Interventional Pain: A Step-by-Step Guide for the FIPP Exam
Editors: Stogicza, A.R., Mansano, A., Trescot, A.M., Staats, P.S.
Publisher: Springer
Splanchnic Block and Radiofrequency Ablation
André M. Mansano
1. EQUIPMENT AND MONITORING
- Standard ASA monitors
- Fluoroscopy
- Sterile prep, and drape
- Skin local anesthesia prior to any needle larger than 25G (unless sedation is used)
- Coaxial view is always used to advance needle, unless otherwise specified • CPR equipment and medications available
- 22G, 3.5 inch (90 mm) – 7 inch (180 mm) needle, tip curved for diagnostic injection
- 18–20G, 3.5 inch (90 mm) – 7 inch (180 mm) curved tip radiofrequency cannula with 10 mm active tip for radiofrequency ablation (RF)
- Grounding pad
- RF generator with capacity for unipolar and bipolar lesions
- Infusion of 500 ml fluid preprocedure
- Local anesthetic
- Nonionic contrast
2. ANATOMY
- The splanchnic nerves are comprised of medial branches from the lower seven thoracic sympathetic ganglia
- The greater splanchnic nerve is derived from the fifth to ninth thoracic ganglia, with the potential for contribution from the tenth thoracic ganglion
