Interventional Pain: A Step-by-Step Guide for the FIPP Exam
Editors: Stogicza, A.R., Mansano, A., Trescot, A.M., Staats, P.S.
Publisher: Springer
Cervical Medial Branch Block and Radiofrequency Ablation - Oblique Approach
Harold J. Cordner and André M. Mansano
1. PROS OF OBLIQUE APPROACH
- Shorter needle track and less patient discomfort than posterior approach
- Patient in supine position, affords better comfort, communication, and airway access
- Easy visualization of lower levels
2. CONS OF OBLIQUE APPROACH
- Vital structures (spinal cord and vertebral artery) in needle trajectory
- Parallel placement of an RF cannula to the medial branch nerve is not possible, technique is less suitable for RF ablation (unless special needles are used)
3. EQUIPMENT AND MONITORING
- Standard ASA monitoring
- Fluoroscopy
- Sterile prep, and drape
- Skin local anesthesia prior to any needle larger than 25G (unless sedation is used)
- Procedure is not performed with a coaxial view
- CPR equipment and medications available
- For diagnostic block
- 22–25G, 2 inch (50 mm) – 3.5 inch (90 mm) needle, tip curved to facilitate steering. 0.3- 0.5 ml local anesthetic/level
- Non-ionic contrast (optional)
- For RFA
- 18–22G, 2 inch (50 mm)
- 3.5 inch (90 mm) radiofrequency cannula: 5–10 mm active tip
- Grounding pad – RF generator with capacity for unipolar and bipolar lesions
- Local anesthetic
4. ANATOMY
- Prevalence studies, physical exam, and pain referral maps can be utilized to choose levels
- C2–3 and C5–6 levels are the most common causes of cervicogenic headache and neck pain, respectively
- At the C3 level, there is a superfcial medial branch (third occipital nerve) that is located in close proximity to the C2/3 facet joint and serves to innervate that joint as well as the suboccipital area
- The deep medial branch of C3 (which is analogous to the medial branches of C4, C5, and C6) courses along the waist of the corresponding articular pillars and supplies the adjacent vertebral segments (for instance, the C4 and C5 medial branches supply the zygapophyseal joint of C4/5)
- The C5 medial branch is located in the waist of the articular pillar of C5. The C3, C4, and C6 medial branches are located slightly above the waist of the corresponding articular pillars, and variations exist
