Thomas F. Bendtsen, Ana M. Lopez, and Catherine Vandepitte
FACTS
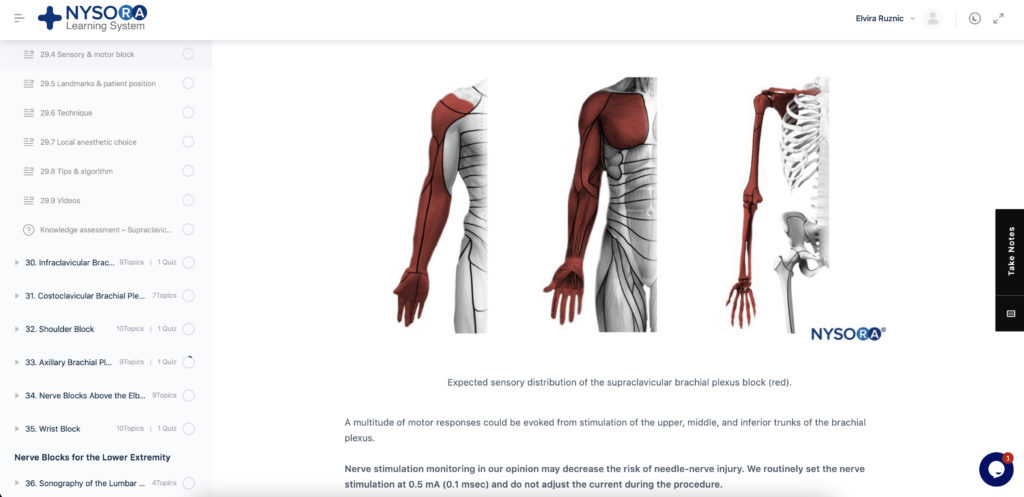
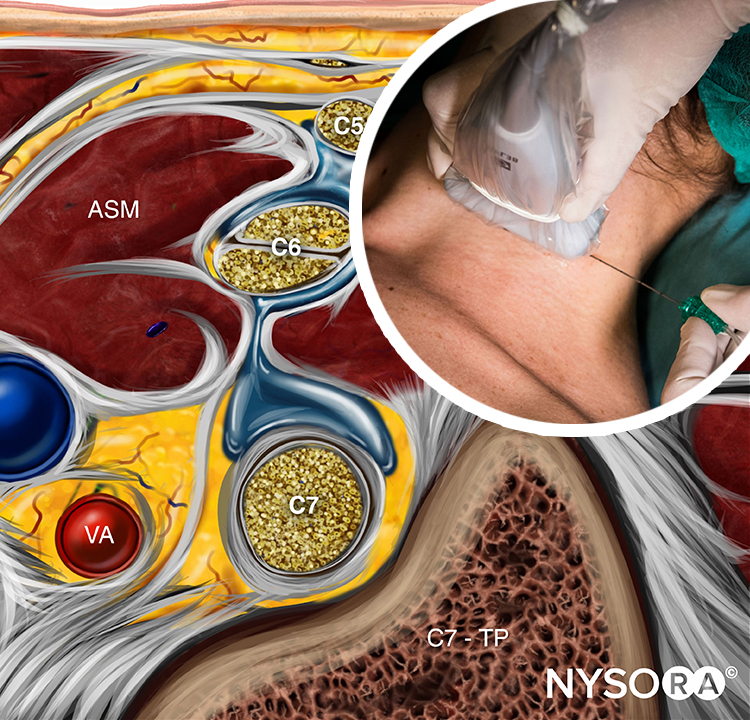
- Indications: Arm, elbow, forearm, hand surgery; anesthesia for shoulder surgery is also possible (Figure 1).
- Transducer position: Transverse on the neck, superior to the clavicle at the midpoint (Figure 1)
- Goal: Local anesthetic spread around the brachial plexus, posterior and superficial to the subclavian artery
- Local anesthetic: 20–25 mL
GENERAL CONSIDERATIONS
At this location, the proximity of the brachial plexus to the chest cavity and pleura had been of concern (Figure 2) until ultrasound (US) guidance renewed interest in the supraclavicular approach to the brachial plexus nerve block. The ability to image the plexus, rib, pleura, and subclavian artery with US has increased safety due to improved monitoring of anatomy and needle placement. Because the trunks and divisions of the brachial plexus are relatively close as they pass over the first rib, the extension and quality of anesthesia are favorable. For these reasons, the supraclavicular nerve block has become a commonly used technique for surgery of the upper limb distal to the shoulder.
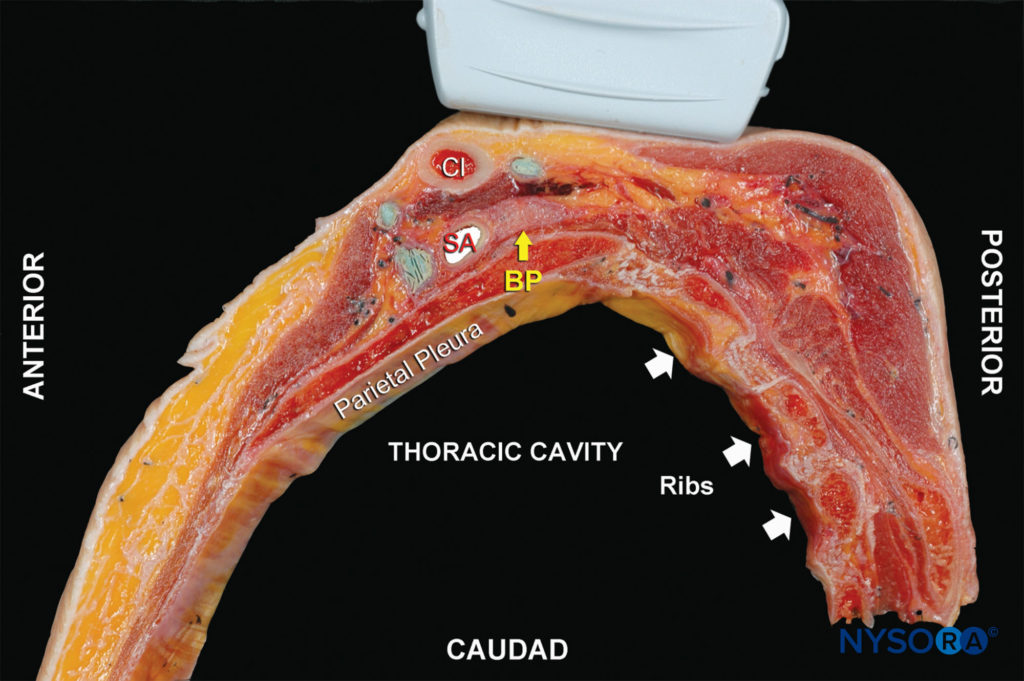
FIGURE 2. Anatomy of the supraclavicular brachial plexus with proper transducer placement slightly oblique above the clavicle (Cl). Yellow arrow: brachial plexus (BP). SA, subclavian artery.