- The greater splanchnic nerves descend in the paravertebral space, obliquely, giving off branches to the descending aorta and perforating the crus of the diaphragm
- The greater splanchnic nerve synapses in the superior aspect of celiac ganglia
- Innervates: Gastrointestinal tract (from distal esophagus to mid-transverse colon) pancreas, stomach, liver, adrenals, ureters, abdominal vessels
- T11 vertebral body
- The target is the anterior third of the T11 vertebral body in lateral view
3. STRUCTURES TO KEEP IN MIND AND POSSIBLE COMPLICATIONS
- Thoracic nerve roots → nerve injury
- Intercostal blood vessels and nerves → nerve injury, bleeding
- Intervertebral disc → discitis
- Lung/pleura → pneumothorax
- Thoracic duct → chylothorax
- Diaphragm → hemidiaphragmatic paralysis
- Aorta/inferior vena cava → bleeding, local anesthetic toxicity
- Segmental/intercostal artery, possibly feeding the anterior spinal artery (artery of Adamkiewicz) → spinal cord injury/ischemia
- Infection
- Bleeding
- Postprocedure pain
- Vasovagal reaction
- Allergic reaction
- Hypotension caused by splanchnic vasodilation
4. FLUOROSCOPY TECHNIQUE, TARGET LOCALIZATION
- Patient in prone position
- Anteroposterior (AP) image (Fig. 1a–c)
