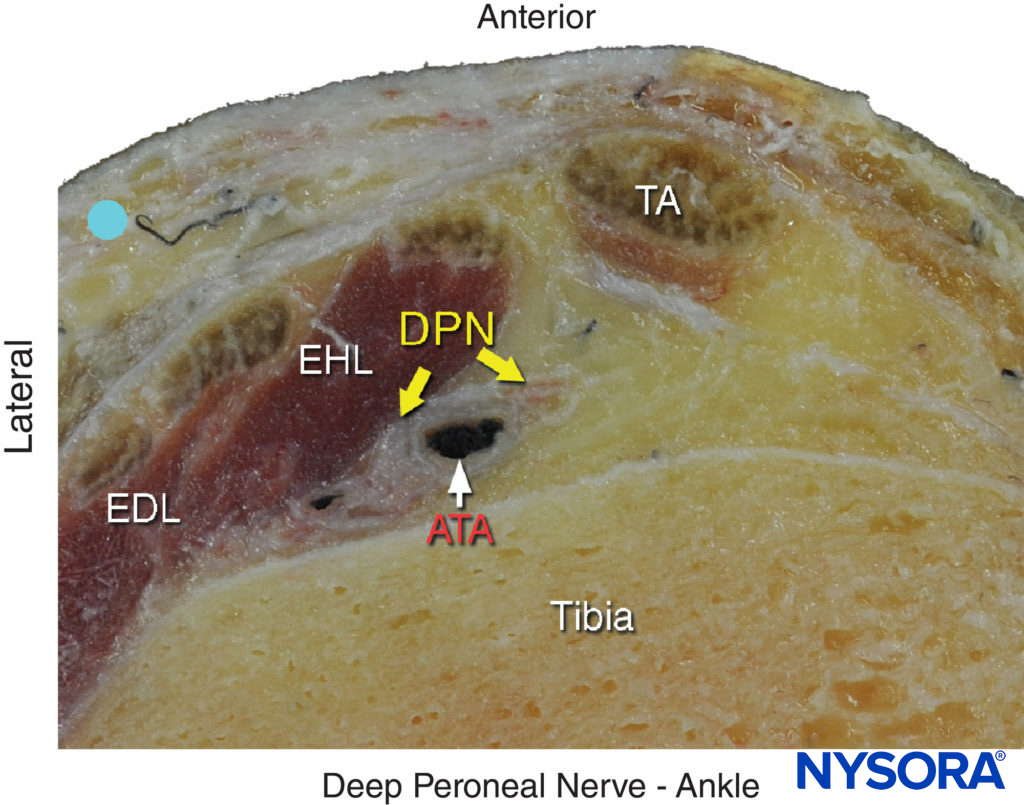
FIGURE 5. Cross-sectional anatomy of the deep peroneal nerve at the level of the ankle. The deep peroneal nerve (DPN) is located just lateral to anterior tibial artery (ATA) and between extensor hallucis longus (EHL) and tibia. Note the proximity of the extensor digitorum longus (EDL) and the tibialis anterior (TA), which can serve as an important landmark; to locate it, flex and extend the patient’s great toe manually. The deep peroneal nerve appears divided in this section. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York:McGraw-Hill, 2011.)