ULTRASOUND ANATOMY
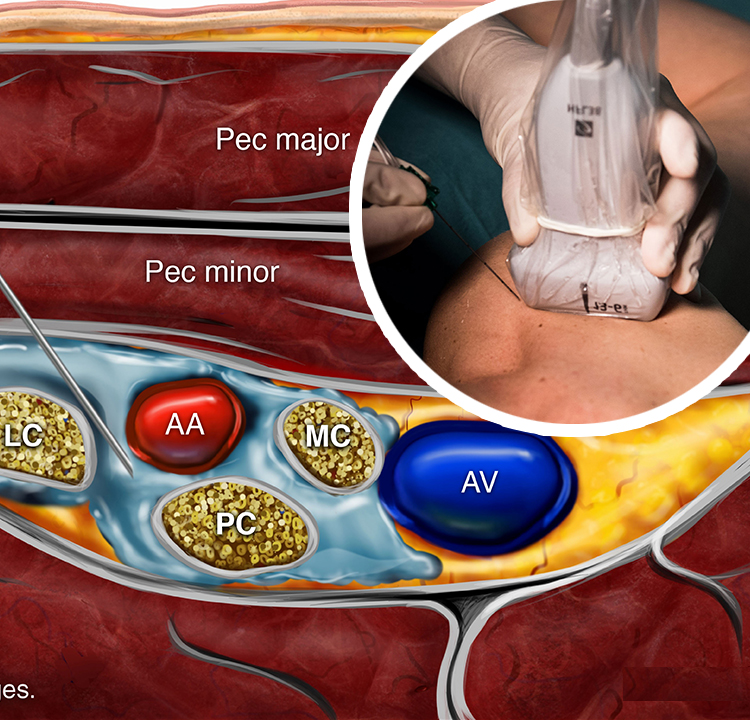
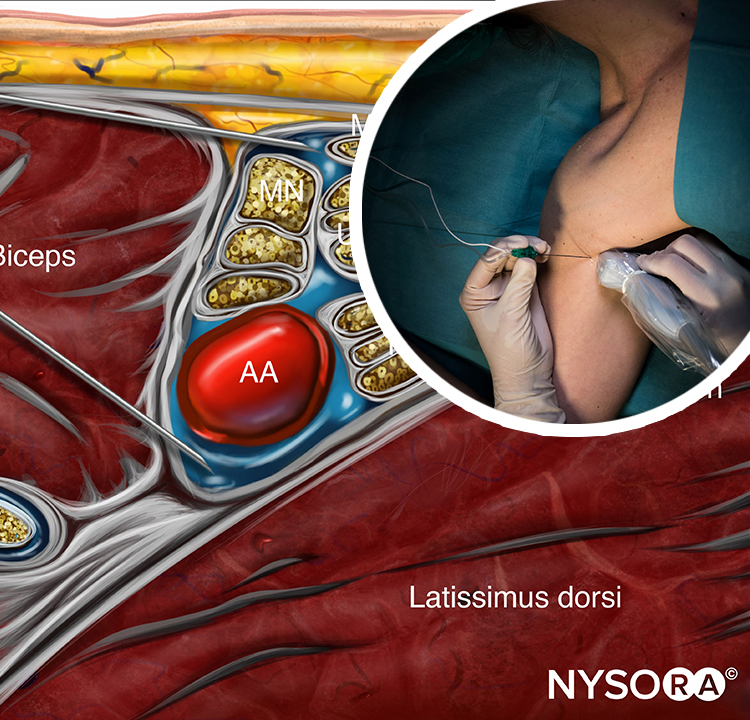
The subclavian artery crosses over the first rib between the insertions of the anterior and middle scalene muscles, posterior to the midpoint of the clavicle. The subclavian artery is readily apparent as an anechoic round structure, whereas the parietal pleura and the first rib can be seen as a linear hyperechoic structure immediately lateral and deep to the subclavian artery (Figure 3). The rib casts an acoustic shadow so that the image field deep to the rib appears anechoic.2 The brachial plexus can be seen as a bundle of hypoechoic round nodules just posterior and superficial to the artery (Figures 3 and 4). It is often possible to see the fascial sheath of the muscles surrounding the brachial plexus. Adjusting the transducer orientation, the upper, middle and lower trunks of the brachial plexus can be individually identified, as they join together at the costoclavicular space. To visualize the lower trunk, the transducer is oriented in the sagittal plane, until the first rib is seen deep to the plexus and the artery. (Figure 4). Anterior or posterior to the first rib is the hyperechoic pleura, with lung tissue deep to it. This structure can be confirmed by observing a “sliding” motion of the viscera pleura in synchrony with the patient’s respiration. The brachial plexus is typically visualized at a 1- to 2-cm depth at this location. The presence of two separate clusters of elements of the brachial plexus may be more or less obvious, sometimes with separation by a blood vessel (Figure 4). The dorsal scapular artery commonly passes through or within the vicinity of the brachial plexus. It is important to recognize that the more superficial and lateral branches come from C5–C7 (shoulder, lateral aspect of arm, and forearm) and can be tracked up to the interscalene area, whereas the deeper and more medial contingent are branches of C8 and T1 (hand and medial aspect of forearm). Adequate spread of local anesthetic in both areas is necessary for successful nerve block of the arm and hand. For additional information see Functional Regional Anesthesia Anatomy.
