Learning objectives
- Definition of opioid tolerance
- Adverse effects of methadone and buprenorphine
- The pre-, peri- and postoperative management of opioid-tolerant or methadon-using patients
Definition and mechanisms
- Opioid tolerance is a process characterized by neuroadaptations that result in reduced drug effects, and more specifically, opioid tolerance is:
- Characterized by reduced responsiveness to an opioid agonist such as morphine
- Usually manifested by the need to use increasing doses to achieve the desired effect
- A common occurrence in individuals taking high doses of opioids for extended periods
- Addiction to opioids is common among recreational opioid users (heroin), but relatively rare in chronic pain patients
- The six most common clinically used opioids are morphine, oxycodone, hydromorphone, fentanyl, buprenorphine, and methadone
- Successful approaches to pharmacotherapy of opioid addiction continue to rely largely on the substitution of short-acting agonists such as heroin with oral administration of long-acting high-efficacy agonists such as methadone or partial agonists buprenorphine
- Methadone
- Is a synthetic opioid agonist used as an analgesic for chronic pain (often in rotation with other opioids) and also for opioid dependence
- A μ-agonist as well as an NMDA-antagonist and monoamine reuptake inhibitor
- Relieves cravings and removes withdrawal symptoms
- Detoxification using methadone can be accomplished in less than a month
- Buprenorphine
- Is an opioid used to treat opioid use disorder, acute pain, and chronic pain
- A partial agonist at μ-receptors and an antagonist at κ- and δ-receptors
- It is used in addiction medicine to suppress opioid withdrawal and craving for 24–48 hours
Adverse effects
| Methadone | Buprenorphine |
|---|---|
| Sedation Constipation Flushing Perspiration Heat intolerance Dizziness Weakness Chronic fatigue Insomnia Constricted pupils Dry mouth Nausea and vomiting Hypotension Headache Tachycardia Abnormal heart rhythms Trouble breathing, slow or shallow breathing Weight gain Memory loss Itching Difficulty urinating Swelling of the hands, arms, feet, and legs Mood changes, euphoria, disorientation Blurred vision Skin rash Central sleep apnea | Nausea and vomiting Drowsiness Dizziness Headache Memory loss Cognitive and neural inhibition Perspiration Itching Dry mouth Constricted pupils Hypotension Urinary retention Respiratory depression |
Preoperative management
- Obtain a detailed medical history
- Perform a physical exam
- Obtain pain history and medication history
Perioperative management
- Assessment and monitoring
- Assess the overall effectiveness of the pain management
- Consider other important factors such as the presence of opioid-related side-effects, signs of opioid withdrawal, patient expectations, patient satisfaction, mood, and levels of physical function
- Acute pain management plan
- Identify complex patients early
- Adhere to a clear multi-disciplinary pain management plan
- Consider opioid-sparing techniques
- Opioid-sparing techniques
- Use paracetamol, NSAIDs or COX-2s
- Use local, regional, or neuraxial anesthesia where possible
- Administer ketamine in a low dose as a continuous i.v. or subcutaneous infusion for 1–3 days in the acute pain management of opioid-tolerant patients
- Consider the use of:
- Gabapentinoids (e.g. gabapentin/pregabalin)
- IV lidocaine infusions
- Prevention of withdrawal
- Maintain the usual 24-hour opioid dose and continue the patient’s baseline opioid into the postoperative period
- Convert the dose of oral morphine to i.v. morphine
- Manage acute post-surgical pain with the addition of an appropriate dose of immediate-release opioids
- Continue the use of a buprenorphine path (up to 70 µg/h) as this is unlikely to interfere with the use of full opioid agonists
- The patient may need parenteral replacement if unable to take oral opioids
- Additional opioids
- Note that opioid-tolerant patients may require a greater amount of immediate-release oral opioids than expected
- Consider IV patient-controlled analgesia and base the size of the bolus dose on the patient’s usual 24-hour opioid requirement
- Opioid rotation
- Switch from one opioid to another to improve pain relief and to reduce side-effects
- Reduce the calculated equianalgesic dose by 30–50% because of the possibility of incomplete crosstolerance
- Converting back from IV to oral opioid
- Identify the i.v. opioid consumption in the previous 24 hours and convert this to an equivalent oral dose
- Administer 50% of this oral equivalent dose in a sustained-release form and prescribe 1/6th of the equivalent dose as an immediate-release preparation every four hours
- Opioid tolerance or opioid-induced hyperalgesia
- Increase the opioid dose or consider an opioid rotation in opioid-tolerant patients
- Reduce the opioid dose in opioid-induced hyperalgesia patients
- Substance abuse and substitution therapy
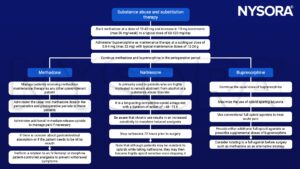
Postoperative management
- Methadone
- Continue preoperative dose
- Continue the multimodal pain management
- Buprenorphine
- Continue preoperative dose
- If not on the maximal dose, increase the dose to 24-32 mg/day, divide the daily dose to every 6-8 hours
- Continue the multimodal pain management
- Consider converting buprenorphine to methadone to prevent acute withdrawal
Suggested reading
- Srivastava, D., Hill, S., Carty, S., Rockett, M., Bastable, R., Knaggs, R., Lambert, D., Levy, N., Hughes, J., Wilkinson, P., 2021. Surgery and opioids: evidence-based expert consensus guidelines on the perioperative use of opioids in the United Kingdom. British Journal of Anaesthesia 126, 1208–1216.
- Sritapan Y, Clifford S, Bautista A. Perioperative Management of Patients on Buprenorphine and Methadone: A Narrative Review. Balkan Med J. 2020;37(5):247-252.
- Simpson, G., Jackson, M., 2017. Perioperative management of opioid-tolerant patients. BJA Education 17, 124–128.
- Rajan, J., Scott-Warren, J., 2016. The clinical use of methadone in cancer and chronic pain medicine. BJA Education 16, 102–106.
- Morgan MM, Christie MJ. Analysis of opioid efficacy, tolerance, addiction and dependence from cell culture to human. Br J Pharmacol. 2011;164(4):1322-1334.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com