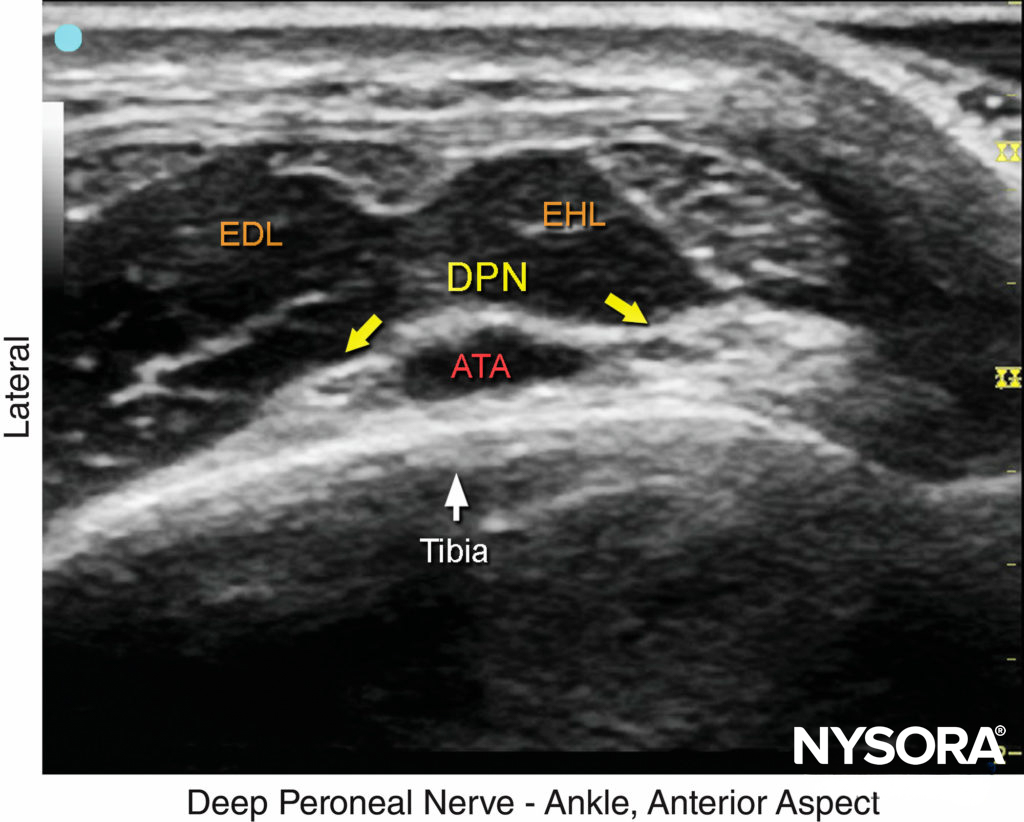
FIGURE 6. US image of the deep peroneal nerve (DPN), seen at the surface of the tibia just lateral to the anterior tibial artery (ATA). The nerve is divided in this image. The surrounding tendons are the extensor hallucis longus (EHL) and the extensor digitorum longus (EDL). (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
Superficial Peroneal Nerve
The superficial peroneal nerve innervates the dorsum of the foot. It emerges to lie superficial to the fascia 10–20 cm above the ankle joint on the anterolateral surface of the leg and divides into two or three small branches. A transducer placed transversely on the leg, approximately 5-10 cm proximal and anterior to the lateral malleolus, will identify the hyperechoic nerve branches lying in the subcutaneous tissue immediately superficial to the fascia (Figures 7, 8, and 9). To identify the nerve proximal to its division, the transducer can be traced proximally until, at the lateral aspect, the extensor digitorum longus and peroneus brevis muscle can be seen with a prominent groove between them leading to the fibula (Figure 10).

FIGURE 7. Transducer position and needle insertion to nerve block the superficial peroneal nerve.