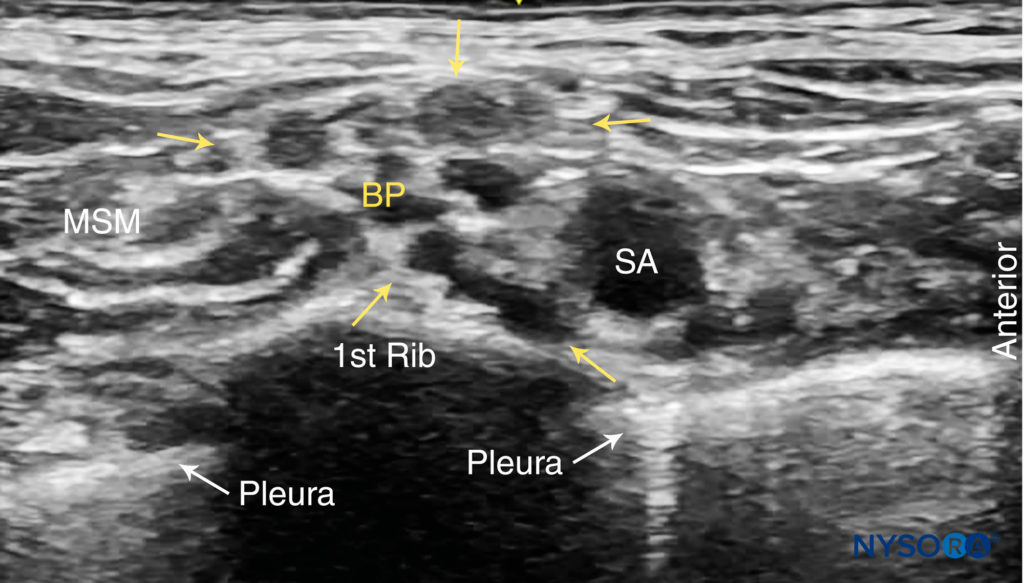
FIGURE 3. Supraclavicular brachial plexus (BP; yellow arrows) seen slightly superficial and posterolateral to the subclavian artery (SA). The brachial plexus is enveloped by a connective tissue sheath. Note the intimate location of the pleura and lung to the brachial plexus and subclavian artery. MSM, middle scalene muscle.
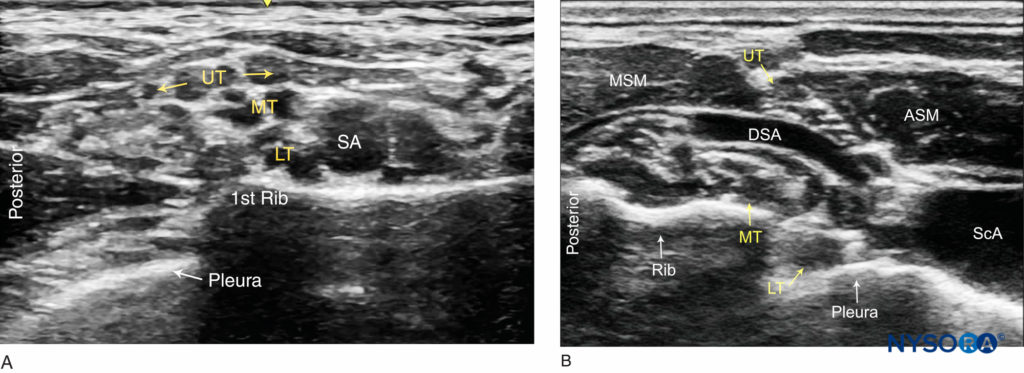
FIGURE 4. Ultrasound images of the brachial plexus cephalad to the clavicle. (A) Sagittal view: The upper (UT), Middle (MT) and lower (LT) trunks of the brachial plexus are seen posterior to the subclavian artery (SA) and superficial to the first rib. (B) Oblique view: The upper trunk (UT) is positioned between the anterior (ASM) and middle (MSM) scalene muscles. The lower trunk (LT) and the subclavian artery are superficial to the pleura.
From the Compendium of Regional Anesthesia: Cognitive priming for a supraclavicular brachial plexus block.
DISTRIBUTION OF ANESTHESIA
The supraclavicular approach to the brachial plexus block results in anesthesia of the upper limb including often the shoulder because all trunks and divisions can be anesthetized from this location. The skin of the proximal part of the medial side of the arm (intercostobrachial nerve, T2), however, is never anesthetized by any technique of the brachial plexus nerve block and, when necessary, can be blocked by an additional subcutaneous injection just distal to the axilla (Figure 1). For a more comprehensive review of the brachial plexus anatomy and distribution, see Functional Regional Anesthesia Anatomy.
EQUIPMENT
The equipment needed for a supraclavicular brachial plexus nerve block includes the following:
• Ultrasound machine with linear transducer (8–18 MHz), sterile sleeve, and gel (or other acoustic coupling agent; eg, saline)
• Standard nerve block tray
• 20–25 mL local anesthetic
• 5-cm, 22-gauge, short-bevel, insulated stimulating needle
• Peripheral nerve stimulator
• Opening injection pressure monitoring system
• Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks here.
LANDMARKS AND PATIENT POSITIONING
Any position that allows for comfortable placement of the ultrasound transducer and needle advancement is appropriate. This nerve block can be performed with the patient in the supine, semi-sitting, or slight lateral position, with the patient’s head turned away from the side to be blocked. When possible, asking the patient to reach for the ipsilateral knee will depress the clavicle slightly and allow better access to the structures of the anterolateral neck. Knowledge of the underlying anatomy and the position of the brachial plexus in relation to the subclavian artery, first rib, and pleura is important for the success and safety of the technique. Scanning is usually started just above the clavicle, approximately at its midpoint.
GOAL
The goal of this nerve block is to place the needle within the brachial plexus sheath posterior to the subclavian artery and inject local anesthetic to surround the trunks and divisions of the brachial plexus at this level.
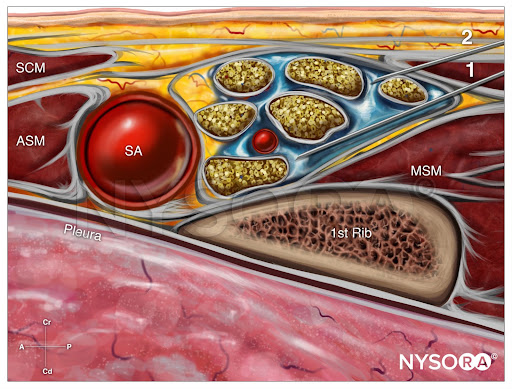
From the Compendium of Regional Anesthesia: Reverse Ultrasound Anatomy for a supraclavicular brachial plexus block with needle insertion in-plane and local anesthetic spread (blue). SCM, sternocleidomastoid muscle; ASM, anterior scalene muscle; SA, subclavian artery; MSM, middle scalene muscle.
TECHNIQUE
With the patient in the proper position, the skin is disinfected and the transducer is positioned in the transverse plane immediately proximal to the clavicle, slightly posterior to at its midpoint. The transducer is tilted caudally, as if to image the chest contents, to obtain a cross-sectional view of the subclavian artery (Figure 5). The brachial plexus is seen as a collection of hypoechoic oval structures posterior and superficial to the artery. Color Doppler should be routinely used prior to needle insertion to rule out the passage of large vessels (ie, dorsal scapular artery, transverse cervical artery, suprascapular artery) in the anticipated trajectory of the needle.
