FACTS
- Indications: Foot, ankle and Achilles tendon surgery
- Transducer position: Transverse over the popliteal fossa
- Goal: Local anesthetic spread surrounding the sciatic nerve within the epineural sheath
- Local anesthetic: 15–20 mL
GENERAL CONSIDERATIONS
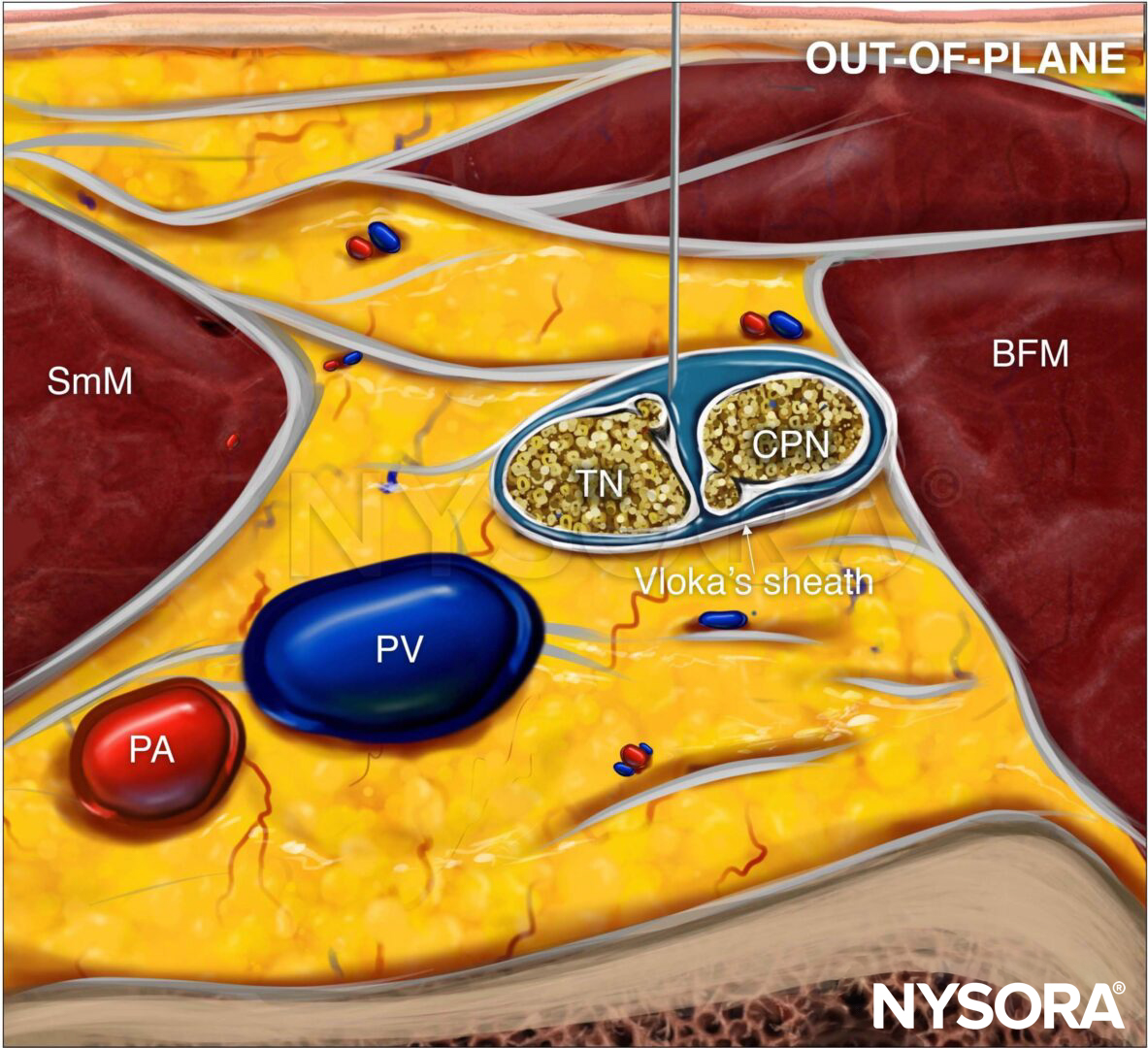
The anatomy of the sciatic nerve in the popliteal fossa is variable, and the division into the tibial nerve (TN) and common peroneal nerve (CPN) occurs at an inconstant distance from the popliteal crease (Figure 1). With nerve stimulator–based techniques, larger volumes (eg, > 40 mL) of local anesthetic have been used to increase the chance of nerve block success.
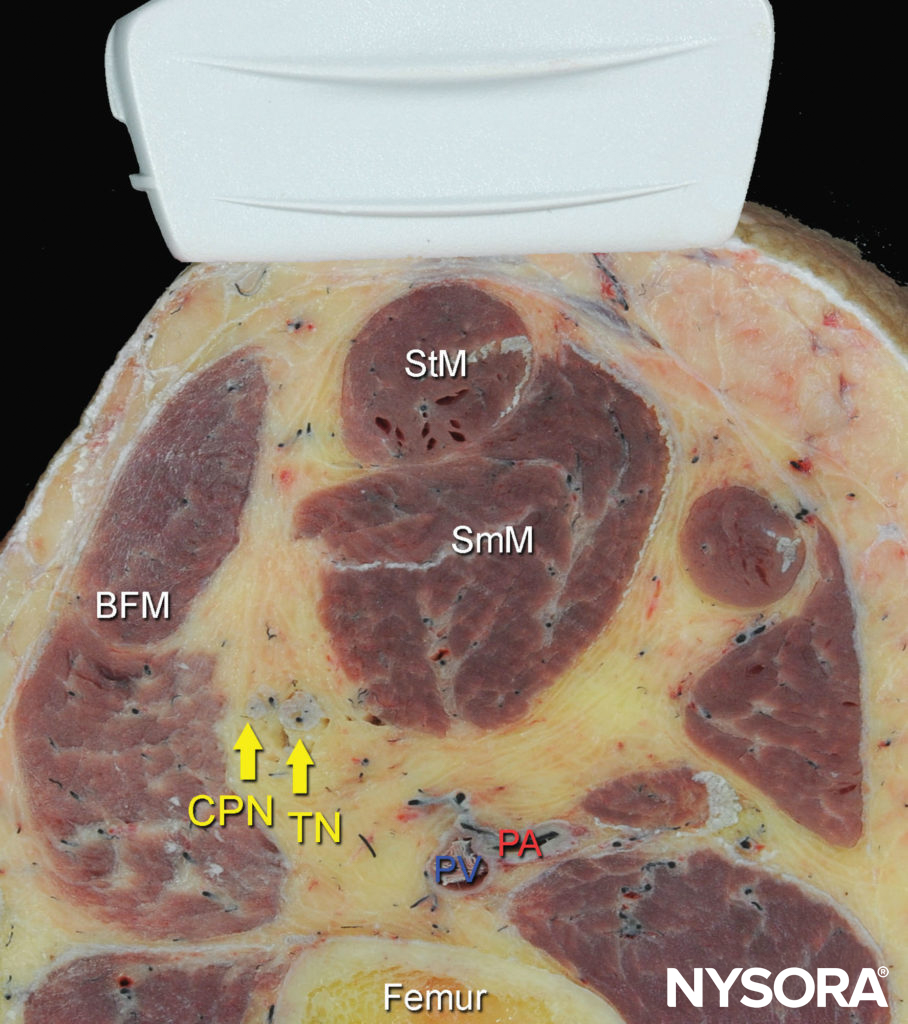
FIGURE 1. Cross-sectional anatomy of the sciatic nerve in the popliteal fossa. Shown are the common peroneal nerve (CPN), tibial nerve (TN), popliteal artery (PA), popliteal vein (PV), femur, biceps femoris muscle (BFM), semimembranosus muscle (SmM), and semitendinosus (StM) muscle. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
However, US guidance reduces the volume required for a reliable nerve block because the injection can be halted once adequate spread is observed. The most common approaches to the popliteal sciatic nerve block are the lateral approach, with the patient in the supine or lateral position, and the posterior approach in the prone or lateral position (Figure 2). While the patient position and needle path differ between the two approaches, the rest of the technique details are similar.