- Identify T11 level (Some also perform procedure at T10, as well as T12 level)
- Square off the inferior endplate of T11 (Fig. 2a–c)
- Identify diaphragm movement during inspiration and expiration, particularly if performing the procedure at T12 level (as well). If the diaphragm shadows the lateral edge of the T12 vertebral body, then only do the T11 or T10 and T11 level
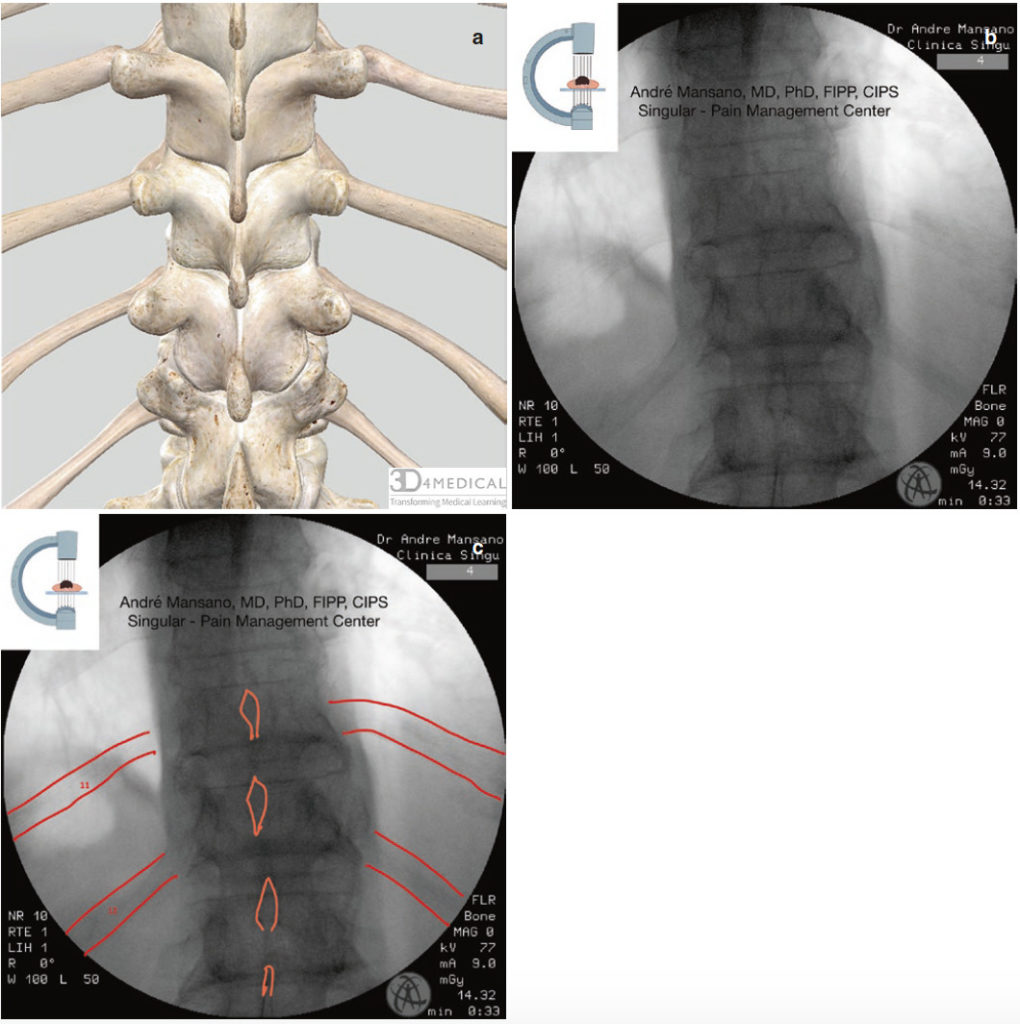
Fig. 1 AP view of the thoracic spine. Red = ribs; orange = spinous process. Complete Anatomy image (a), native (b) and edited fluoroscopy image (c)
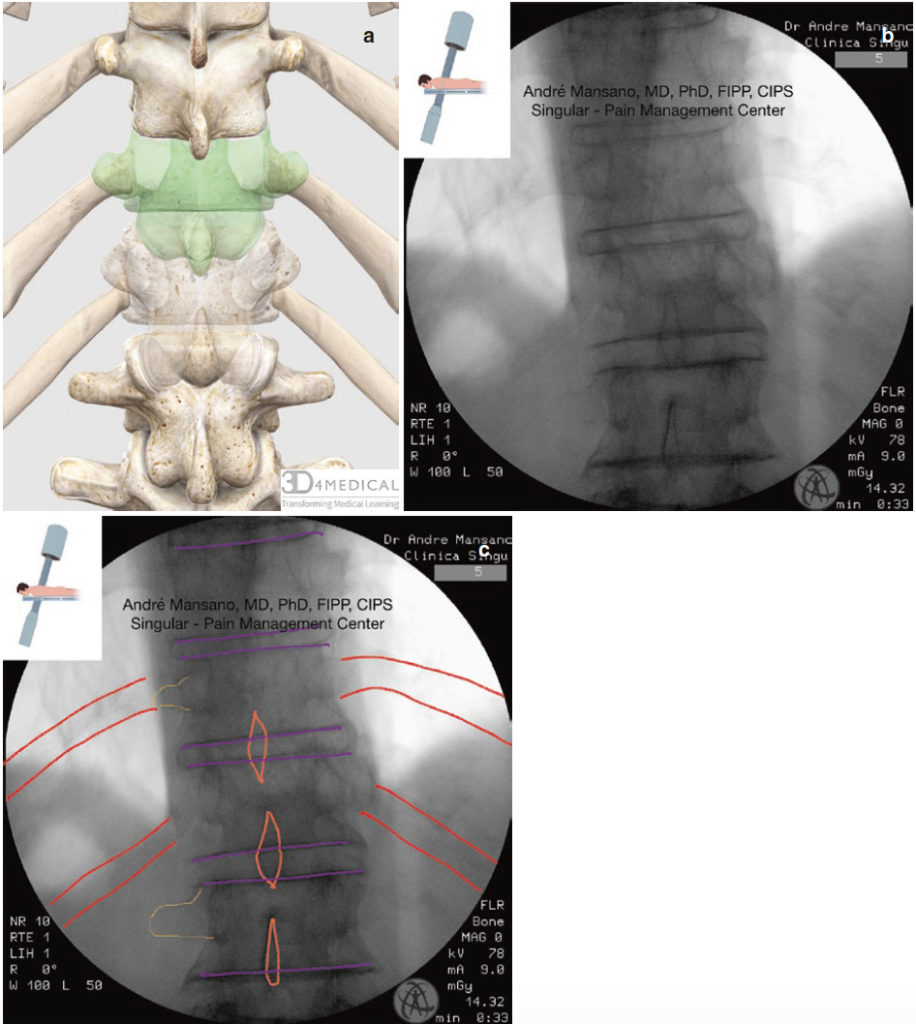
Fig. 2 AP view of the thoracic spine with caudad tilt of the C-arm, squared endplates of T11 vertebra. Red = ribs; orange = spinous process; yellow = transverse process; purple = vertebral body endplates. Complete Anatomy image, T11 vertebra faded and highlighted, and T12 vertebra faded (a), native (b) and edited fluoroscopy image (c)
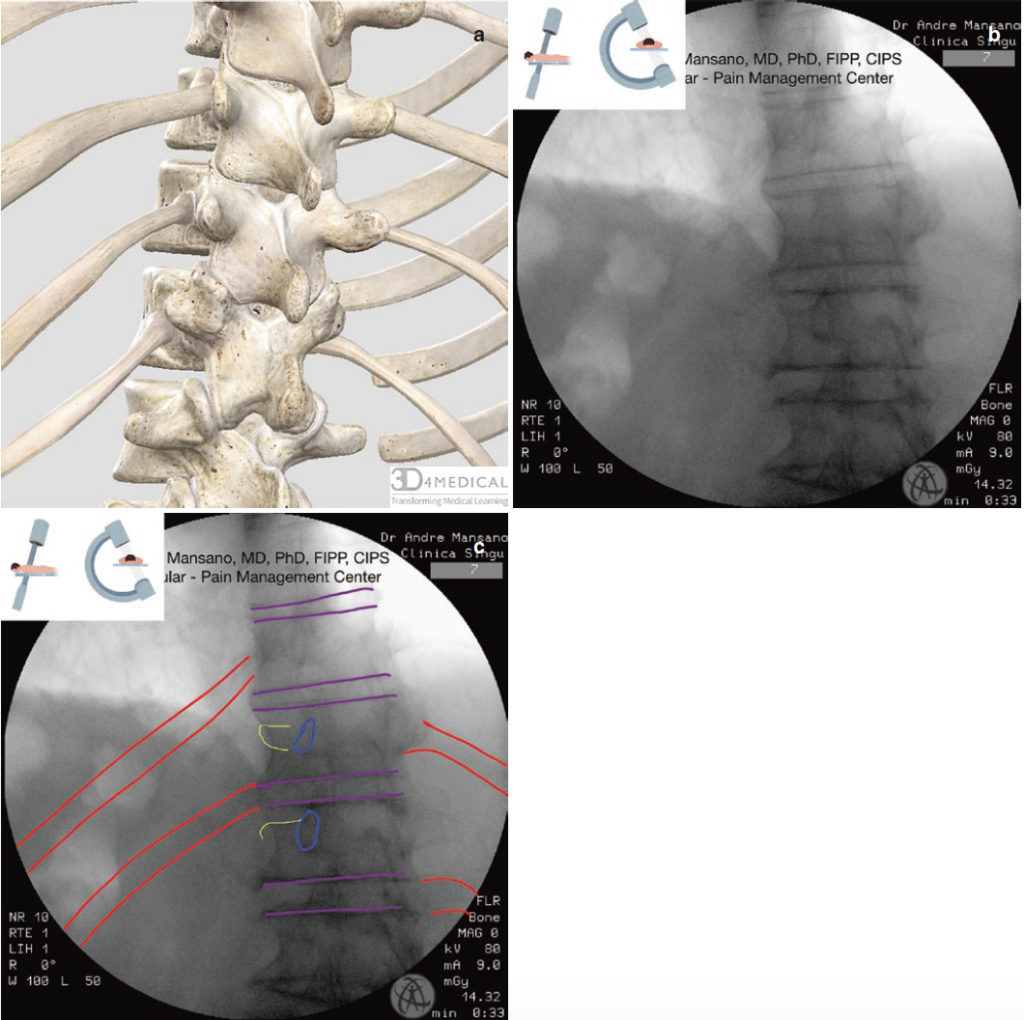
Fig. 3 Oblique view of the thoracic spine. Red = ribs; Blue = pedicle; yellow = transverse process; purple = vertebral body endplates. Complete Anatomy image (a), native (b) and edited fluoroscopy image (c)