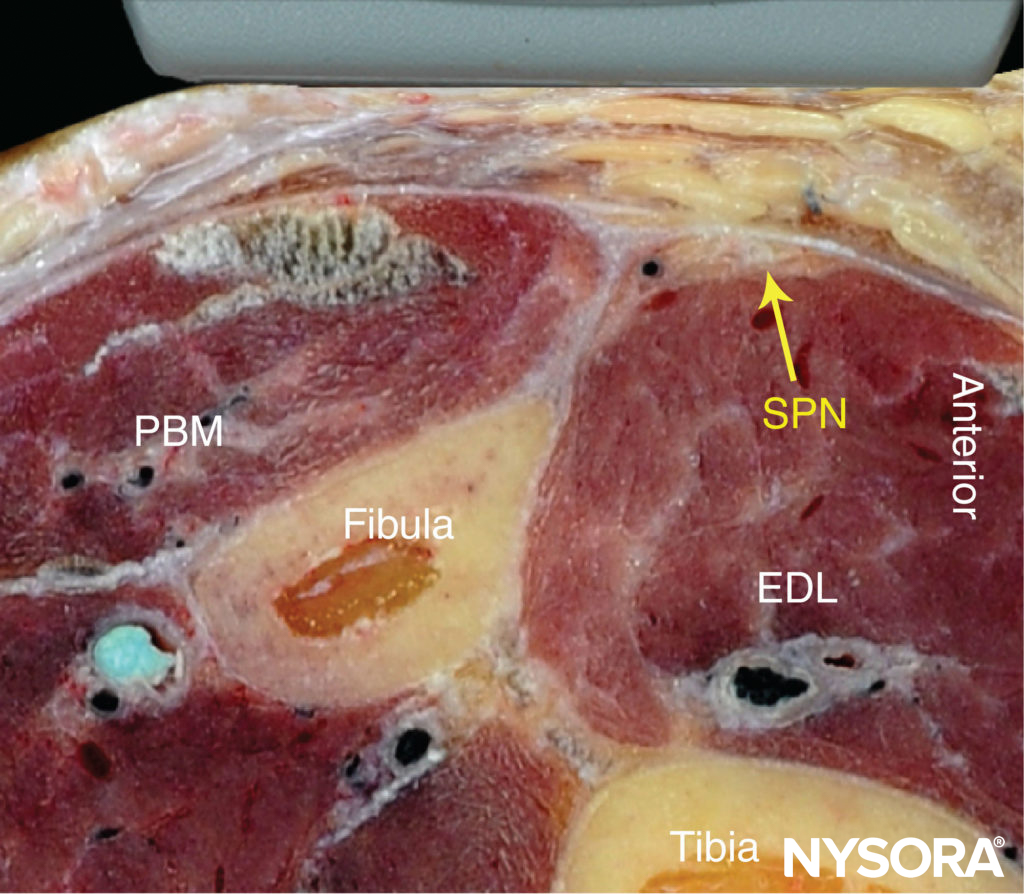
FIGURE 8. Cross-sectional anatomy of the superficial peroneal nerve (SPN). EDL, extensor digitorum longus muscle; PBM, peroneus brevis muscle. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound- Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)

FIGURE 9. US anatomy of the superficial peroneal nerve (SPN). PBM, peroneus brevis muscle. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
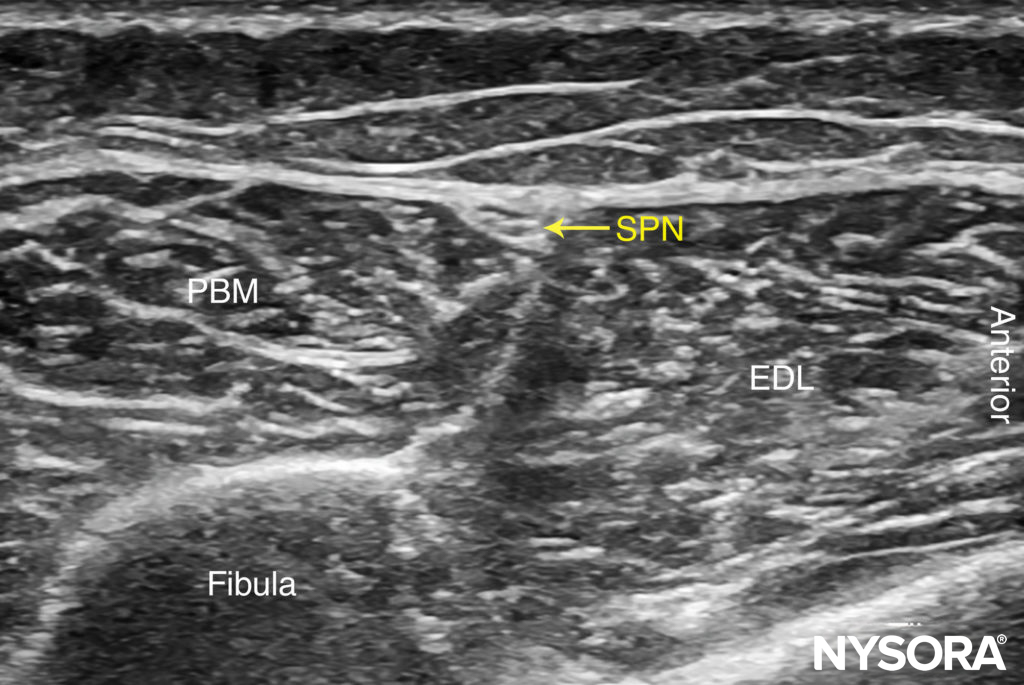
FIGURE 10. US anatomy of the superficial peroneal nerve with structures labeled. EDL, extensor digitorum longus muscle; PBM, peroneus brevis muscle; SPN, superficial peroneal nerve.