NYSORA Tips
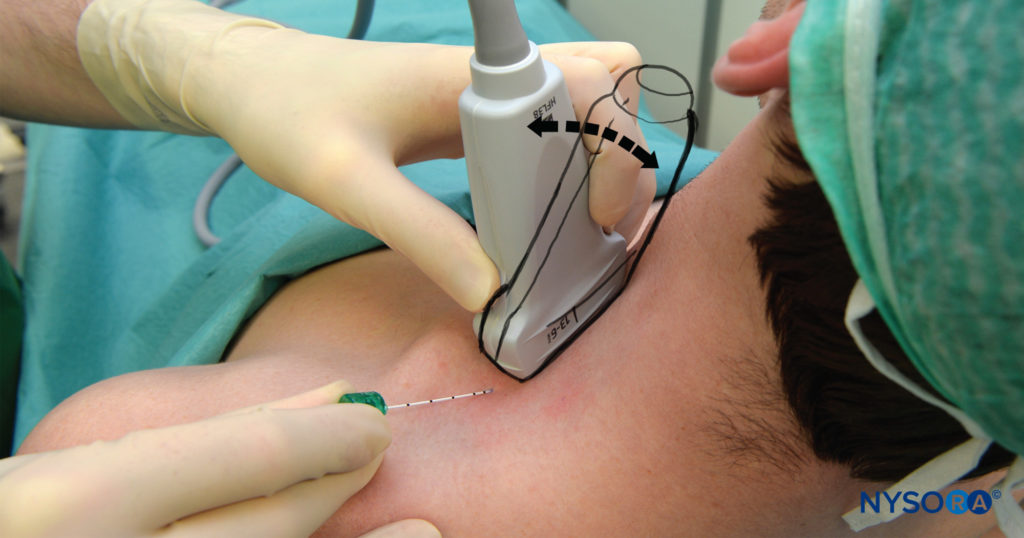
FIGURE 5. Supraclavicular brachial plexus nerve block: transducer position just proximal the clavicle and needle insertion. The brachial plexus is very shallow at this location, typically 1–3 cm; therefore, inclination of the needle should be equally shallow. The image also shows the caudal tilt that is useful in obtaining best image of the plexus
• To achieve the best possible view, the transducer often must be tilted slightly inferiorly (see arrows in Figure 5). The goal is to see the subclavian artery in the transverse view and the brachial plexus just superficial and posterior to the subclavian artery, enclosed within the brachial plexus sheath. Transducer rotation clockwise often facilitate best imaging of the tissue space (sheath) containing the plexus.
Using a 25- to 27-gauge needle, 1–2 mL of local anesthetic is injected into the skin 1 cm lateral to the transducer to decrease discomfort during needle insertion. To avoid inadvertent puncture of and injection into the brachial plexus, the needle should not be initially inserted deeper than 1 cm. The distribution of local anesthetic via small-volume injections is observed as the needle advances through tissue layers (hydro-localization); small-volume injections are used to avoid inadvertent needle insertion into the brachial plexus. The nerve block needle is then inserted in plane toward the brachial plexus, in a lateral-to-medial direction (Figures 5 and 6).
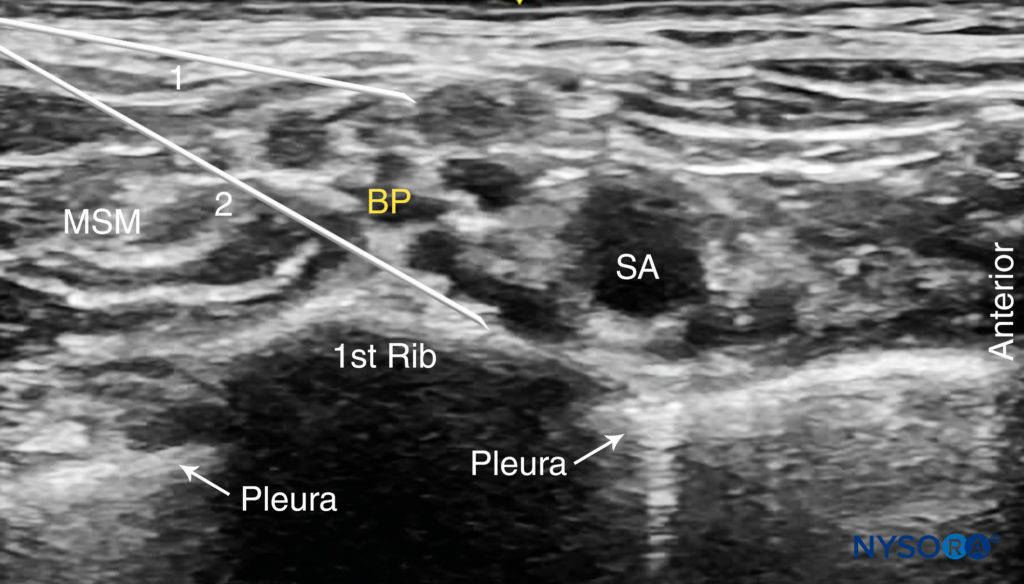
FIGURE 6. Supraclavicular brachial plexus nerve block: needle path and two separate injections required for nerve block of the brachial plexus. Two needle positions (1 and 2) are used to inject local anesthetic within the connective tissue sheath (arrows) containing the brachial plexus (BP).
Nerve stimulation (0.5 mA, 0.1 msec), is often associated with a motor response of the arm, forearm, or hand. Note, however, that motor response may be absent despite accurate needle placement. Insertion of the needle into the sheath is often associated with a palpable “pop.” After careful aspiration, 1–2 mL of local anesthetic is injected to confirm proper needle placement. When the injection displaces the brachial plexus away from the needle, an additional advancement of the needle 1–2 mm closer to the plexus may be required to accomplish adequate local anesthetic spread (Figures 7, 8, and 9). When the injection of local anesthetic does not appear to result in a spread around the brachial plexus, needle repositioning may be necessary. Typically, 20–25 mL of local anesthetic is required for adequate nerve block. It has been suggested that lower volumes can be used in older patients. (see Figure 7). Supplementary video related to this nerve block can be found at Ultrasound-Guided Supraclavicular Brachial Plexus Nerve Block Video.
