FACTS
- Indications: arm, elbow, forearm, and hand surgery (Figure 1)
- Transducer position: approximately parasagittal, just medial to the coracoid process, inferior to the clavicle
- Goal: local anesthetic spread around axillary artery
- Local anesthetic volume: 20–30 mL
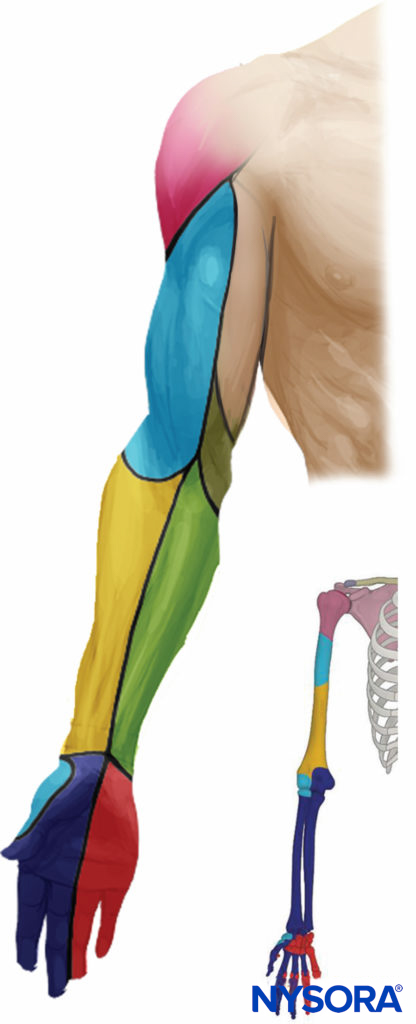
FIGURE 1. Distribution of sensory block of the infraclavicular brachial plexus nerve block.
GENERAL CONSIDERATIONS
The ultrasound (US)-guided infraclavicular brachial plexus nerve block is in some ways both simple and challenging. It is simple in that identification of the arterial pulse on the sonographic image is an easy primary goal in establishing the landmark. However, the plexus at this level is situated deeper, and the angle of