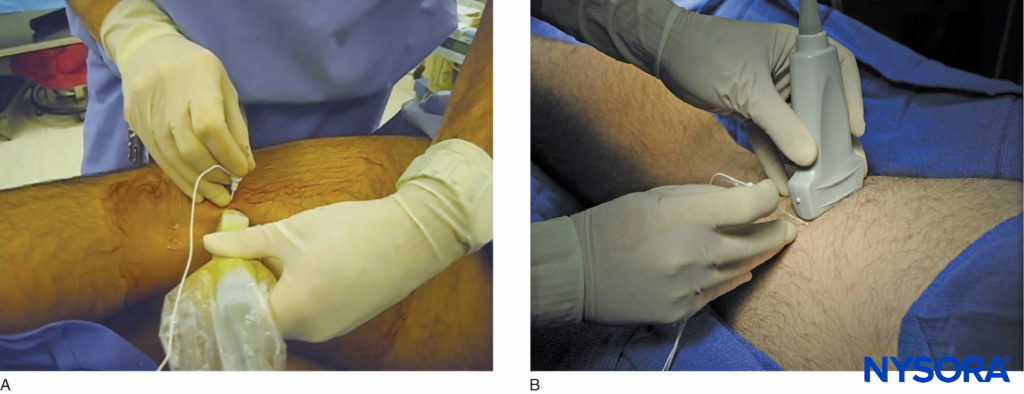
FIGURE 2. The posterior approach to the US-guided popliteal sciatic nerve block can be performed (A) with the patient in the lateral position, or (B) with the patient prone. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
The injection of local anesthetic must occur within the sciatic nerve sheath that contains both components of the nerve. The injection is ideally accomplished at the position where both components of the nerve are within the sheath but slightly separated by adipose tissue, allowing for safe placement of the needle between them. Although the sciatic nerve block can be accomplished with an injection around either nerve component, injecting into the space between both is more common in clinical practice.
ULTRASOUND ANATOMY
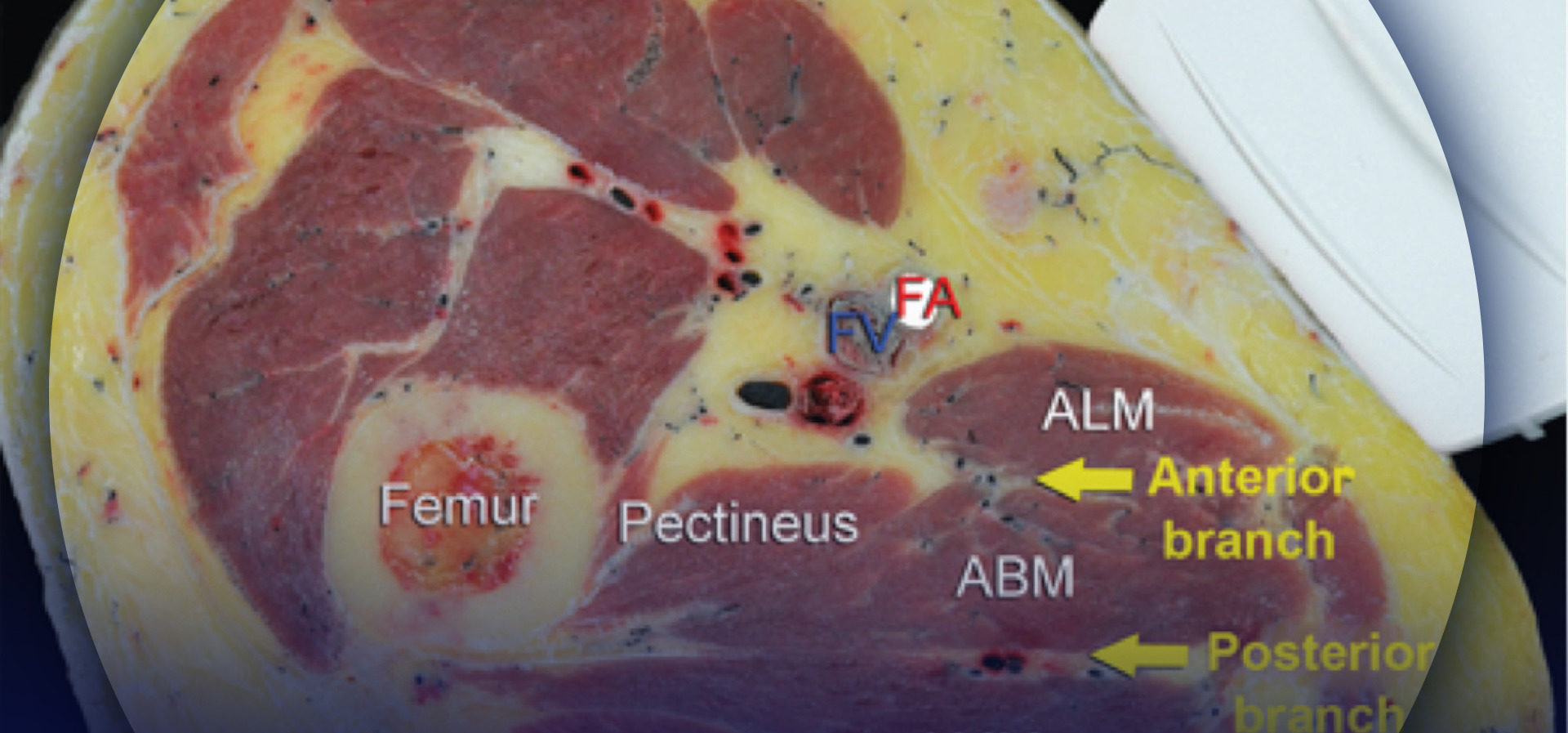
Beginning with the transducer in the transverse position at the popliteal crease, the popliteal artery is identified, aided with color Doppler US when necessary, at a depth of approximately 3–4 cm. The popliteal vein accompanies the artery at it is positioned just superficial (posterior) to it. On either side of the artery are the biceps femoris muscles (laterally) and the semimembranosus and semitendinosus muscles (medially). The tibial nerve is positioned superficial and lateral to the vein and is seen as a hyperechoic, oval or round structure with a honeycomb pattern (Figure 3). Asking the patient to dorsiflex and plantar flex the ankle makes the two sciatic nerve branches twist or move in relation to each other. Usually, tilting the transducer caudally is necessary to bring out the nerve from the neighboring adipose tissue.