The superficial peroneal nerve is located in this groove, just deep to the fascia. Once it has been identified at this more proximal location, the nerve can be traced distally to the ankle or it can be blocked at this level. Because the superficial nerves are rather small, their identification with US is not always possible.
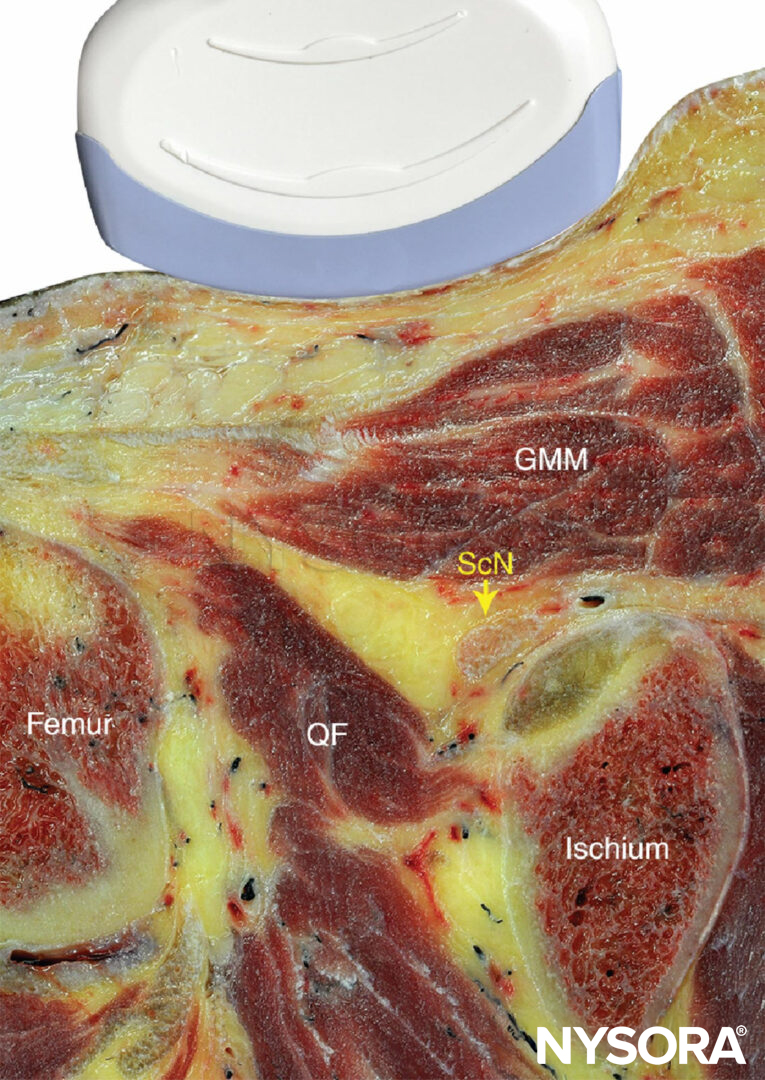
Sural Nerve
The sural nerve innervates the lateral margin of the foot and ankle. Proximal to the lateral malleolus, the sural nerve can be visualized as a small hyperechoic structure that is intimately associated with the small saphenous vein superficial to the deep fascia.
The sural nerve, can be traced back along the posterior aspect of the leg, running in the midline superficial to the Achilles tendon and gastrocnemius muscles (Figures 11, 12, and 13). A calf tourniquet can be used to increase the size of the vein and facilitate its imaging; the nerve is often found in the immediate vicinity of the vein.