- The C7 vertebra has a prominent transverse process (TP), and the location of the medial branch at this level is variable. It can be found as far caudal as the TP/superior articular process (SAP) junction and as far rostral as the apex of the C7 SA
5. STRUCTURES TO KEEP IN MIND AND POSSIBLE COMPLICATIONS
- Vertebral artery (if needle is more anterior than appropriate target) → seizure, dissection, stroke
- Inadvertent intraarticular facet injection
- Inadvertent passage of needle though a facet joint → intrathecal, epidural medication administration, high spinal anesthesia, spinal cord injury, paralysis, death
- Injection of spinal nerve root → nerve damage, epidural, intrathecal injection
- Injection of a vascular structure that may be in contiguity with a radicular artery → spinal cord infarct
- Infection
- Bleeding
- Postprocedure pain
- Vasovagal reaction
- Allergic reaction
6. FLUOROSCOPY TECHNIQUE, TARGET LOCALIZATION
- Supine patient position
- C-arm in lateral view. In a true lateral, the articular pillars overlap and are clear and crisp. The facet joints above and below the level of interest must be crisp. The disc spaces must be clear. The anterior and posterior tubercles on each side should form a superimposed curvilinear line located in the superior posterior quadrant of the vertebral body shadow (Fig. 1a and b)
- A cranio-caudal or dorsoventral adjustment may be needed to get an optimal view of the articular pillar
- At this point, oblique the C-arm until the neural foramens are clearly visualized (Fig. 1a–c)
- The target point is the base of the superior articular process (SAP) at or just below the most inferior aspect of the intervertebral foramen
- The skin entry point (Fig. 2a, b) is slightly posterior and caudal to the target

Fig. 1 Foraminal view of the cervical spine. Blue Asterisk marks the optimal skin entry. Dark green = superior articular process. Complete Anatomy image (a), native (b) and edited fuoroscopy images (c)
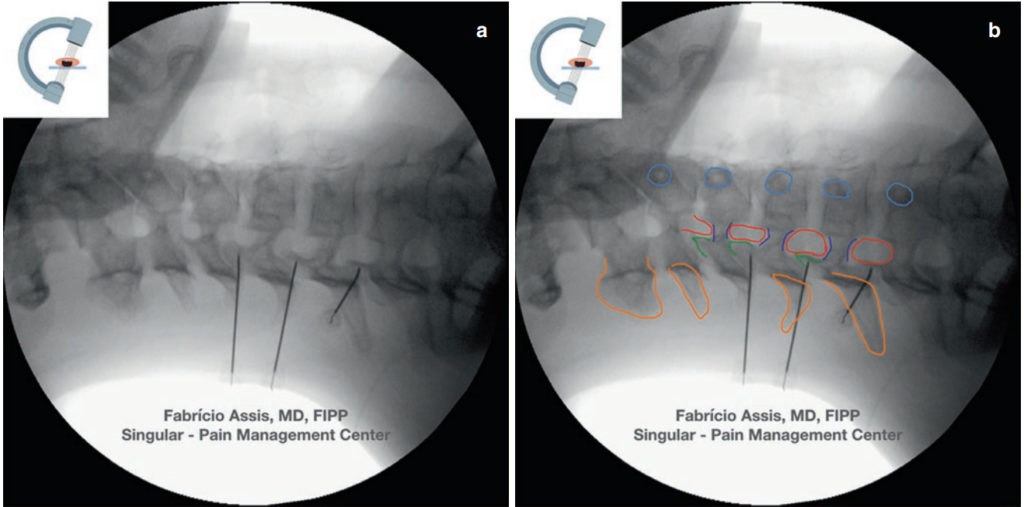
Fig. 2 Native and edited images of oblique view of the cervical spine. Needles in place, touching the articular pillar. Orange = spinous process and lamina; dark green = superior articular process; red = intervertebral foramen; dark blue = ipsilateral pedicle; light blue = contralateral pedicle. Native (a) and edited fuoroscopy images (b)
7. PROCEDURE STEPS
- Insert needle just posterior and caudal to the base of SAP (Fig. 1b, c)