7. PROCEDURE STEPS
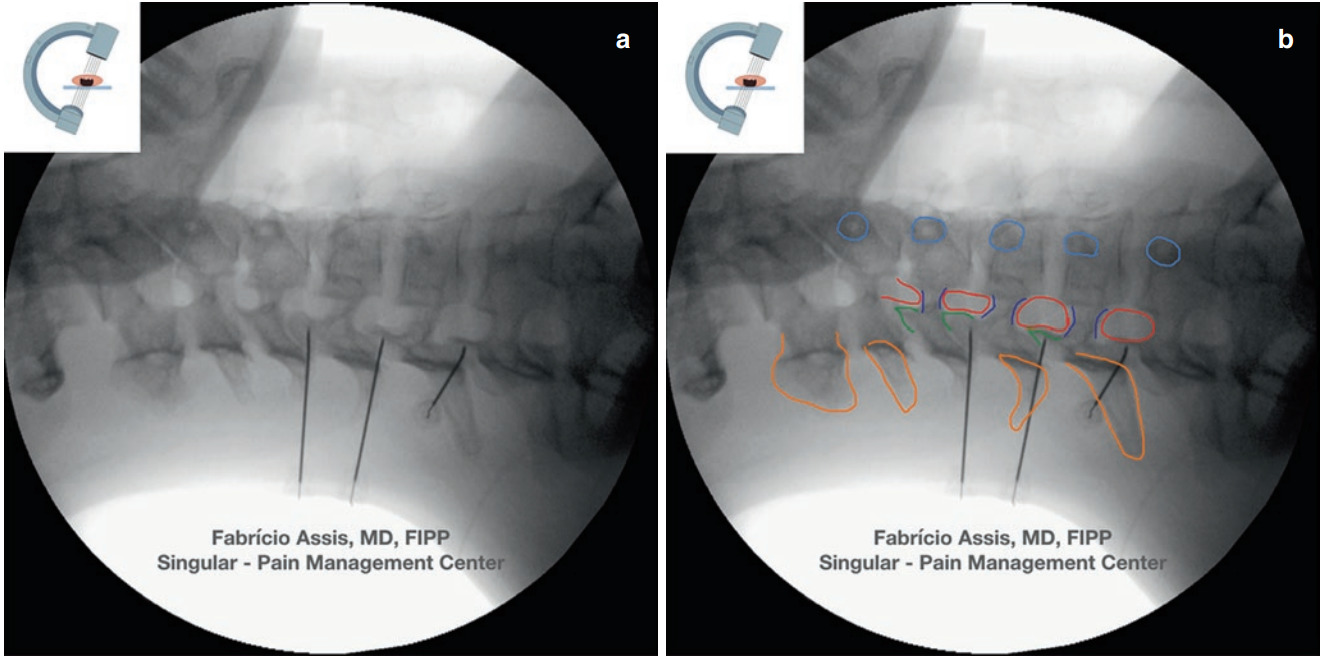
- The entry point for all levels is just lateral to the vertebral body, caudad to the rib (Fig. 4a, b)
- Advance the needle in a coaxial view until touching the vertebral body
- Lateral view to confirm the depth of needle
- Slip the needle smoothly along the vertebral body anteriorly and medially until it reaches the junction of anterior one third and posterior two thirds of the lateral surface of the vertebral body (Fig. 5a, b)
- Return to AP view to confirm the position of the tip of the needle
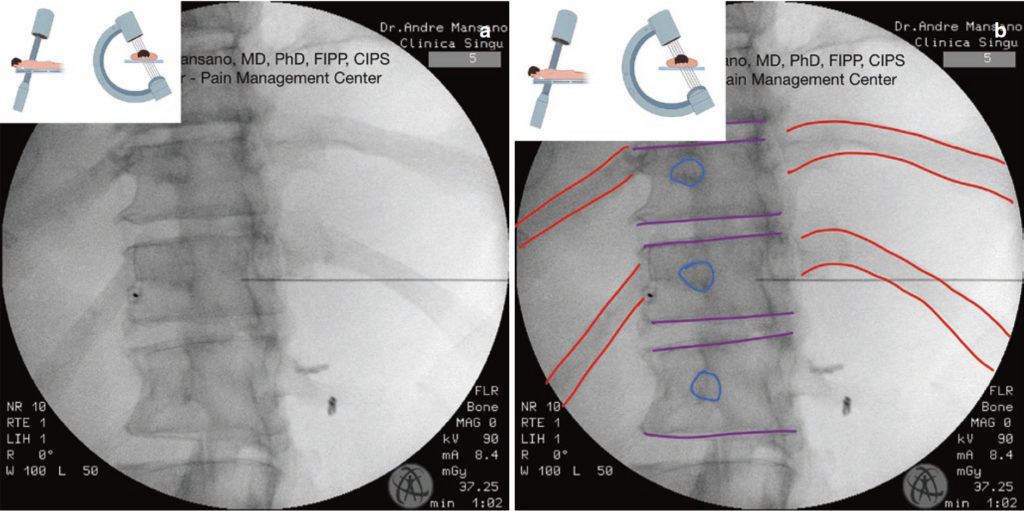
Fig. 4 Oblique view of the thoracic spine. Note the entry point at the left side just lateral to the vertebral body under the rib. The right needle is already in place. Blue = pedicle; purple = endplates; red = ribs. Native (a) and edited (b) fluoroscopy image
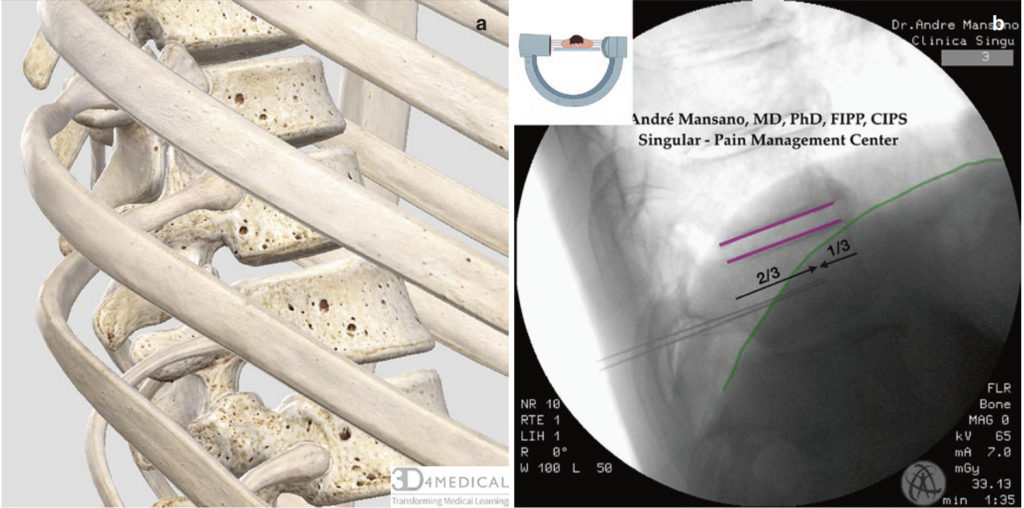
Fig. 5 Lateral view of the thoracic spine. Note the final position of the needles at the anterior third of the vertebral body. Green = diaphragm; purple = vertebral body endplates. Complete Anatomy image (a), edited fluoroscopy image (b)
For diagnostic block:
- Aspirate for fluid (blood, cerebrospinal fluid (CSF) or chyle)
- Inject 1–3 ml of nonionic contrast media (Fig. 6)
- Check the optimal dispersion of the contrast media in AP and lateral view. The contrast media must “hug” the vertebral body laterally (Fig. 7a, b)
- Inject 5–8 ml of local anesthetic
- The procedure must be performed bilaterally
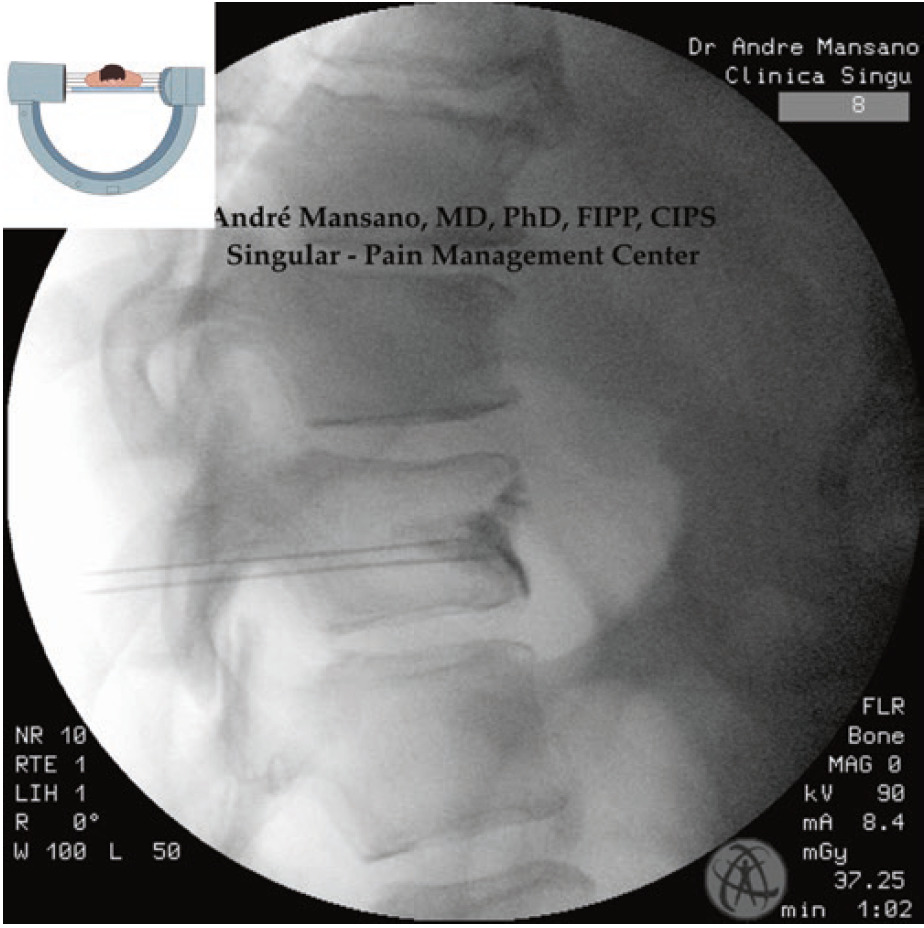
Fig. 6 Lateral view. Splanchnic nerve block. Note the optimal contrast media dispersion. Native fluoroscopy image
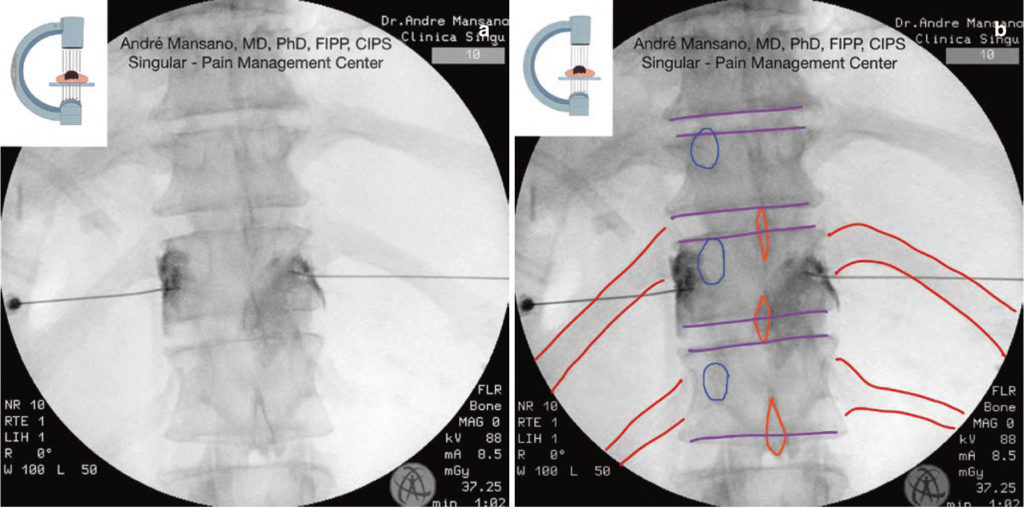
Fig. 7 AP view of the thoracic spine. Splanchnic nerve block. Note the contrast media dispersion “hugging” the vertebral body laterally. Red = ribs; orange = spinous process; purple = vertebral body endplates. Native (a) and edited (b) fluoroscopy image
For chemical neurolysis:
- Aspirate for fluid (blood, CSF, or chyle)
- Inject 1–3 ml of nonionic contrast media
- Check the optimal dispersion of the contrast media in AP and lateral view. The contrast media must “hug” the vertebral body laterally
- Inject 4–8 ml of phenol 6–10% (not painful) or alcohol 80% after local anesthetic (otherwise extremely painful)