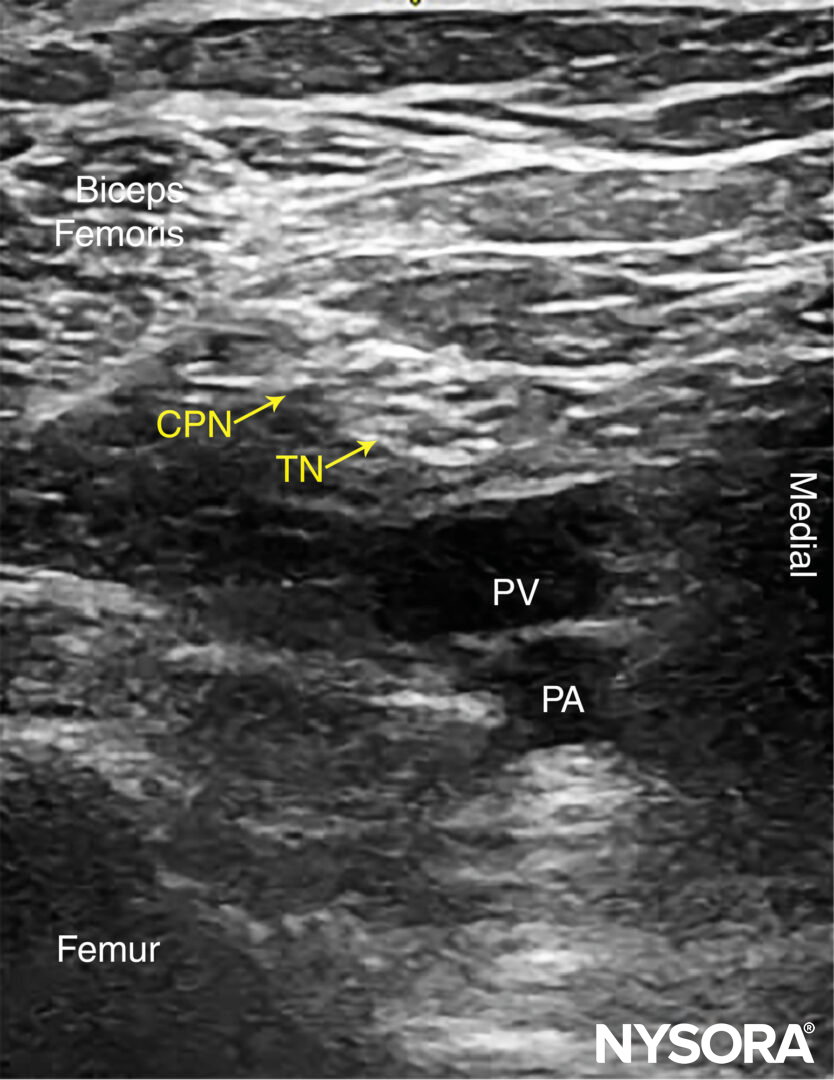
FIGURE 3. Sonoanatomy of the sciatic nerve at the popliteal fossa. The two main divisions of the sciatic nerve, the tibial nerve (TN) and the common peroneal nerve (CPN), are seen immediately lateral and superficial to the popliteal vein (PV) and artery (PA). This image was taken at 5 cm above the popliteal fossa crease, where the TN and CPN have just started diverging.
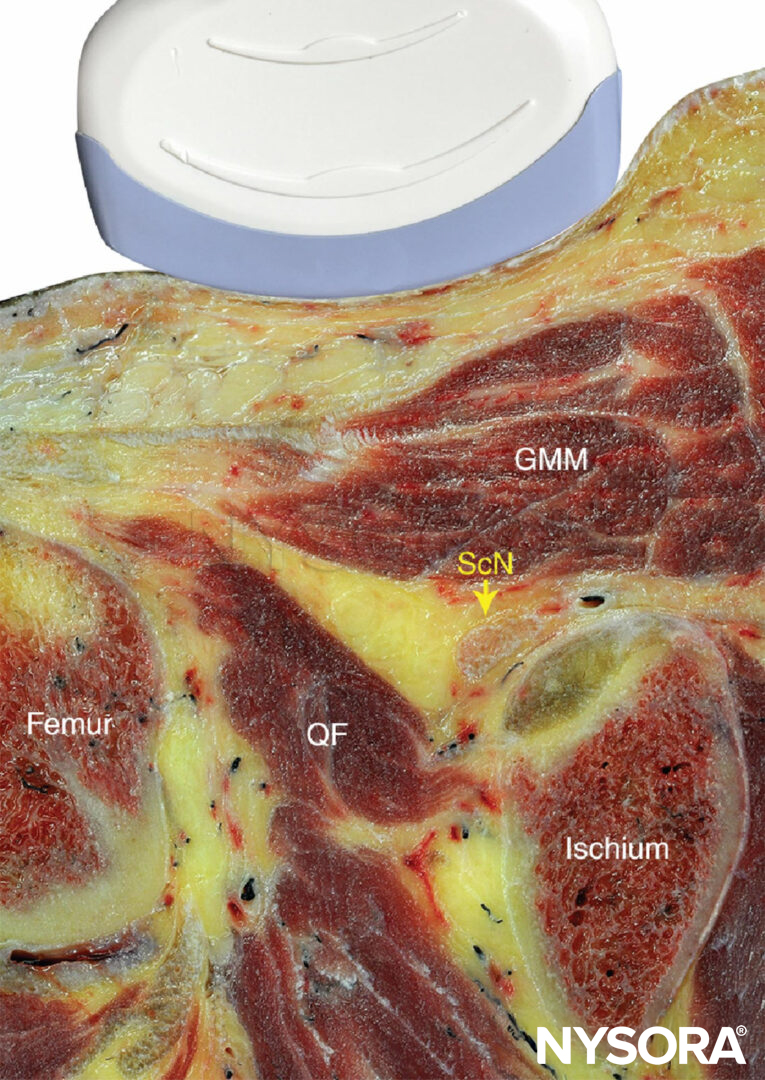
Once the tibial nerve has been identified, the CPN is visualized slightly more superficial and lateral to the tibial nerve. The transducer should be slid proximally until the tibial and peroneal nerves are visualized coming together to form the sciatic nerve before its division (Figure 4). This junction usually occurs at a distance 5–10 cm from the popliteal crease but may occur very close to the crease or, less commonly, more proximally in the thigh.