approach is more acute, making simultaneous visualization of the needle and the relevant anatomy more challenging. Fortunately, although it is not always possible to reliably identify the three cords of the plexus, an adequate nerve block can be achieved by simply depositing the local anesthetic in a U shape around the artery. The infraclavicular brachial plexus nerve block is well suited for the catheter technique because the musculature of the chest wall helps stabilize the catheter and prevents its dislodgement compared with the more superficial location used with the interscalene and supraclavicular approaches to brachial plexus block.
ULTRASOUND ANATOMY
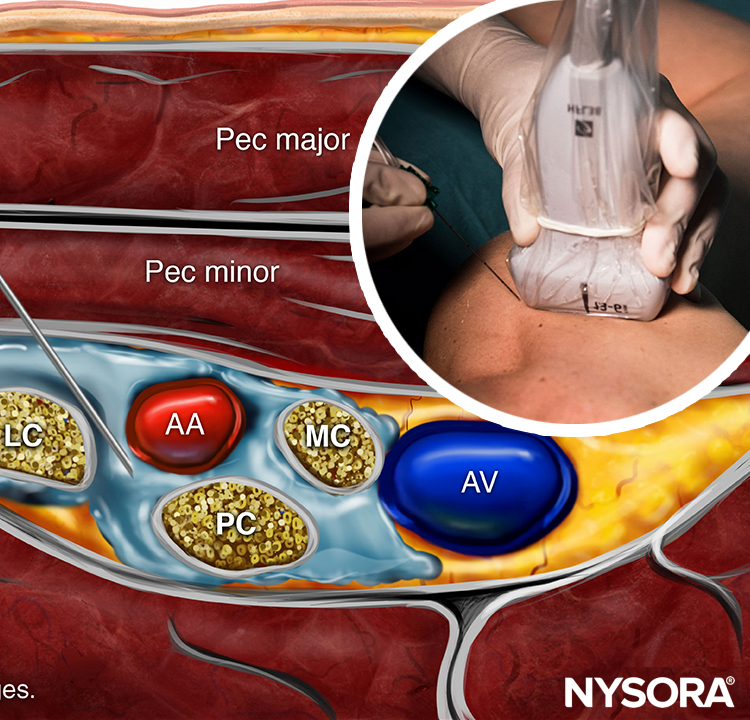
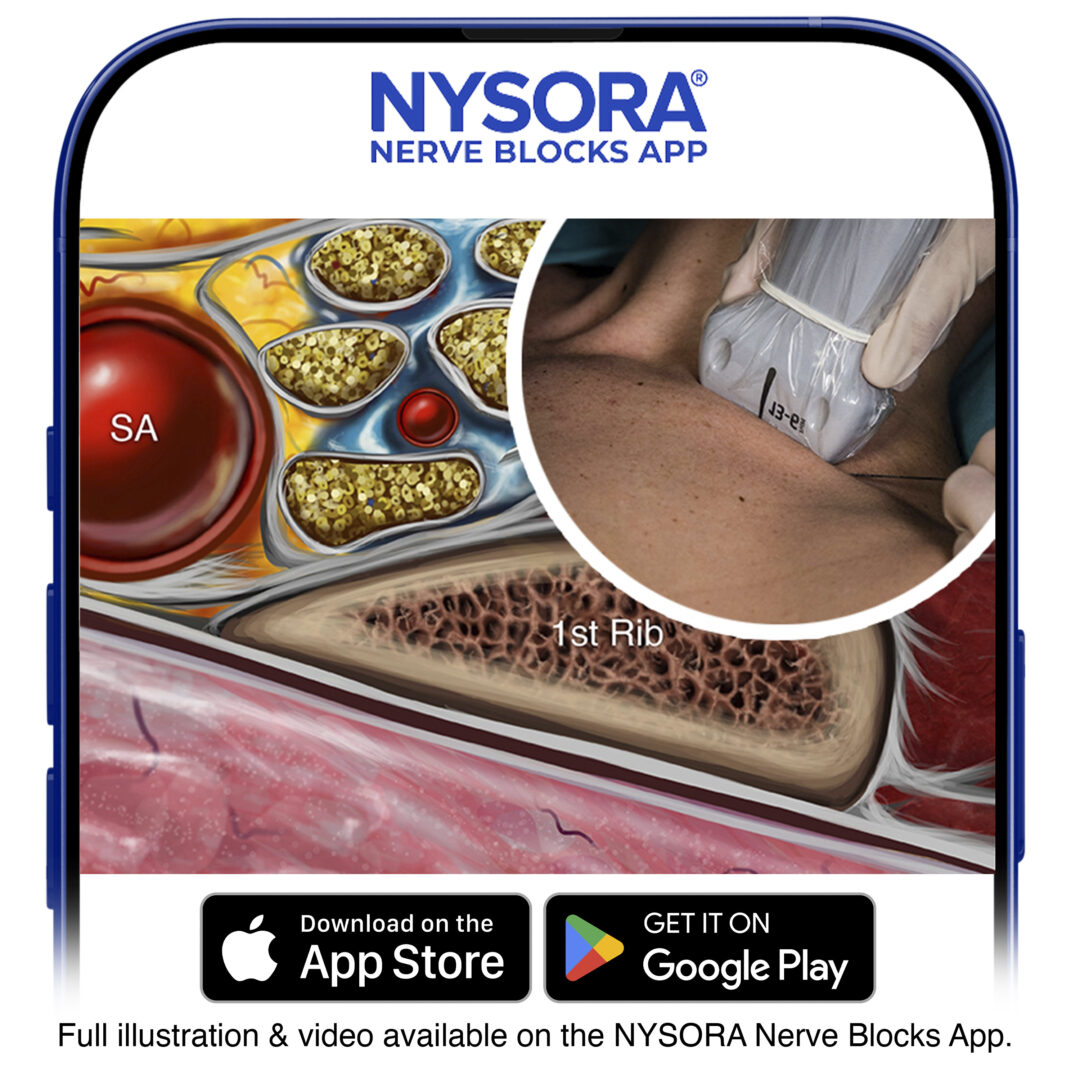