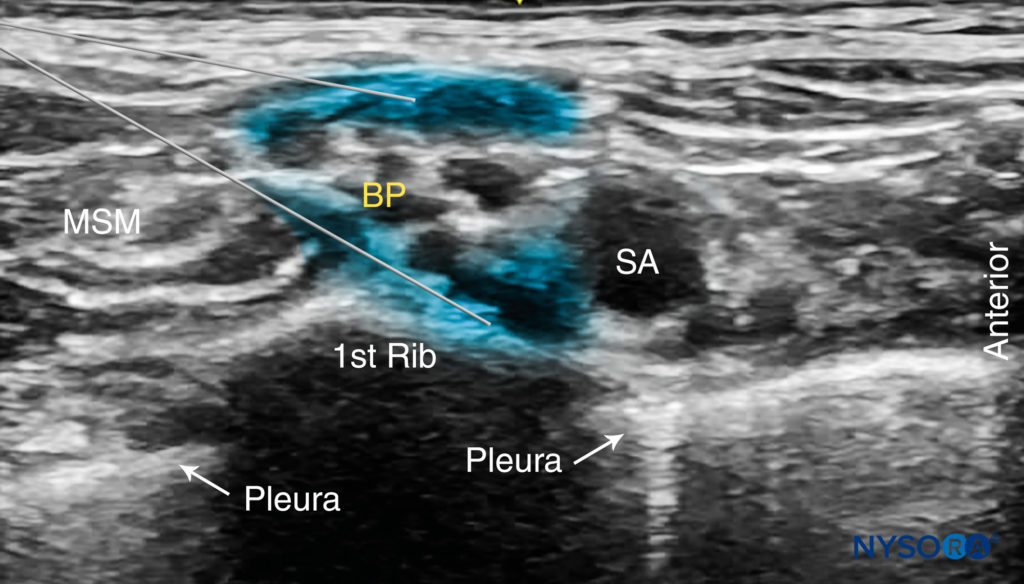
FIGURE 7. The desired spread of local anesthetic (blue-shaded areas) in two different needle positions to accomplish brachial plexus (BP) nerve block. Local anesthetic should spread within the connective tissue sheath resulting in separation of the brachial plexus trunks posterior to the subclavian artery (SCA).
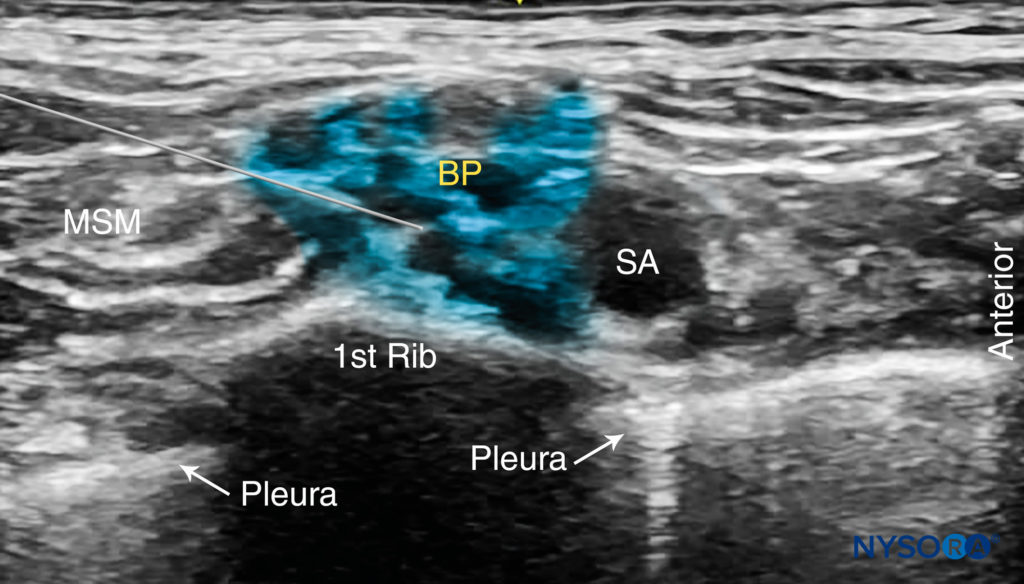
FIGURE 8. Ultrasound image simulating needle path and expected local anesthetic spread after a single injection within the connective tissue sheath surrounding the brachial plexus. Additional monitoring (eg, nerve stimulation and injection pressure) is recommended to decrease the risk of intrafascicular injection.
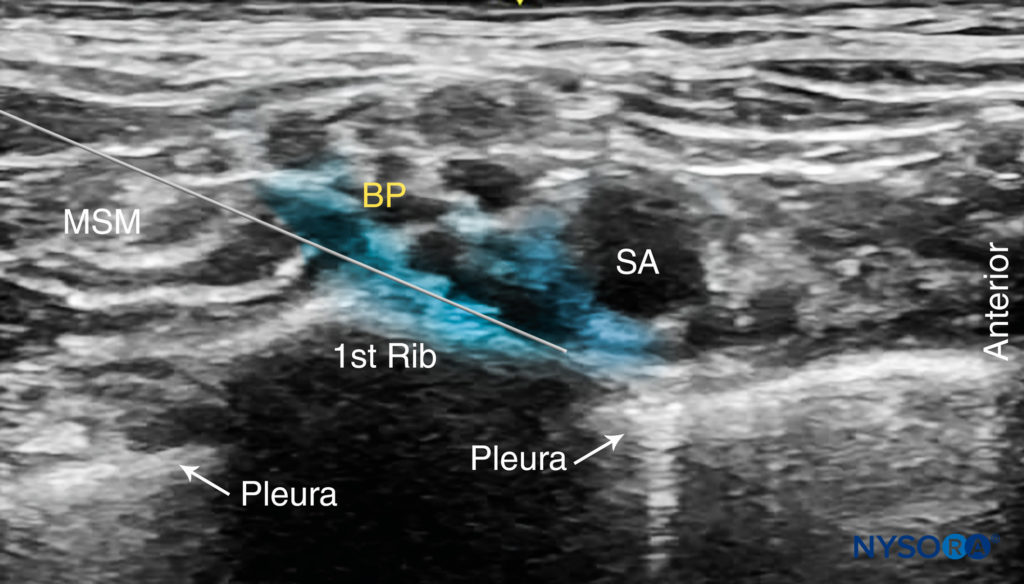
FIGURE 9. Ultrasound-guided supraclavicular brachial plexus nerve block simulating a single injection between the subclavian artery (SA) and the first rib.
TIPS
• A motor response to nerve stimulation is not necessary if the plexus, needle, and local anesthetic spread are well visualized.
• The neck is a highly vascular area, and care must be exercised to avoid needle placement or injection into the vascular structures. Of particular importance is to note the intimately located subclavian artery and dorsal scapular artery, which often cross the brachial plexus at this level. Other vessels can be found within the vicinity of the brachial plexus, such as the suprascapular artery and the transverse cervical artery. The use of color Doppler before needle placement and injection is highly recommended.