FIGURE 11. Transducer position and needle insertion to nerve block the sural nerve. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
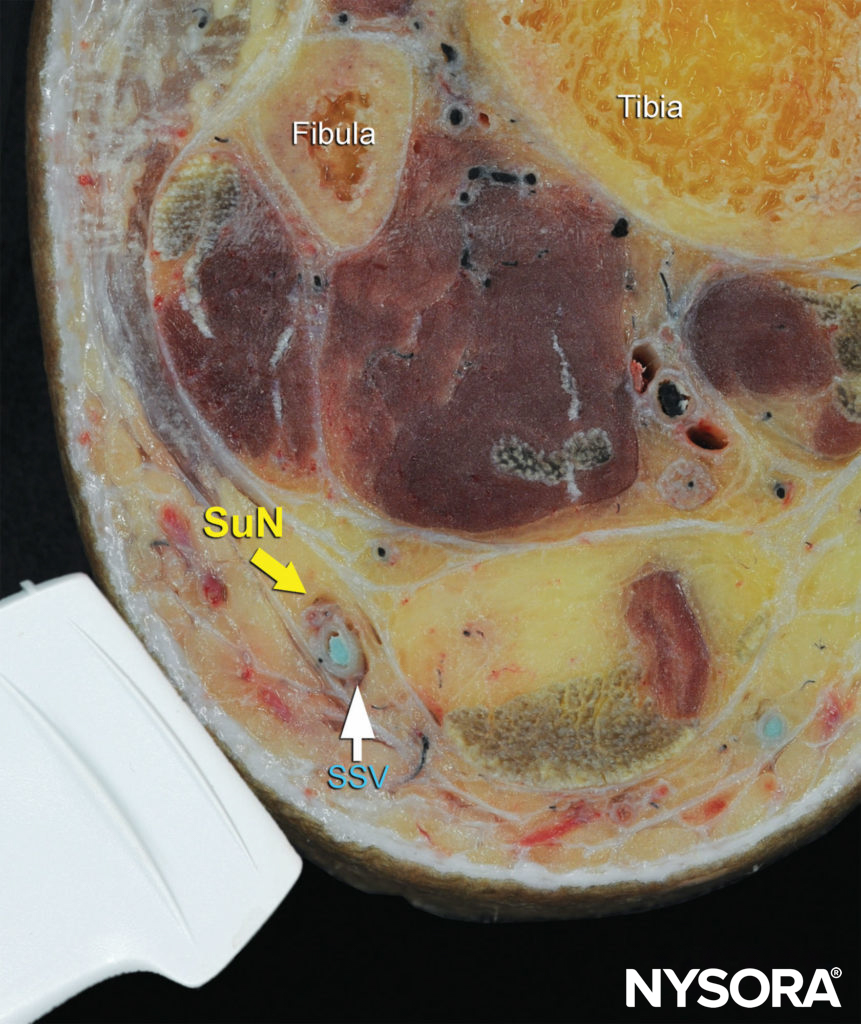
FIGURE 12. Cross-sectional anatomy of the sural nerve at the level of the ankle. Shown is the sural nerve (SuN) in the immediate vicinity of the small saphenous vein (SSV). (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
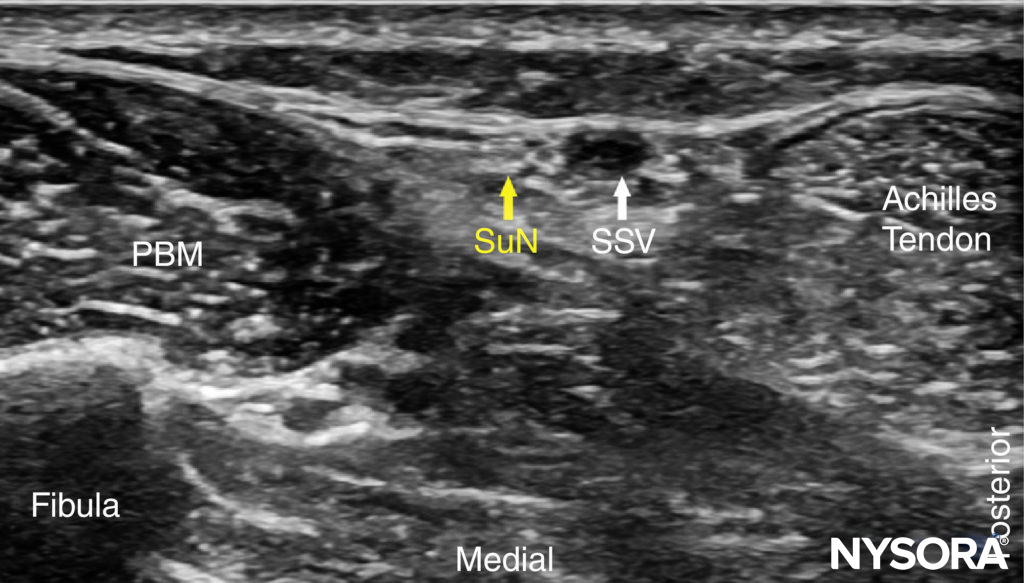
FIGURE 13. US anatomy of the sural nerve (SuN). Shown are the peroneus brevis muscle (PBM) and small saphenous vein (SSV).