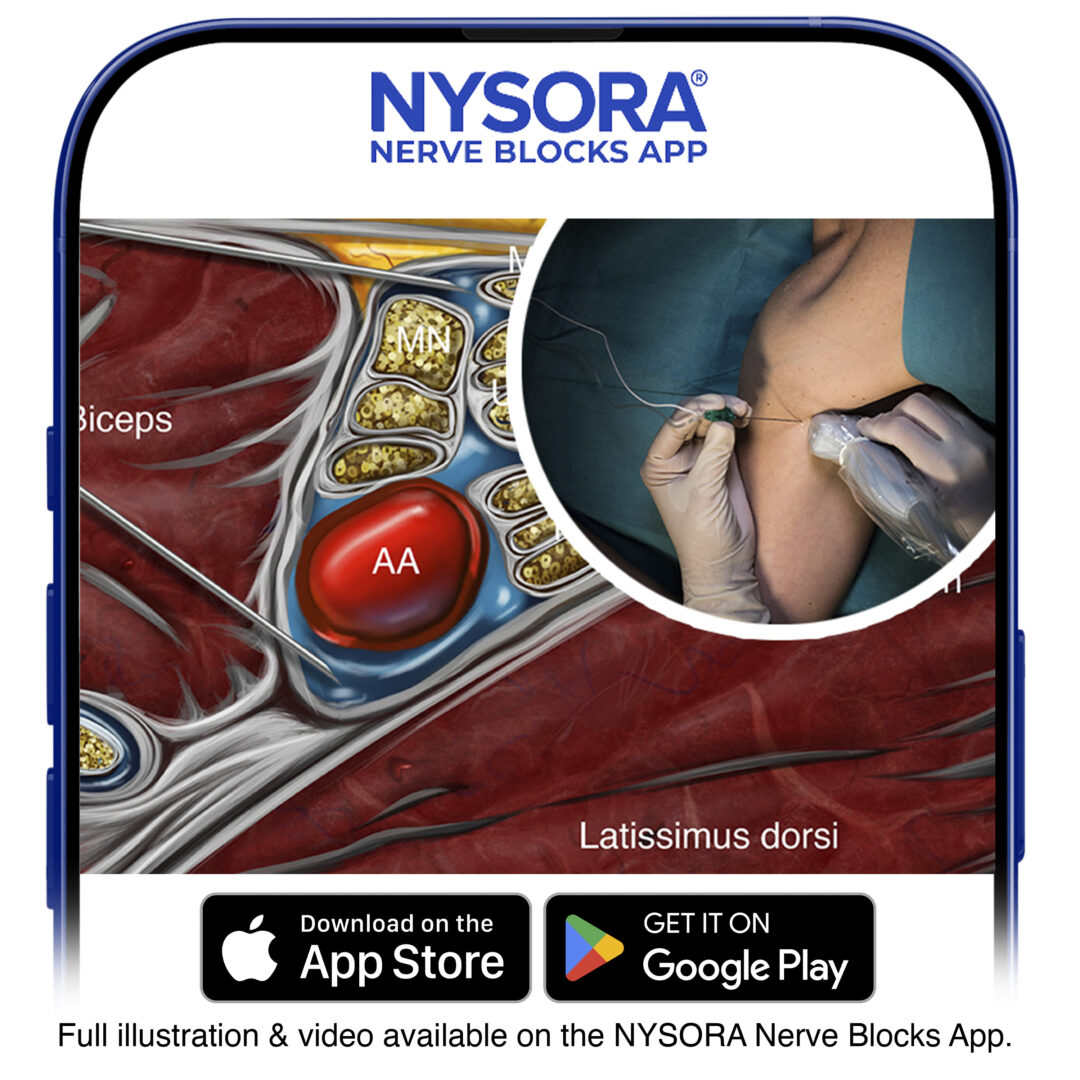
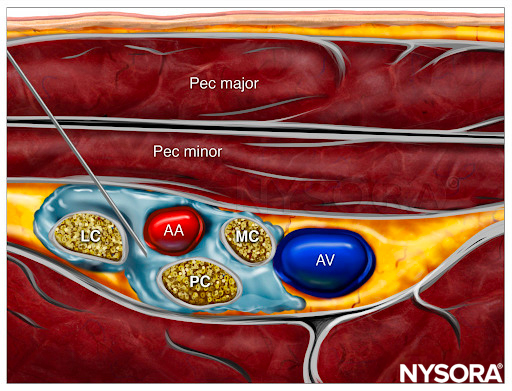
The axillary artery can be identified deep to the pectoralis major and minor muscles. An effort needs to be made to obtain clear views of both pectoralis muscles and their respective fasciae. This is important because the area of interest lies underneath the fascia of the pectoralis minor muscle. Surrounding the artery are the three cords of the brachial plexus: the lateral, posterior, and medial cords. These are named for their usual position relative to the axillary artery, although there is a great deal of anatomical variation. With the left side of the screen corresponding to the cephalad aspect, the cords can often be seen as round hyperechoic structures at the positions