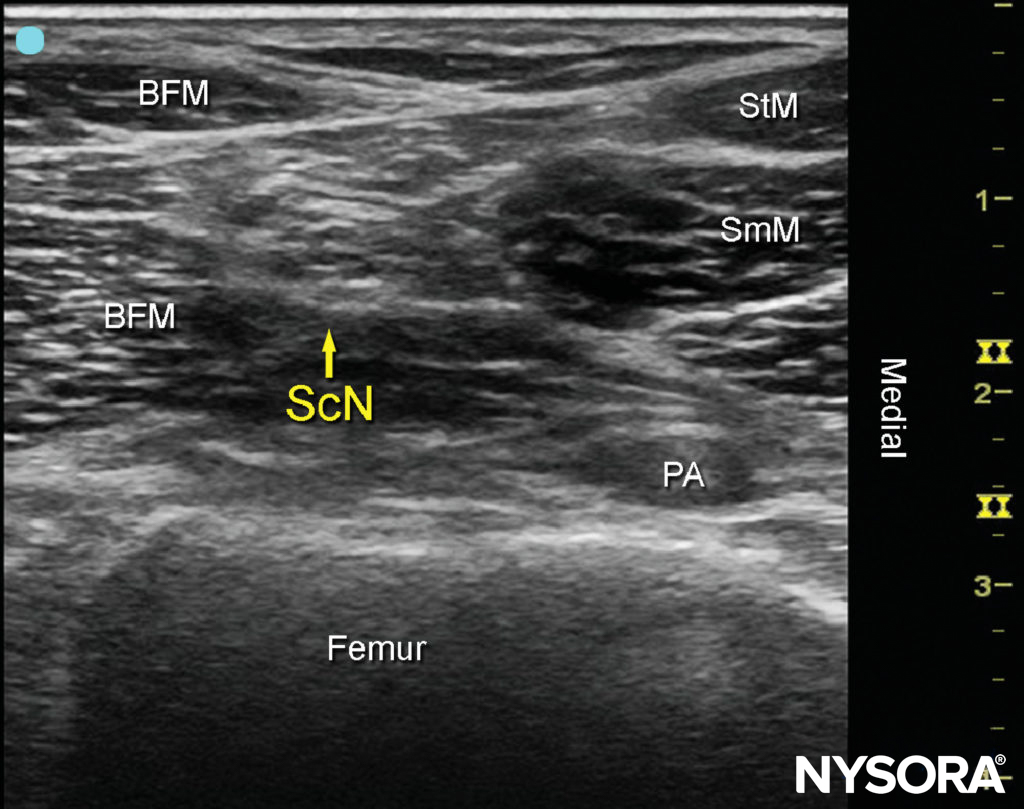
FIGURE 4 Sonoanatomy of the sciatic nerve (ScN) before its division. Shown are the ScN, superior and lateral to the popliteal artery (PA), positioned between the biceps femoris muscle (BFM) the semimembranosus muscle (SmM), and the semitendinosus muscle (StM).
As the transducer is moved proximally, the popliteal vessels move deeper and become more challenging to image. Adjustments in depth, gain, focus, and direction of the US beam should be made to keep the nerve visible at all times. At the popliteal fossa, the sciatic nerve typically is visualized at a depth of 2–4 cm.
NYSORA Tips
• Ultrasound imaging should specifically focus on identifying the sciatic nerve sheath (Vloka’s sheath) containing both components of the sciatic nerve (tibial and common peroneal nerves). Successful injection will deposit local anesthetic within the Vloka’s sheath
For a more comprehensive review of the sciatic nerve distribution, see Functional Regional Anesthesia Anatomy.
block DISTRIBUTION
Sciatic nerve block results in anesthesia of the lower limb below the knee, both motor and sensory, with the exception of the medial leg and foot, which is the territory of the saphenous nerve, a branch of the femoral nerve. The motor fibers to the hamstring muscles are spared; however, fibers to the posterior aspect of the knee joint are blocked (Figure 5).
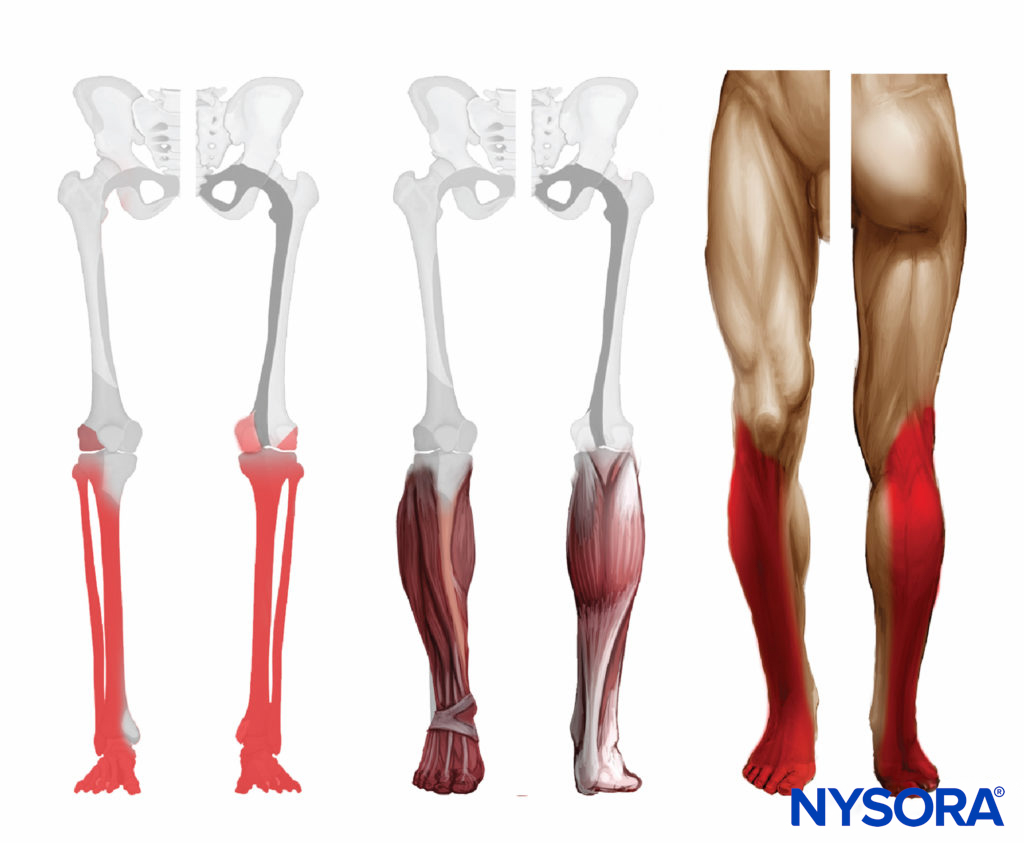
FIGURE 5. Expected distribution of the sciatic nerve sensory block at the level of the popliteal fossa.