• Pneumothorax (The presence of air or gas in the cavity between the lungs and the chest wall, causing collapse of the lung) is also a rare but possible complication, typically delayed rather than immediate, therefore, it is paramount to keep the needle tip visible at all times.
• Never inject against high resistance to injection. The inability to initiate injection with an opening injection pressure of less than 15 psi may signal an intrafascicular injection.
• Multiple injections
• May increase the speed of onset and the success rate.
• May allow for a reduction in the required volume of local anesthetic.
• May carry a higher risk of nerve injury.
CONTINUOUS ULTRASOUND-GUIDED SUPRACLAVICULAR NERVE BLOCK
The ultrasound-guided continuous supraclavicular nerve block is in many ways similar to the technique used for interscalene catheter placement. The goal is to place the catheter within the vicinity of the trunks and divisions of the brachial plexus adjacent to the subclavian artery. The procedure consists of three phases: (1) needle placement; (2) catheter advancement; and (3) securing the catheter. For the first two steps of the procedure, ultrasound can be used to ensure accuracy in most patients. The needle is typically inserted in plane from the lateral-to-medial direction so that the tip is just posterior to the brachial plexus sheath. The needle is then advanced to pierce the sheath, followed by catheter placement. For additional information see Continuous Peripheral Nerve Blocks: Local Anesthetic Solutions and Infusion Strategies.
NYSORA Tips
• The risk of phrenic nerve palsy is lower than with the interscalene nerve block but cannot be reliably avoided. Therefore, in patients who cannot tolerate a 27–30% decrease in respiratory function with phrenic block, an axillary or infraclavicular nerve block is a better choice of anesthesia for upper extremity surgery.
Two main disadvantages of tunneling are the risk of catheter dislodgement during the tunneling and the potential for scar formation. A number of devices are commercially available to help secure the catheter. The starting infusion regimen is typically 5-8 mL/h of 0.2% ropivacaine of bupivacaine 0.125% with 3-5 mL patient-controlled boluses hourly. A catheter-over-needle technique has also been described.
To learn more about this nerve block, see Supraclavicular Brachial Plexus Nerve Block – Landmarks and Nerve Stimulator Technique
This text was a sample of content from the Compendium of Regional Anesthesia on the NYSORA LMS.
NYSORA’s Compendium of Regional Anesthesia is simply the most comprehensive, and practical curriculum on Regional Anesthesia from A to Z, featuring NYSORA’s Premium content. As opposed to textbooks and e-books, the Compendium is continuously updated and features NYSORA’s newest videos, animations, and visual content.
The Compendium is one of several gold-standard educational courses on NYSORA’s Learning System (the NYSORA LMS), and registration to NYSORALMS.com is free. The FULL access to the Compendium, however, is based on an annual subscription, as it requires an army of illustrators, video editors, and an educational team to continue making it the BEST tool for education on everything regional anesthesia. While you can think of the compendium as an ebook on steroids, a quick test drive will give you a real-time feel of how incredible the Compendium really is. Your subscription will transform the way you read about regional anesthesia:
- Learn visually: Everything regional, including spinal, epidural, and nerve block procedures and management protocols
- Review step-by-step techniques instructions for over 60 nerve blocks
- Access NYSORA’s fabled illustrations, animations, and videos (such as Reverse Ultrasound Anatomy)
- Access RA info on any device via the desktop platform and mobile app
- Get real-time updates
- Review infographics for exam preparation (e.g. EDRA)
- Use the Community feed with real case discussions, images and videos are posted and discussed by subscribers and world’s top experts alike.
Even if you do not wish to subscribe to the Compendium, do register to the NYSORA LMS, be the first to know what’s new in regional anesthesia, and get involved in case discussions.
Here’s what the activity feed on NYSORA LMS looks like:
We are convinced that once you experience the Compendium on the NYSORA LMS, and you’ll never go back to your old books, and your subscription will support keeping NYSORA.com free for the rest of the world.
Additional Reading
- Liu SS, Gordon MA, Shaw PM, Wilfred S, Shetty T, Yadeau JT: A prospective clinical registry of ultrasound-guided regional anesthesia for ambulatory shoulder surgery. Anesth Analg 2010;111:617–623.
- Hebbard PD: Artifactual mirrored subclavian artery on ultrasound imaging for supraclavicular nerve block. Can J Anaesth 2009;56:537–538
- Abrahams MS, Panzer O, Atchabahian A, Horn JL, Brown AR: Case report: limitation of local anesthetic spread during ultrasound-guided interscalene nerve block. Description of an anatomic variant with clinical correlation. Reg Anesth Pain Med 2008;33:357–359.
- Murata H, Sakai A, Hadzic A, Sumikawa K: The presence of transverse cervical and dorsal scapular arteries at three ultrasound probe positions commonly used in supraclavicular brachial plexus block. Anesth Analg 2012;115:470–473.
- Pavičić Šarić J, Vidjak V, Tomulić K, Zenko J: Effects of age on minimum effective volume of local anesthetic for ultrasound-guided supraclavicular brachial plexus nerve block. Acta Anaesthesiol Scand 2013;57:761–766.
- Murata H, Sakai A, Sumikawa K: A venous structure anterior to the brachial plexus in the supraclavicular region. Reg Anesth Pain Med 2011; 36:412–413.
- Snaith R, Dolan J: Preprocedural color probe Doppler scanning before ultrasound-guided supraclavicular nerve block. Anesth Pain Med 2010;35:223.
- Guirguis M, Karroum R, Abd-Elsayed AA, Mounir-Soliman L: Acute respiratory distress following ultrasound-guided supraclavicular nerve block. Ochsner J 2012;12:159–162.
- Bhatia A, Lai J, Chan VW, Brull R: Case report: pneumothorax as a complication of the ultrasound-guided supraclavicular approach for brachial plexus nerve block. Anesth Analg 2010;111:817–819.
- Abell DJ, Barrington MJ: Pneumothorax after ultrasound-guided supraclavicular nerve block: presenting features, risk, and related training. Reg Anesth Pain Med 2014;39:164–167.
- Gauss A, Tugtekin I, Georgieff M, Dinse-Lambracht A, Keipke D, Gorsewski G: Incidence of clinically symptomatic pneumothorax in ultrasound-guided infraclavicular and supraclavicular brachial plexus nerve block. Anaesthesia 2014;69:327–336.
- Kumari A, Gupta R, Bhardwaj A, Madan D: Delayed pneumothorax after supraclavicular nerve block. J Anaesthesiol Clin Pharmacol 2011;27:121–122.