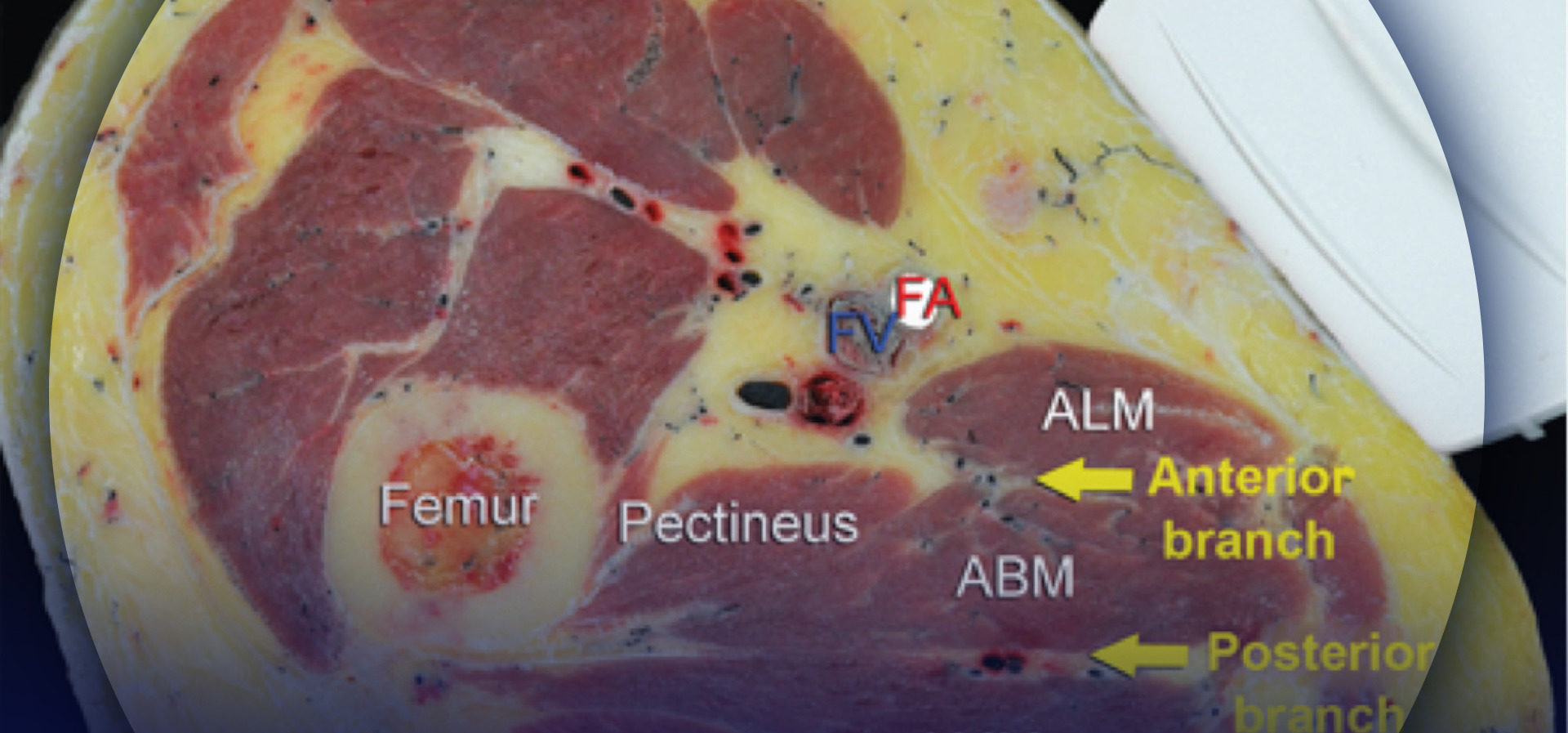
Saphenous Nerve
The saphenous nerve innervates the medial malleolus and a variable portion of the medial aspect of the leg below the knee. The nerve travels down the medial leg alongside the great saphenous vein. Because it is a small nerve, it is best visualized 10–15 cm proximal to the medial malleolus, using the great saphenous vein as a landmark (Figures 14, 15, and 16). A proximal calf tourniquet can be used to assist in increasing the size of the vein.