of approximately 9 o’clock (lateral cord), 7 o’clock (posterior cord), and 5 o’clock (medial cord) (Figures 2 and 3). The axillary vein is seen as a compressible hypoechoic structure that lies medially to the axillary artery. Multiple other, smaller vessels (eg, the cephalic vein) are often present as well. The transducer is moved in the cephalad-caudad and medial-lateral direction until the artery is identified in cross-section. Depending on the depth selected and the level at which the scanning is performed, the chest wall and the pleura may be seen in the medial and more caudal aspect of the image. The axillary artery and/or brachial plexus are typically identified at a depth of 3–5 cm in average-size patients.
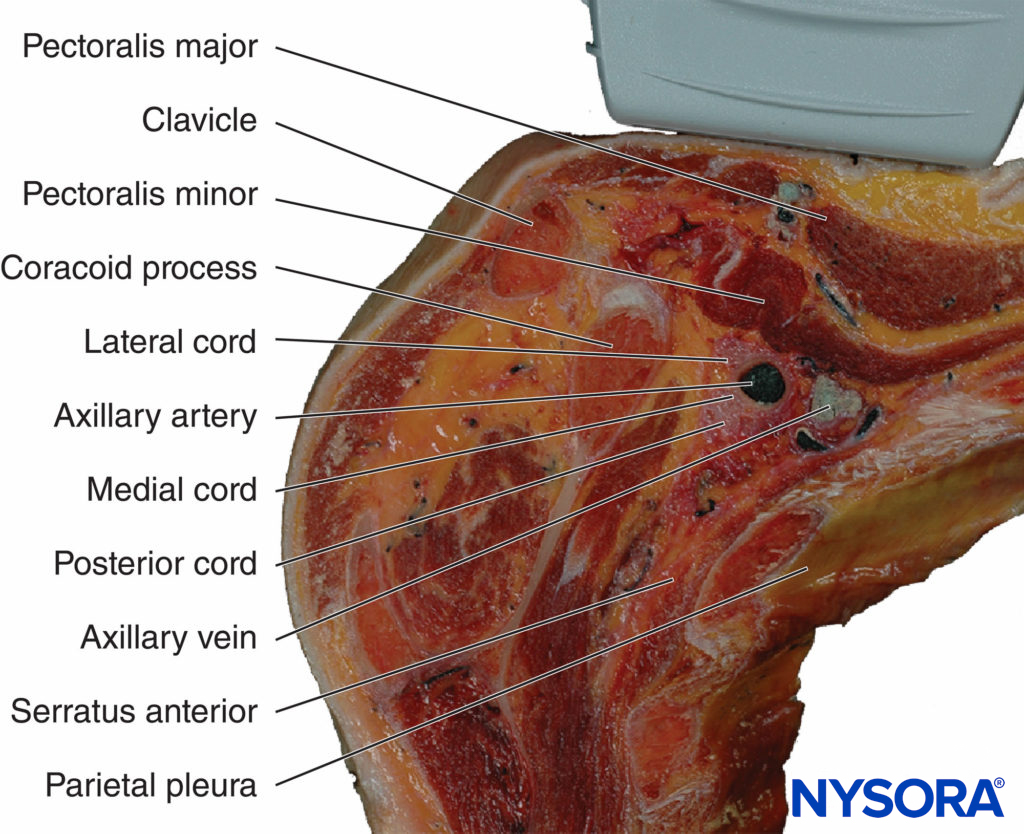