- Kakazu C, Tokhner V, Li J, Ou R, Simmons E: In the new era of ultrasound guidance: is pneumothorax from supraclavicular nerve block a rare complication of the past? Br J Anaesth 2014;113:190–191.
- Tran DQ, Muñoz L, Zaouter C, Russo G, Finlayson RJ: A prospective, randomized comparison between single- and double-injection, ultrasound-guided supraclavicular brachial plexus nerve block. Reg Anesth Pain Med 2009;34:420–424.
- Techasuk W, González AP, Bernucci F, Cupido T, Finlayson RJ, Tran DQ: A randomized comparison between double-injection and targeted intracluster-injection ultrasound-guided supraclavicular brachial plexus nerve block. Anesth Analg 2014;118:1363–1369.
- Arab SA, Alharbi MK, Nada EM, Alrefai DA, Mowafi HA: Ultrasound-guided supraclavicular brachial plexus nerve block: single versus triple injection technique for upper limb arteriovenous access surgery. Anesth Analg 2014;118:1120–1125.
- Ip VH, Tsui BC: The catheter-over-needle assembly facilitates delivery of a second local anesthetic bolus to prolong supraclavicular brachial plexus nerve block without time-consuming catheterization steps: a randomized controlled study. Can J Anaesth 2013;60:692–699.
- Aguirre J, Ekatodramis G, Ruland P, Borgeat A: Ultrasound-guided supraclavicular nerve block: is it really safer? Reg Anesth Pain Med 2009;34:622.
- Arcand G, Williams SR, Chouinard P, et al: Ultrasound-guided infraclavicular versus supraclavicular nerve block. Anesth Analg 2005;101:886–890.
- Beach ML, Sites BD, Gallagher JD: Use of a nerve stimulator does not improve the efficacy of ultrasound-guided supraclavicular nerve blocks. J Clin Anesth 2006;18:580–584.
- Bigeleisen PE, Moayeri N, Groen GJ: Extraneural versus intraneural stimulation thresholds during ultrasound-guided supraclavicular nerve block. Anesthesiology 2009;110:1235–1243.
- Chan VW, Perlas A, Rawson R, Odukoya O: Ultrasound-guided supraclavicular brachial plexus nerve block. Anesth Analg 2003;97:1514–1517.
- Chin KJ, Niazi A, Chan V: Anomalous brachial plexus anatomy in the supraclavicular region detected by ultrasound. Anesth Analg 2008;107:729–731.
- Chin J, Tsui BC: No change in impedance upon intravascular injection of D5W. Can J Anaesth 2010;57:559–564.
- Collins AB, Gray AT, Kessler J: Ultrasound-guided supraclavicular brachial plexus nerve block: a modified Plumb-Bob technique. Reg Anesth Pain Med 2006;31:591–592.
- Cornish P: Supraclavicular nerve block—new perspectives. Reg Anesth Pain Med 2009;34:607–608.
- Cornish PB, Leaper CJ, Nelson G, Anstis F, McQuillan C, Stienstra R: Avoidance of phrenic nerve paresis during continuous supraclavicular regional anaesthesia. Anaesthesia 2007;62:354–358.
- Duggan E, Brull R, Lai J, Abbas S: Ultrasound-guided brachial plexus nerve block in a patient with multiple glomangiomatosis. Reg Anesth Pain Med 2008;33:70–73.
- Duggan E, El Beheiry H, Perlas A, et al: Minimum effective volume of local anesthetic for ultrasound-guided supraclavicular brachial plexus nerve block. Reg Anesth Pain Med 2009;34:215–218.
- Feigl GC, Dreu M: Important structures to be known for a safe ultrasound-guided supraclavicular plexus nerve block. Reg Anesth Pain Med 2010;35:317–18.
- Feigl GC, Pixner T: Combination of variations of the interscalene gap as a pitfall for ultrasound-guided brachial plexus nerve block. Reg Anesth Pain Med 2011;36:523–524.
- Fredrickson MJ, Kilfoyle DH: Neurological complication analysis of 1000 ultrasound guided peripheral nerve blocks for elective orthopaedic surgery: a prospective study. Anaesthesia 2009;64:836–844.
- Fredrickson MJ, Patel A, Young S, Chinchanwala S: Speed of onset of “corner pocket supraclavicular” and infraclavicular ultrasound guided brachial plexus nerve block: a randomised observer-blinded comparison. Anaesthesia 2009;64:738–744.
- Gupta PK, Pace NL, Hopkins PM: Effect of body mass index on the ED50 volume of bupivacaine 0.5% for supraclavicular brachial plexus nerve block. Br J Anaesth 2010;104:490–495.
- Hanumanthaiah D, Vaidiyanathan S, Garstka M, Szucs S, Iohom G:Ultrasound guided supraclavicular nerve block. Med Ultrason 2013;15:224–229.
- Heil JW, Ilfeld BM, Loland VJ, Mariano ER: Preliminary experience with a novel ultrasound-guided supraclavicular perineural catheter insertion technique for perioperative analgesia of the upper extremity. J Ultrasound Med 2010;29:1481–1485.
- Ihnatsenka B, Boezaart AP: Applied sonoanatomy of the posterior triangle of the neck. Int J Shoulder Surg 2010;4:63–74.
- Jeon DG, Kim SK, Kang BJ, Kwon MA, Song JG, Jeon SM: Comparison of ultrasound-guided supraclavicular nerve block according to the various volumes of local anesthetic. Korean J Anesthesiol 2013;64:494–499.
- Jeon DG, Kim WI. Cases series: ultrasound-guided supraclavicular nerve block in 105 patients. Korean J Anesthesiol 2010;58:267–271.
- Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C: Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg 1994;78:507–513.
- Kinjo S, Frankel A: Failure of supraclavicular nerve block under ultrasound guidance: clinical relevance of anatomical variation of cervical vessels. J Anesth 2012;26:100–102.
- Klaastad O, Sauter AR, Dodgson MS: Brachial plexus nerve block with or without ultrasound guidance. Curr Opin Anaesthesiol 2009;22:655–660.
- la Grange P, Foster PA, Pretorius LK: Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus nerve block. Br J Anaesth 1978;50:965–967.
- Lasserre A, Tran-Van D, Gaertner E, Labadie P, Fontaine B: Ultrasound guided locoregional anaesthesia: realization and diagnosis of complications [in French]. Ann Fr Anesth Reanim 2009;28:584–587.
- Macfarlane AJ, Perlas A, Chan V, Brull R: Eight ball, corner pocket ultrasoundguided supraclavicular nerve block: avoiding a scratch. Reg Anesth Pain Med 2008;33:502–503.