FIGURE 14. Transducer position and needle insertion to nerve block the saphenous nerve. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
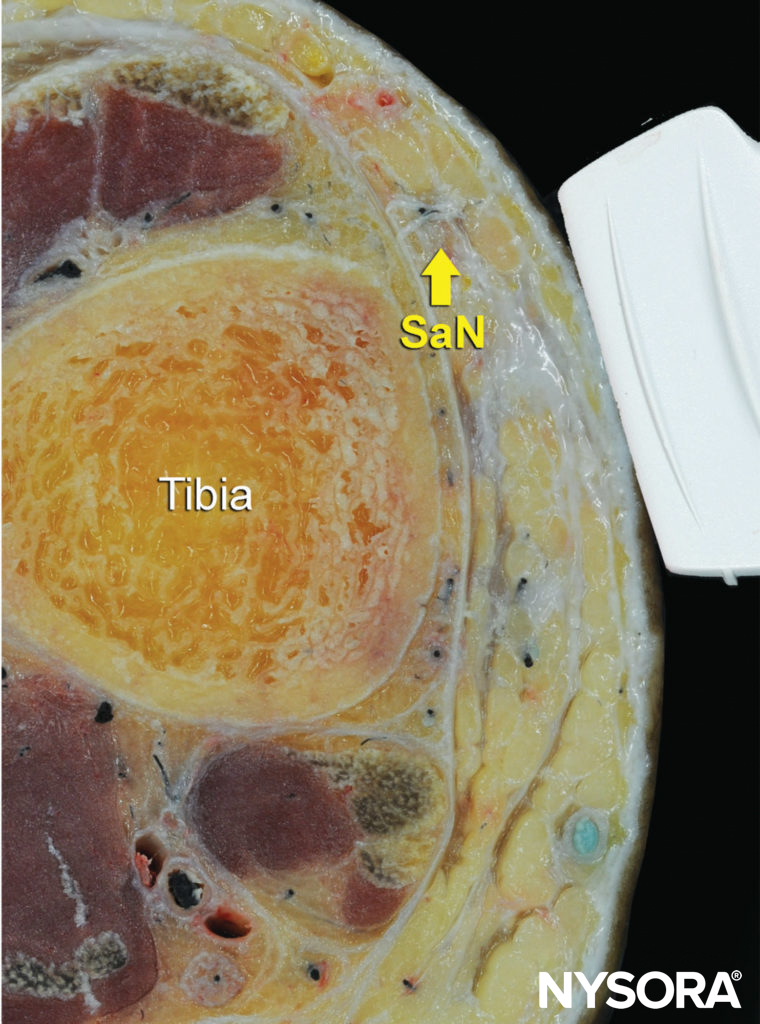
FIGURE 15. Cross-sectional anatomy of the saphenous nerve (SaN) at the level of the ankle. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)

FIGURE 16. US anatomy of the saphenous nerve (SaN). Shown are the great saphenous vein (SaV) and the medial malleolus (Med. Mall.). (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
For a more comprehensive review of the distribution of each nerve, see Functional Regional Anesthesia Anatomy.