FIGURE 2. Anatomy of the infraclavicular brachial plexus (BP) and the position of the transducer. Paramedian sagittal plane at the level of the coracoid process. The BP is seen surrounding the axillary artery (AA) underneath the coracoid process and pectoralis minor muscle (PMiM). Note that the injection of local anesthetic should take place below the fascia of the PMiM to spread around the AA.
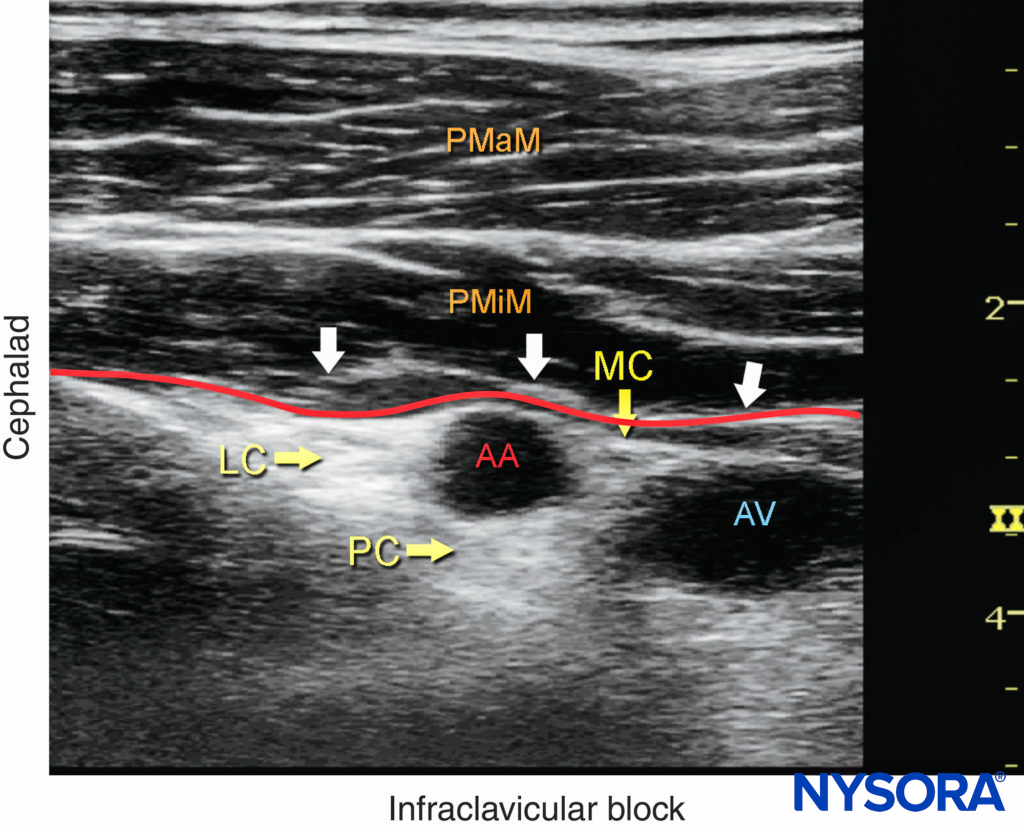
FIGURE 3. Ultrasound image of the brachial plexus (BP) distal to the clavicle. Note that the BP, axillary artery (AA) and axillary vein (AV) are located below the fascia (red line) of the pectoralis minor muscle (PMiM). LC, lateral cord; MC, medial cord; PC, posterior cord; PMaM, pectoralis major muscle.