- The procedure must be performed bilaterally
For radiofrequency (RF):
- Perform sensory and motor stimulation: At 50 Hz, the sensory stimulation is conducted up to 1 V. The patient may report stimulation in the epigastric region. If the stimulation is in a girdle-like fashion around the intercostal spaces, then the needle needs to be advanced anteriorly. At 2 Hz, motor stimulation is conducted up to 2 V, while checking for intercostal muscle contraction. If this is negative, then test stimulation is satisfactory.
- Inject 2–3 ml of local anesthetic
- Perform the RF lesion (60–90 seconds, 80 C). Turn the RF needle 180 and perform another lesion
- The procedure must be performed bilaterally
6. CLINICAL PEARLS
- There are also approaches at T12 (target: anterior third of the vertebral body on lateral view) and T10 the (target: middle of the vertebral body on lateral view)
- The occurrence of pneumothorax is the primary complication. Its occurrence can be avoided by keeping the needle in close proximity to the vertebral body
- The chemical neurolysis can be harmful, especially if the solution disperses backwards to the exiting nerve root. Look carefully at the contrast media dispersion
- All patients must receive an intravenous infusion of 500 ml crystalloids to prevent hypotension caused by splanchnic vasodilatation
7. UNACCEPTABLE, POTENTIAL HARMFUL NEEDLE PLACEMENT
- Rough needle manipulation
- Needle too lateral (risk of pneumothorax)
- Not checking multiple fluoroscopy views (AP and lateral)
- Needle anterior to vertebral body (risk of great vessel puncture)
- Any position in the spinal canal
- Any proof of lack of understanding of thoracic spine anatomy, for example leaving the needle between the spinous processes and believing it is the right place
8. UNACCEPTABLE, BUT NOT HARMFUL NEEDLE PLACEMENT
- Use of large bore needles (increased risk of pneumothorax)
- Procedure at inappropriate level
- Disc puncture
- The procedure was abandoned after unsuccessful attempts, but it was clear that the examinee was cognizant of the safety aspects of the procedure, the needle did not compromise vital structures, did not reach
Enriched with NextLevel CME™ technology:
– Make notes in seconds and never lose them
– Insert your own images, infographics
– Add and watch videos inside your notes
– Attach PDFs, articles, website links
– Listen to the audio