EQUIPMENT
The equipment recommended for a popliteal sciatic nerve block includes the following:
- Ultrasound machine with a linear transducer (8–12 MHz), sterile sleeve, and gel
- Standard nerve block tray
- A 20-mL syringe containing local anesthetic
- 50- to 100-mm, 21- to 22-gauge, short-bevel, insulated stimulating needle
- Peripheral nerve stimulator
- Injection pressure monitor
- Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING: LATERAL APPROACH
This nerve block is performed with the patient in the supine or lateral position. This can be accomplished either by resting the foot on an elevated footrest or flexing the knee while an assistant stabilizes the foot and ankle on the bed (Figure 6). If nerve stimulation is used, exposure of the calf and foot is required to observe motor responses.

FIGURE 6. Needle insertion technique to nerve block the sciatic nerve in the popliteal fossa using the lateral approach with the patient in the supine position. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
LANDMARKS AND PATIENT POSITIONING: POSTERIOR APPROACH
This nerve block is performed with the patient in the prone or lateral position (Figure 2). A small footrest is useful to facilitate identification of a motor response if nerve stimulation is used. A footrest also relaxes the hamstring tendons, making transducer placement and manipulation easier.
GOAL
The goal is to inject the local anesthetic within the common connective tissue (Vloka’s) sheath that envelops the TN and CPN. Alternatively, separate nerve blocks of TN and CPN can be performed.
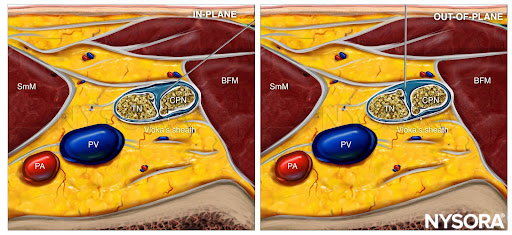
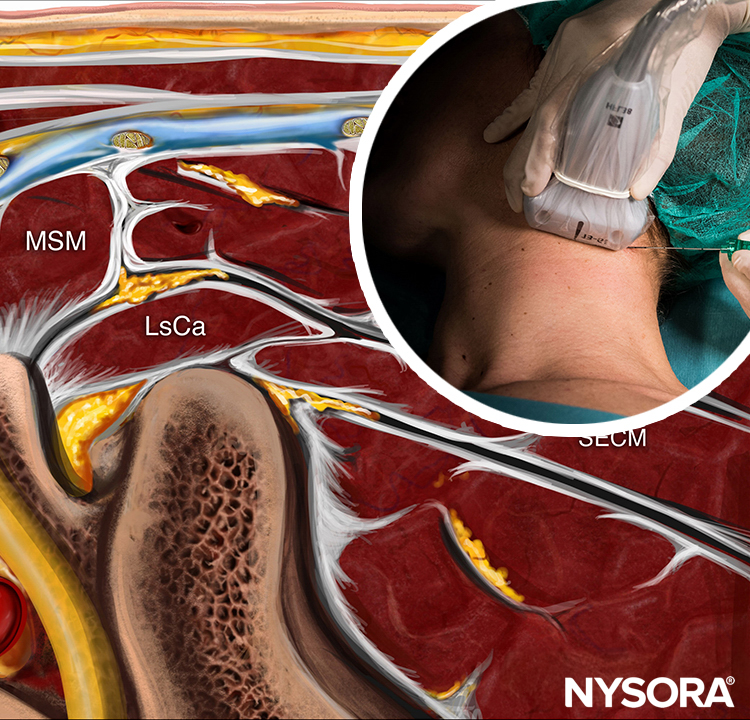
From the Regional Anesthesia Manual: Reverse Ultrasound Anatomy for a popliteal sciatic nerve block with needle insertion in-plane and out-of-plane and local anesthetic spread (blue). TN, tibial nerve; CPN, common peroneal nerve; PV, popliteal vein; PA, popliteal artery; SmM, semimembranosus muscle; BFM, biceps femoris muscle.
TECHNIQUE
The skin is disinfected and the transducer positioned to identify the sciatic nerve. If the nerve is not immediately apparent, tilting the transducer toward the feet can help improve the contrast and bring the nerve “out of the background”. Sliding the transducer slightly proximal or distal may improve the quality of the image and allow for better visualization.
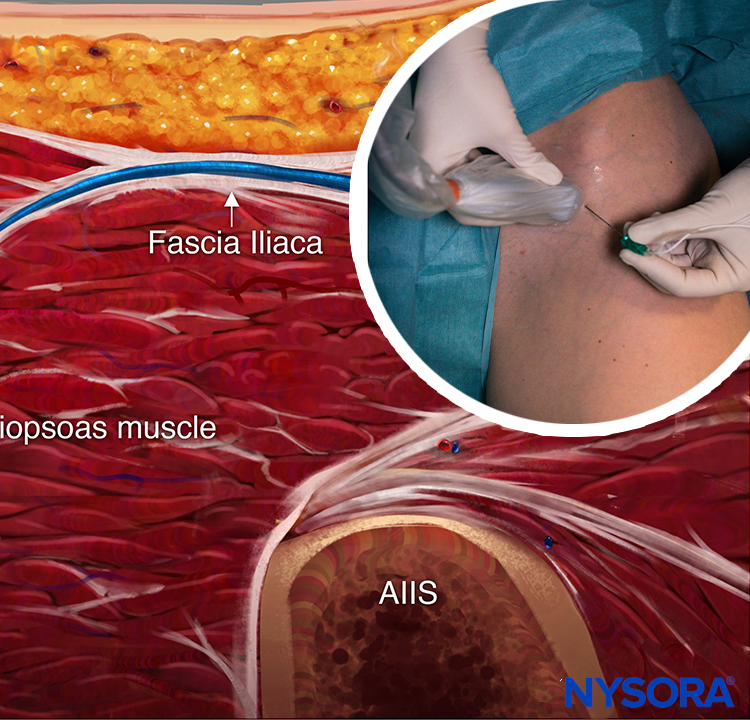
It is recommended to perform the nerve block at the level where TN and CPN start diverging but are still in the common sciatic nerve (Vloka’s) sheath. For the lateral approach, a skin wheal is made on the lateral aspect of the thigh 2–3 cm above the lateral edge of the transducer, and the needle is inserted in plane in a horizontal orientation from the lateral aspect of the thigh and advanced toward the sciatic nerve (Figures 7 and 8).