DISTRIBUTION OF ANESTHESIA
An ankle nerve block results in anesthesia of the entire foot.
EQUIPMENT
The equipment recommended for an ankle nerve block is:
- Ultrasound machine with linear transducer (8–18 MHz), sterile sleeve, and gel
- Standard nerve block tray
- Three 10-mL syringes containing local anesthetic
- A 1.5-inch, 22- to 25-gauge needle with low-volume extension tubing
- Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
This nerve block is usually performed with the patient in the supine position with a footrest underneath the calf to facilitate access to the ankle, especially for the tibial and sural nerve blocks. An assistant is helpful to maintain internal or external rotation of the leg as needed.
GOAL
The goal is to place the needle tip immediately adjacent to each of the five nerves and deposit local anesthetic until the spread around each nerve is accomplished.
TECHNIQUE
With the patient in the proper position, the skin is disinfected. For each of the nerve blocks, the needle can be inserted either in-plane or out-of-plane. Ergonomics often dictate which approach is most effective.
A successful nerve block is predicted by the spread of local anesthetic immediately adjacent to the nerve. Redirection to achieve circumferential spread is not necessary because these nerves are small, and the local anesthetic diffuses quickly into the neural tissue. A 3–5 mL of local anesthetic per nerve is typically sufficient for an effective nerve block.
TIPS
-
- If the smaller superficial nerves (sural, saphenous and superficial peroneal) are not seen, these nerves can be blocked simply by injecting local anesthetic into the subcutaneous tissue as a “skin wheal”; for the sural nerve, inject from the Achilles tendon to the lateral malleolus; for the superficial peroneal and the saphenous, inject anteriorly from one malleolus to the other, taking care to avoid injuring the great saphenous vein.
- The saphenous nerve block can be omitted in surgery on the forefoot and toes. In 97% of patients, the saphenous nerve innervation does not extend beyond the midfoot. However, an anatomical study found branches of the saphenous nerve reaching the first metatarsal in 28% of specimens.
Clinical updates
Pascarella et al. (Journal of Clinical Medicine, 2025) provide an updated, comprehensive review showing that motor-sparing, ultrasound-guided regional techniques—particularly ankle and high-ankle blocks—are preferred for ambulatory foot and ankle surgery, as they balance effective analgesia with early mobilization and lower fall risk than popliteal sciatic blocks. The authors highlight intravenous dexamethasone as a key adjuvant to prolong block duration and reduce opioid requirements, and note growing but still limited evidence for WALANT and Mayo blocks in selected forefoot procedures. Overall, the review emphasizes tailoring block selection, adjuvants, and multimodal analgesia to procedure type and discharge goals, rather than adopting a one-size-fits-all regional strategy.
- Read more about the study HERE.
Schou et al. (Foot and Ankle Surgery, 2024) performed a systematic review with meta-analysis and trial sequential analysis showing that ankle blocks prolong analgesia by ~7 hours compared with no intervention or sham, but with very low-certainty evidence and no reliable reduction in 24-hour opioid consumption. When compared with sciatic nerve blocks, ankle blocks provided ~6–7 hours shorter analgesia and may be associated with slightly higher opioid use, though certainty remained low due to high risk of bias and sparse data. Overall, the findings support ankle blocks as a mobility-preserving option for outpatient forefoot surgery, but highlight the need for higher-quality trials to define their role within multimodal analgesia pathways.
- Read more about the study HERE.
Moosa et al. (BJA Education, 2022) provide an updated, practical synthesis of ultrasound-guided regional anaesthesia for foot and ankle surgery, emphasizing that more proximal ultrasound-guided ankle blocks (rather than traditional landmark techniques at the malleoli) reliably extend sensory coverage to the heel and improve tolerance of ankle tourniquets. The review highlights procedure-specific block selection (ankle vs popliteal sciatic ± saphenous) to balance analgesia with postoperative motor function, noting that ankle blocks preserve mobility compared with popliteal approaches. It also underscores the growing roles of perineural catheters and IV dexamethasone to prolong analgesia during high-pain procedures, while emphasising vigilance for compartment syndrome and safe postoperative mobilisation strategies.
- Read more about the study HERE.