DISTRIBUTION OF ANESTHESIA
The infraclavicular approach to brachial plexus block results in anesthesia of the upper limb below the shoulder. If required, the skin of the medial aspect of the upper arm (intercostobrachial nerve, T2) can be blocked by an additional subcutaneous injection on the medial aspect of the arm just distal to the axilla. A simpler approach is for surgeons to infiltrate the skin with the local anesthetic directly over the incision line as needed.
EQUIPMENT
The equipment recommended for an infraclavicular brachial plexus nerve block includes the following:
- Ultrasound machine with linear transducer (8–14 MHz), sterile sleeve, and gel
- Standard nerve block tray
- 20–30 mL of local anesthetic drawn up in syringes
- 8- to 10-cm, 21- to 22-gauge, short-bevel, insulated stimulating needle
- Peripheral nerve stimulator
- Opening injection pressure monitoring system
- Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
Any position that allows for the comfortable placement of the ultrasound transducer and needle advancement is appropriate. The nerve block is typically performed with the patient in the supine position with the head turned away from the side to be blocked (Figure 4). The arm is abducted to 90 degrees and the elbow flexed. This maneuver raises the clavicle, reduces the depth from the skin to the plexus, and substantially facilitates visualization of the pectoralis muscles as well as the cords of the brachial plexus and the needle. The coracoid process is an important landmark and can be easily identified by palpating the bony prominence just medial to the shoulder while the arm is elevated and lowered. As the arm is lowered, the coracoid process meets the fingers of the palpating hand. Scanning usually begins just medial to the coracoid process and inferior to the clavicle. Keeping the probe in a parasagittal plane, scanning medially and laterally allows the chest wall and pleura to be located (Figure 5). The nerve block should be performed with the probe lateral to the pleura in order to minimize the risk of pneumothorax.
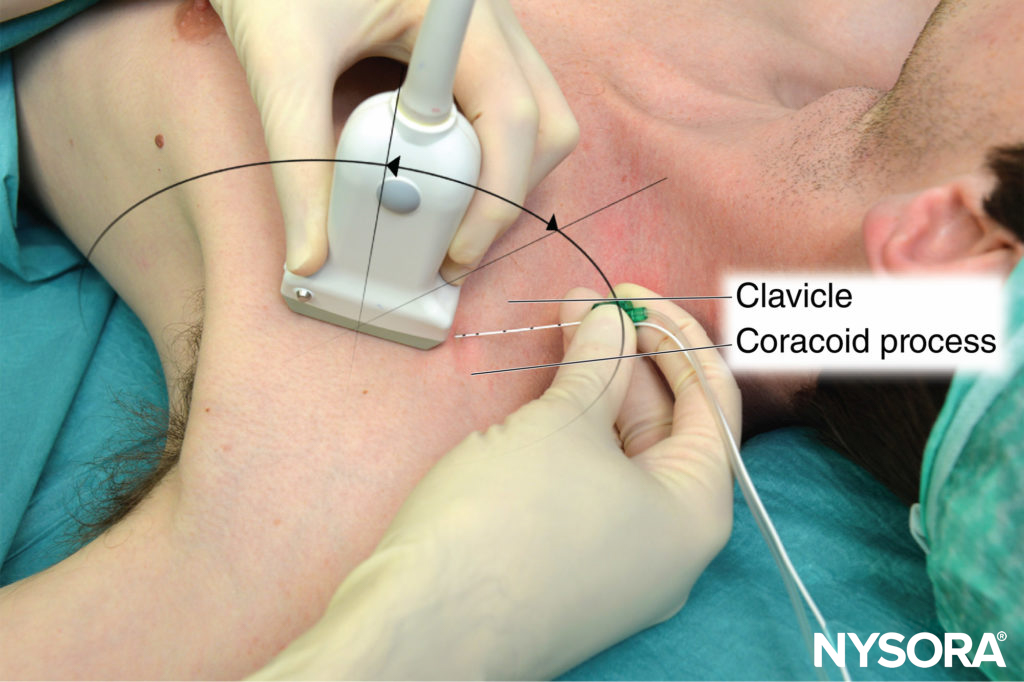
FIGURE 4. Patient position for infraclavicular brachial plexus nerve block needle insertion. The transducer is positioned parasagittally just medial to the coracoid process and inferior to the clavicle.