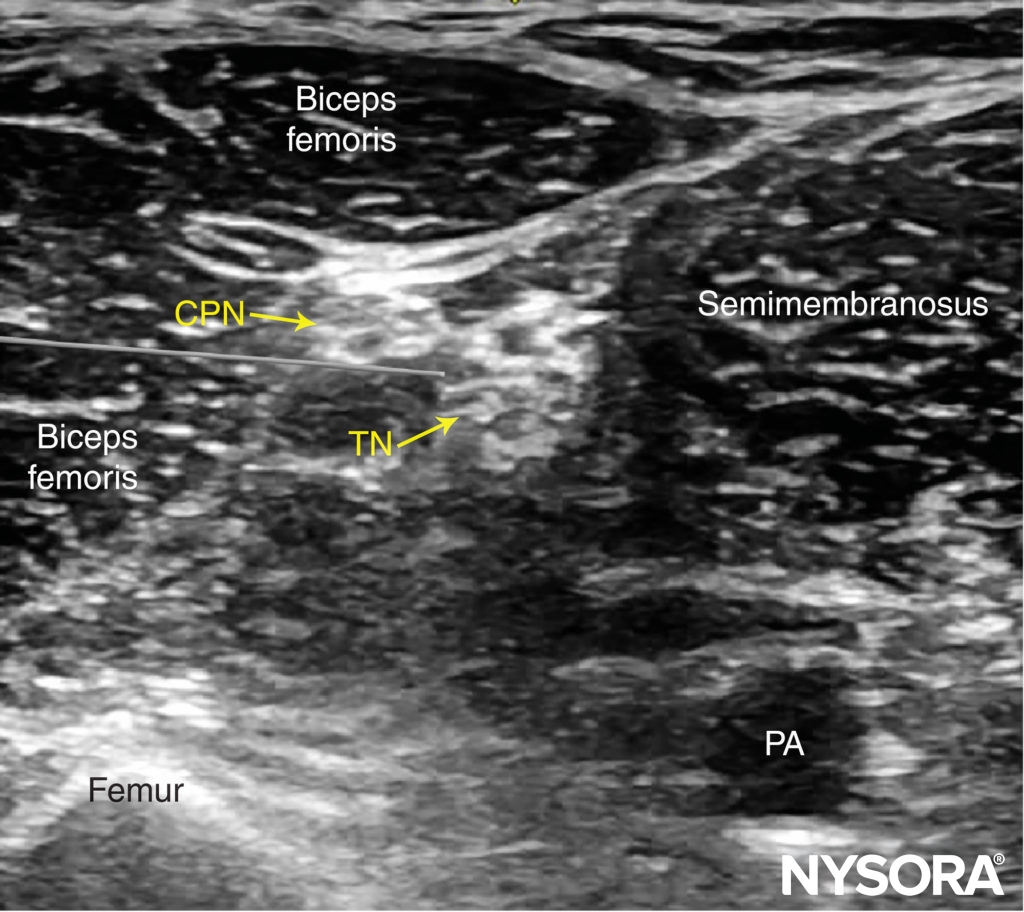
FIGURE 7. Simulated needle path and needle tip placement to nerve block the sciatic nerve (TN and CPN) using the lateral approach. PA, popliteal artery.
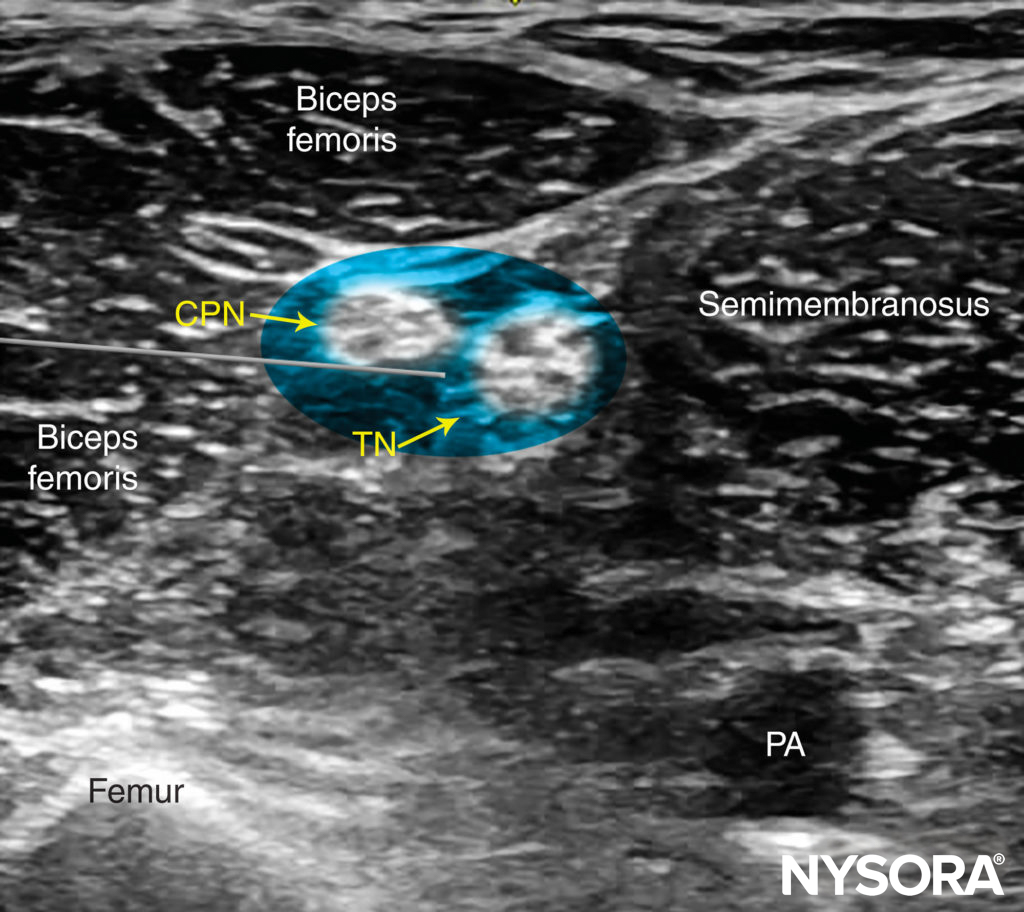
FIGURE 8. Simulated needle path and local anesthetic distribution to nerve block the sciatic nerve (TN and CPN) in the popliteal fossa using the lateral approach. PA, popliteal artery.
For the posterior approach, the needle is inserted in plane from lateral to medial (Figure 9) or out of plane (Figure 10). If nerve stimulation is used (0.5 mA, 0.1 msec), the contact of the needle tip with either branch of the nerve usually is associated with a motor response of the calf or foot. Once the needle tip is placed within the common sciatic nerve sheath, 1–2 mL of local anesthetic is injected to confirm the proper injection site. Such injection should result in a distribution of local anesthetic within the sheath, and separation of the TN and CPN within Vloka’s sheath (Figure 11).