- Advance the needle until bony contact at the base of SAP (Fig. 2a, b). Keep in mind that this procedure is not done in a coaxial view
- Posteroanterior (PA) view to check the optimal needle position at the waist of the articular pillar (Fig. 3a–c)
- Once needle position is confrmed in two views, sensory and motor testing is performed to confrm needle is within effective proximity to the medial branch nerve and not in proximity to the motor nerve root. Ideally, sensory testing will reveal paresthesia <0.5 V and motor testing at 1.5– 2.0 V should produce no motor response in upper extremity or face
- Inject 0.3–0.5 cc of contrast media to detect possible intravascular spread for diagnostic procedure
- Inject 0.3 cc of local anesthetic for block
- Radiofrequency lesioning can then be performed at 75–80°C for 60–120 seconds
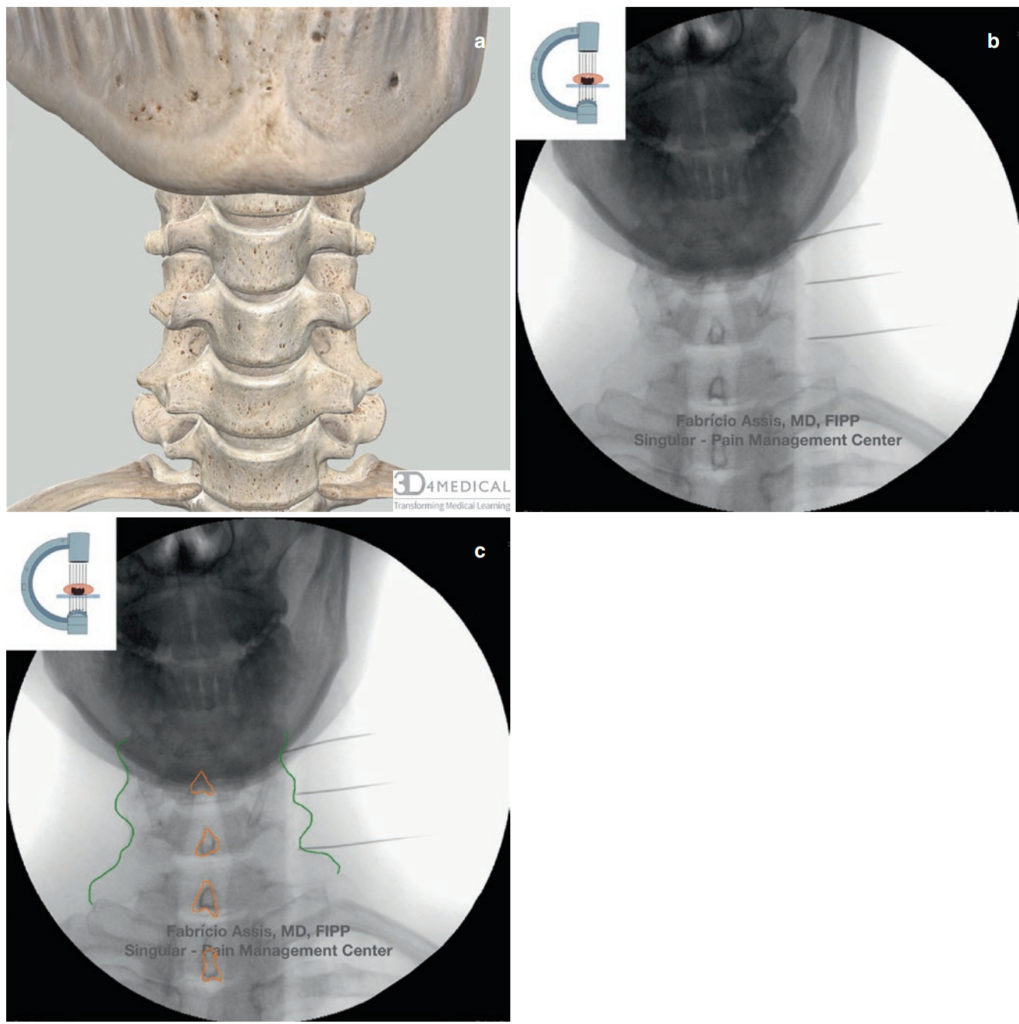
Fig. 3 PA view of the cervical spine, needles in place for C5, 6, 7 MBB. Orange = spinous process; dark green = articular pillar line. Complete Anatomy image (a), native (b) and edited fuoroscopy images (c)
8. CLINICAL PEARLS
- An optimal view of the cervical foramen is paramount in performing this procedure
- Good sensory and motor stimulation is necessary to ensure more consistent success
- Due to the poor predictive value of single diagnostic blocks, dual medial branch blocks may be performed to make the diagnosis of facet joint pain prior to proceeding to the defnitive radiofrequency treatment
- Small amount of corticosteroid may help prevent neuritis or postlesioning pain
9. UNACCEPTABLE, POTENTIALLY HARMFUL NEEDLE PLACEMENT ON EXAM
- Not checking PA view
- Needle through facet joint or compromised intraspinal space
- Needle tip too anterior
- Needle in foramen
- Any proof of lack of understanding of cervical spine anatomy
10. UNACCEPTABLE, BUT NOT HARMFUL NEEDLE PLACEMENT ON EXAM
- Unnecessarily large bore needle
- Not obtaining a good oblique view
- The procedure was abandoned after unsuccessful attempts, but it was clear that the examinee was cognizant of the safety aspects of the procedure, the needle did not compromise vital structures, did not reach the epidural space, spinal cord or vertebral artery
Enriched with NextLevel CME™ technology:
– Make notes in seconds and never lose them
– Insert your own images, infographics
– Add and watch videos inside your notes
– Attach PDFs, articles, website links
– Listen to the audio