- Manickam BP, Oosthuysen SA, Parikh MK: Supraclavicular brachial plexus nerve block-variant relation of brachial plexus to subclavian artery on the first rib. Reg Anesth Pain Med 2009;34:383–384.
- Marhofer P, Schrogendorfer K, Koinig H, Kapral S, Weinstabl C, Mayer N: Ultrasonographic guidance improves sensory nerve block and onset time of three-in-one nerve blocks. Anesth Analg 1997;85:854–857.
- Morfey D, Brull R: Ultrasound-guided supraclavicular nerve block: What is intraneural? Anesthesiology 2010;112:250–251.
- Morfey DH, Brull R: Finding the corner pocket: landmarks in ultrasoundguided supraclavicular nerve block. Anaesthesia 2009;64:1381.
- Neal JM, Moore JM, Kopacz DJ, Liu SS, Kramer DJ, Plorde JJ: Quantitative analysis of respiratory, motor, and sensory function after supraclavicular nerve block. Anesth Analg 1998;86:1239–1244.
- Perlas A, Chan VW, Simons M: Brachial plexus examination and localization using ultrasound and electrical stimulation: a volunteer study. Anesthesiology 2003;99:429–435.
- Perlas A, Lobo G, Lo N, Brull R, Chan VW, Karkhanis R: Ultrasound-guided supraclavicular nerve block: outcome of 510 consecutive cases. Reg Anesth Pain Med 2009;34:171–176.
- Plunkett AR, Brown DS, Rogers JM, Buckenmaier CC III: Supraclavicular continuous peripheral nerve block in a wounded soldier: when ultrasound is the only option. Br J Anaesth 2006;97:715–717.
- Reiss W, Kurapati S, Shariat A, Hadzic A: Nerve injury complicating ultrasound/electrostimulation-guided supraclavicular brachial plexus nerve block. Reg Anesth Pain Med 2010;35:400–401.
- Renes SH, Spoormans HH, Gielen MJ, Rettig HC, van Geffen GJ: Hemidiaphragmatic paresis can be avoided in ultrasound-guided supraclavicular brachial plexus nerve block. Reg Anesth Pain Med 2009;34:595–599.
- Roy M, Nadeau MJ, Côté D, et al: Comparison of a single- or double-injection technique for ultrasound-guided supraclavicular nerve block: a prospective, randomized, blinded controlled study. Reg Anesth Pain Med 2012;37: 55–59.
- Samet R, Villamater E: Eight ball, corner pocket for ultrasound-guided supraclavicular nerve block: high risk for a scratch. Reg Anesth Pain Med 2008; 33:87.
- Shorthouse JR, Danbury CM: Ultrasound-guided supraclavicular brachial plexus nerve block in Klippel-Feil syndrome. Anaesthesia 2009;64: 693–694.
- Sivashanmugam T, Ray S, Ravishankar M, Jaya V, Selvam E, Karmakar MK: Randomized comparison of extrafascial versus subfascial injection of local anesthetic during ultrasound-guided supraclavicular brachial plexus nerve block. Reg Anesth Pain Med 2015;40:337–343.
- Soares LG, Brull R, Lai J, Chan VW: Eight ball, corner pocket: the optimal needle position for ultrasound-guided supraclavicular nerve block. Reg Anesth Pain Med 2007;32:94–95.
- Song JG, Jeon DG, Kang BJ, Park KK: Minimum effective volume of mepivacaine for ultrasound-guided supraclavicular nerve block. Korean J Anesthesiol 2013;65:37–41.
- Subramanyam R, Vaishnav V, Chan VW, Brown-Shreves D, Brull R: Lateral versus medial needle approach for ultrasound-guided supraclavicular nerve block: a randomized controlled trial. Reg Anesth Pain Med 2011;36: 387–392.
- Techasuk W, González AP, Bernucci F, Cupido T, Finlayson RJ, Tran DQ: A randomized comparison between double-injection and targeted intracluster-injection ultrasound-guided supraclavicular brachial plexus nerve block. Anesth Analg 2014;118:1363–1369.
- Tran DQ, Dugani S, Correa JA, Dyachenko A, Alsenosy N, Finlayson RJ: Minimum effective volume of lidocaine for ultrasound-guided supraclavicular nerve block. Reg Anesth Pain Med 2011;36:466–469.
- Tran DQ, Munoz L, Zaouter C, Russo G, Finlayson RJ: A prospective, randomized comparison between single- and double-injection, ultrasound-guided supraclavicular brachial plexus nerve block. Reg Anesth Pain Med 2009; 34:420–424.
- Tran DQ, Russo G, Munoz L, Zaouter C, Finlayson RJ: A prospective, randomized comparison between ultrasound-guided supraclavicular, infraclavicular, and axillary brachial plexus nerve blocks. Reg Anesth Pain Med 2009;34:366–371.
- Tsui BC, Doyle K, Chu K, Pillay J, Dillane D: Case series: ultrasound-guided supraclavicular nerve block using a curvilinear probe in 104 day-case hand surgery patients. Can J Anaesth 2009;56:46–51.
- Tsui BC, Twomey C, Finucane BT: Visualization of the brachial plexus in the supraclavicular region using a curved ultrasound probe with a sterile transparent dressing. Reg Anesth Pain Med 2006;31:182–184.
- VadeBoncouer TR, Weinberg GL, Oswald S, Angelov F: Early detection of intravascular injection during ultrasound-guided supraclavicular brachial plexus nerve block. Reg Anesth Pain Med 2008;33:278–279.
- Vermeylen K, Engelen S, Sermeus L, Soetens F, Van de Velde M: Supraclavicular brachial plexus nerve blocks: review and current practice. Acta Anaesthesiol Belg 2012;63:15–21.
- Vernieuwe L, Van de Putte P: Ultrasound-guided supraclavicular nerve block in a patient with no first rib. J Clin Anesth 2015;27:361–362.
- Watanabe T, Yanabashi K, Moriya K, Maki Y, Tsubokawa N, Baba H: Ultrasound-guided supraclavicular brachial plexus nerve block in a patient with a cervical rib. Can J Anaesth 2015;62:671–673.
- Williams SR, Chouinard P, Arcand G, et al: Ultrasound guidance speeds execution and improves the quality of supraclavicular nerve block. Anesth Analg 2003;97:1518–1523.
- Yazer MS, Finlayson RJ, Tran DQ: A randomized comparison between infraclavicular nerve block and targeted intracluster injection supraclavicular nerve block. Reg Anesth Pain Med 2015;40:11–15.