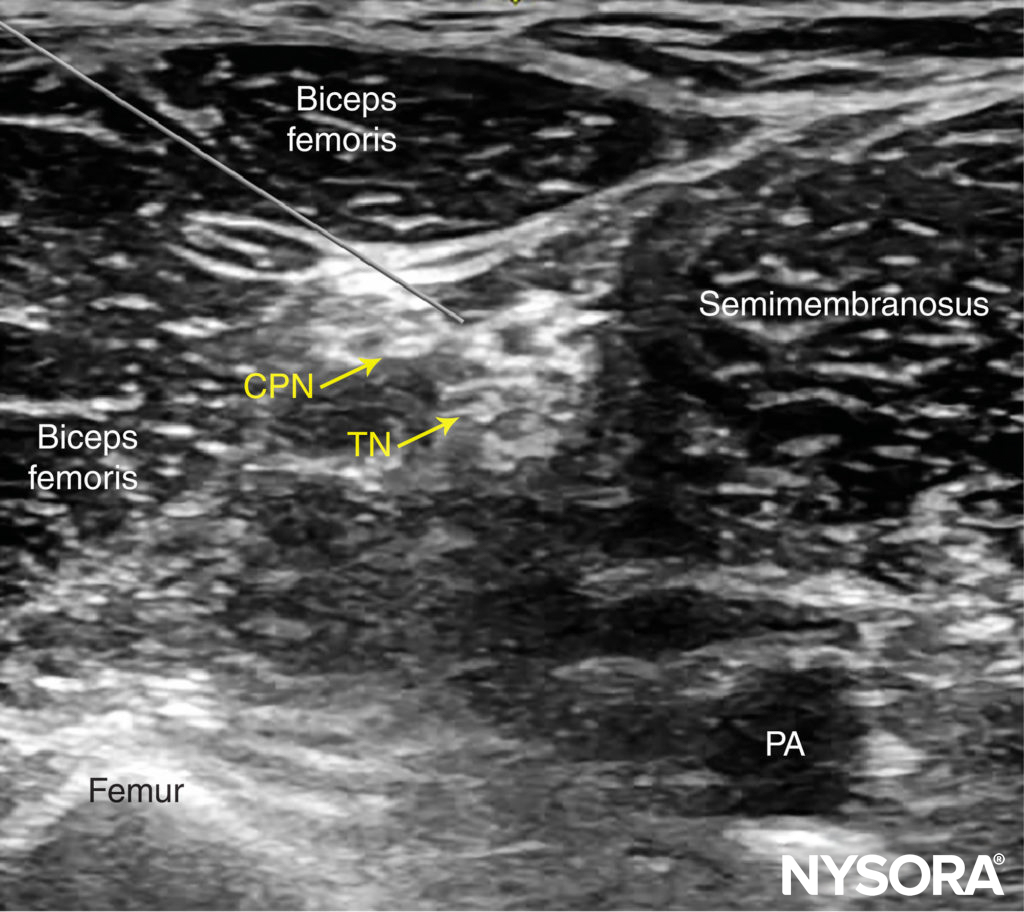
FIGURE 9. Simulated needle path and needle tip placement to nerve block the sciatic nerve (TN and CPN) through the posterior approach, in plane from lateral to medial. PA, popliteal artery.
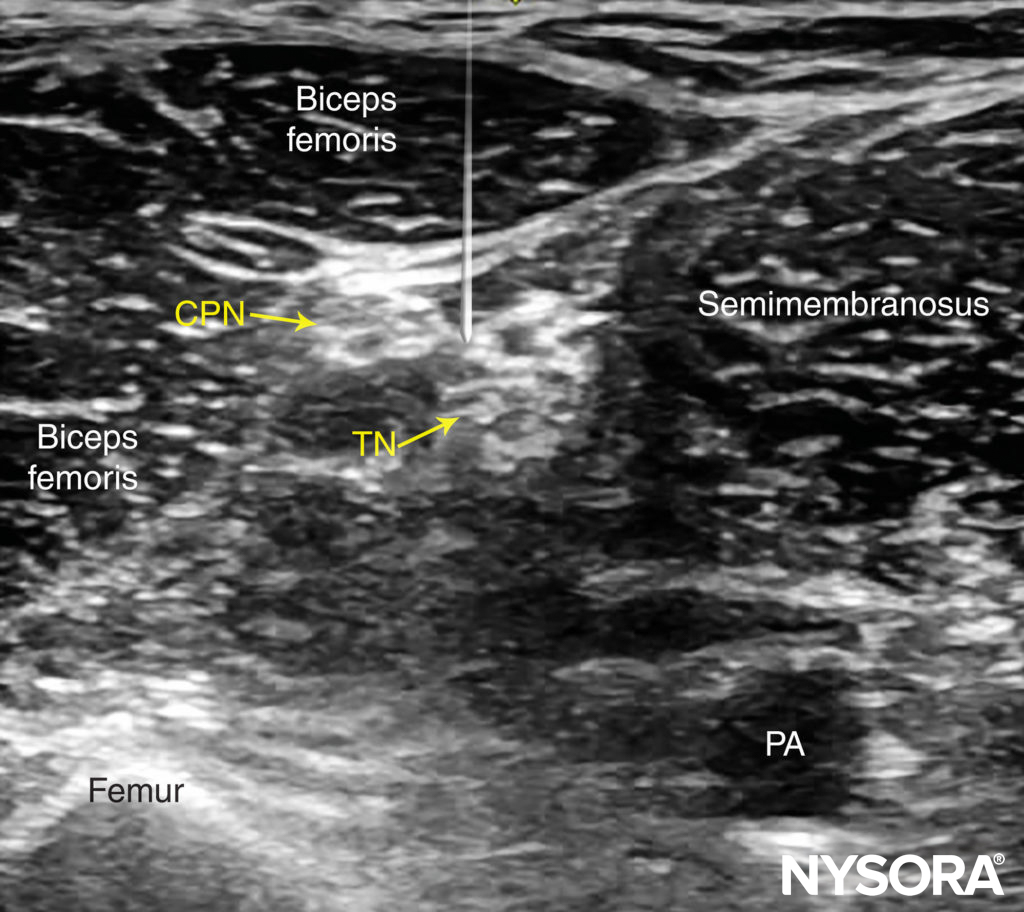
FIGURE 10. Simulated needle path and proper needle tip placement to nerve block the sciatic nerve (TN and CPN) through the posterior approach out of plane. PA, popliteal artery.
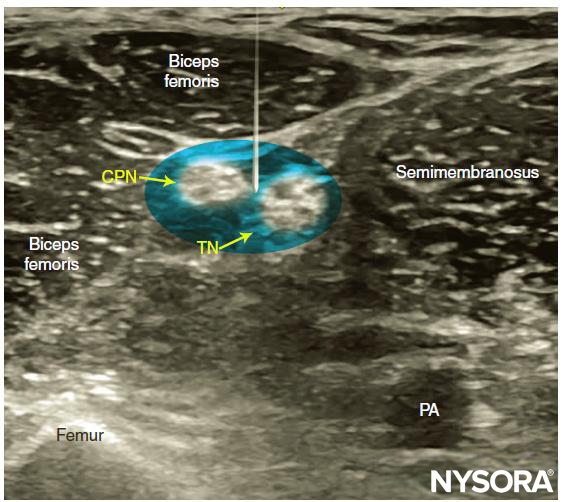
FIGURE 11. Simulated needle path, needle tip position and local anesthetic spread (blue-shaded area) to nerve block the sciatic nerve (TN and CPN) through the posterior approach out of plane. PA, popliteal artery.
When local anesthetic injection does not appear to result in a spread inside the sciatic nerve sheath and around the sciatic nerve components, additional needle repositions and injections may be necessary. Correct injection is recognized when local anesthetic spreads proximally and distally to the site of the injection around both divisions of the nerve, which can be documented by observing the spread of the local anesthetic within Vloka’s sheath proximal to the site of injection. A single injection of local anesthetic typically suffices.
Supplementary video related to this nerve block can be found at Ultrasound-Guided Popliteal Sciatic Nerve Block Video
TIPS
- To improve needle visualization, a skin puncture site 2–3 cm lateral to the transducer will reduce the angle between the needle and the footprint of the transducer (see Figure 6).
- The presence of a motor response to nerve stimulation is useful but not necessary if the nerve, needle, and local anesthetic spread are well visualized.
- Never inject against high resistance because this may signal an intraneural injection (injection pressure must be < 15 psi).
- In the posterior approach to the popliteal nerve block, either an in-plane (lateral or medial) or out-of-plane technique can be used (Figures 9 through 12). While the in-plane lateral approach is commonly used, the advantage of the out-of-plane approach is that the needle path is through the skin and adipose tissue rather than the muscles and thus, less painful.
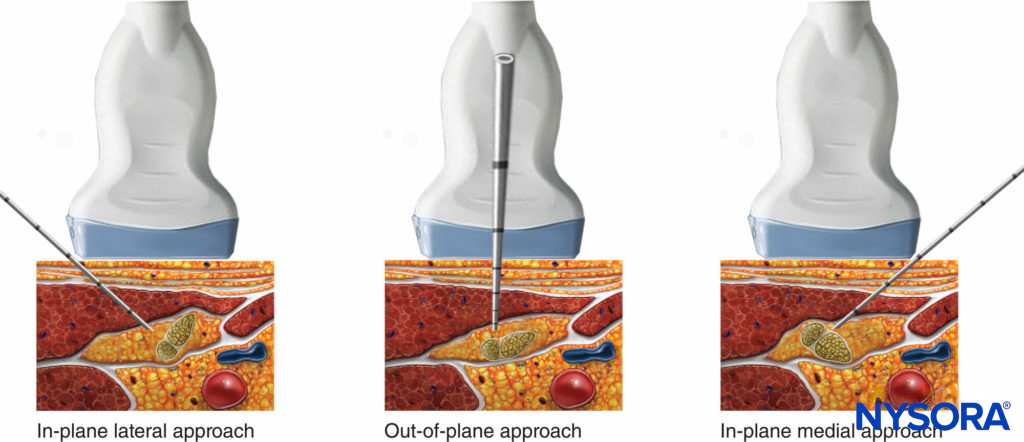
FIGURE 12. In-plane (lateral or medial) or out-of-plane approach are shown – the operator should be able to pick and choose any of these needle orientations, depending on the configuration of tibial and common peroneal branches at the site of injection.

FIGURE 13. Continuous sciatic nerve block in the popliteal fossa using a lateral approach with the patient in the supine position. The needle is positioned within the epineural sheath of the sciatic nerve. After an injection of a small volume of local anesthetic to confirm correct needle position, a catheter is inserted 2–4 cm past the needle tip. Preloading the catheter is useful in facilitating the procedure. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
CONTINUOUS ULTRASOUND-GUIDED POPLITEAL SCIATIC NERVE BLOCK
The goal of the continuous popliteal sciatic nerve block is to place the catheter within the sciatic nerve sheath in the popliteal fossa (Figure 13). The catheter is inserted 4-5 cm beyond needle tip and its correct placement is documented by observing injection of LA within the sciatic nerve sheath. The catheter is secured either by taping it to the skin or tunneling.
The lateral approach may have some advantage over the prone approach with regard to catheter placement. First, the biceps femoris muscle tends to stabilize the catheter and decrease the chance of dislodgement, compared with the subcutaneous tissue of the popliteal fossa in the prone approach. Second, if the knee is to be flexed and extended, the side of the thigh is less mobile than the back of the knee. Finally, access to the catheter site is more convenient with the lateral approach compared with the prone approach. A common starting infusion regimen is ropivacaine 0.2% at 5 mL/h with a patient-administered bolus of 5 mL every 60 minutes.
Follow the link to Continuous Peripheral Nerve Blocks for additional information.
Clinical updates
Schwartz et al. (Journal of Clinical Anesthesia, 2024) report that a single-shot liposomal bupivacaine 133 mg popliteal sciatic nerve block for bunionectomy significantly reduced cumulative pain scores and opioid consumption over 96 h compared with bupivacaine HCl, with a ~44% reduction in pain AUC and ~61% lower opioid use. Patients receiving liposomal bupivacaine were about five times more likely to remain opioid-free through postoperative day 4, while adverse events and motor recovery were similar between groups. These findings support liposomal bupivacaine as a catheter-sparing option to extend analgesia beyond 24 h for outpatient foot surgery.
- Read more about the study HERE.
Maagaard et al. (Anesthesiology, 2024) conducted a randomized, blinded trial in 120 patients undergoing foot or ankle surgery with popliteal sciatic + saphenous blocks and found that IV dexamethasone (12 mg) significantly prolonged block analgesia versus placebo (~56% increase), but adding IV dexmedetomidine (1 µg/kg) provided no additional prolongation. Both dexamethasone regimens reduced pain scores and opioid consumption only in the first 24 h and increased motor block duration, with no sustained benefit at 48–72 h and no clear safety advantage of the combination. These results suggest IV dexamethasone alone is sufficient as an adjunct for lower-extremity peripheral nerve blocks in this setting.
- Read more about the study HERE.
Olofsson et al. (European Journal of Anaesthesiology, 2024) report that, in patients undergoing forefoot surgery with multimodal analgesia, an ankle block did not provide longer analgesia than a popliteal sciatic nerve block. Although a greater proportion of patients in the sciatic block group remained opioid-free (80% vs 58%), pain scores and opioid consumption were similar, while the sciatic block produced a longer sensory block and impaired ambulation. These findings suggest block choice should prioritize functional considerations rather than the expected duration of analgesia.
- Read more about the study HERE.