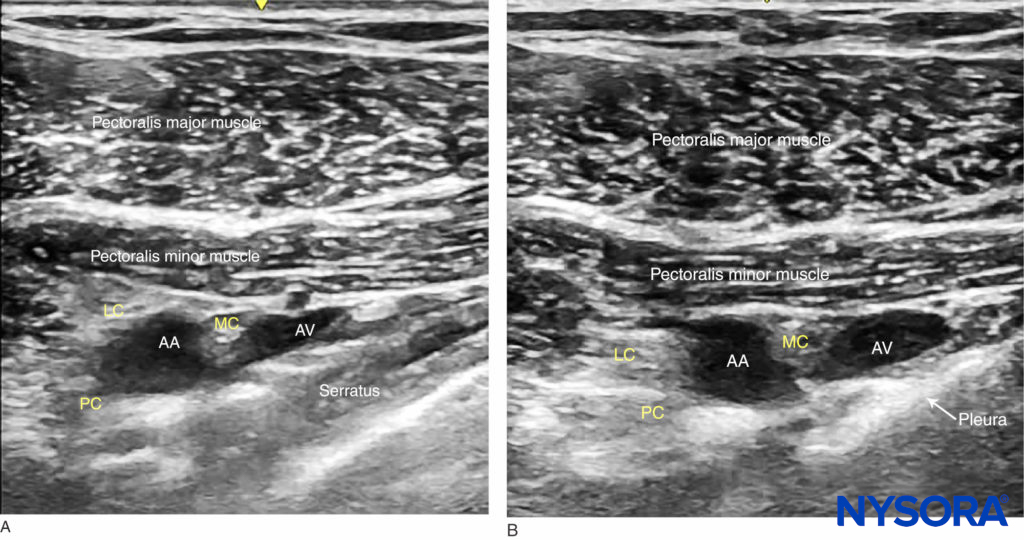
strong>FIGURE 5. Ultrasound-guided infraclavicular nerve block: a medial-to-lateral probe movement is used to avoid the area where the needle advanced in the parasagittal plane could enter the pleura. (A) Parasagittal lateral view: the serratus anterior is seen between the neurovascular bundle and the pleura. (B) In this probe position, the pleura lies closer to the brachial plexus.
GOAL
The goal of the technique is to inject local anesthetic until the spread around the artery is verified by ultrasound. It is not necessary to identify and target individual cords. Instead, injection of local anesthetic to surround the artery in an U-shaped pattern (cephalad, caudad, and posterior) suffices for the nerve block of all three cords.
From the Regional Anesthesia Manual: Reverse Ultrasound Anatomy for an infraclavicular brachial plexus block with needle insertion in-plane and local anesthetic spread (blue). AA, axillary artery; AV, axillary vein; LC, lateral cord; MC, medial cord; PC, posterior cord.
TECHNIQUE
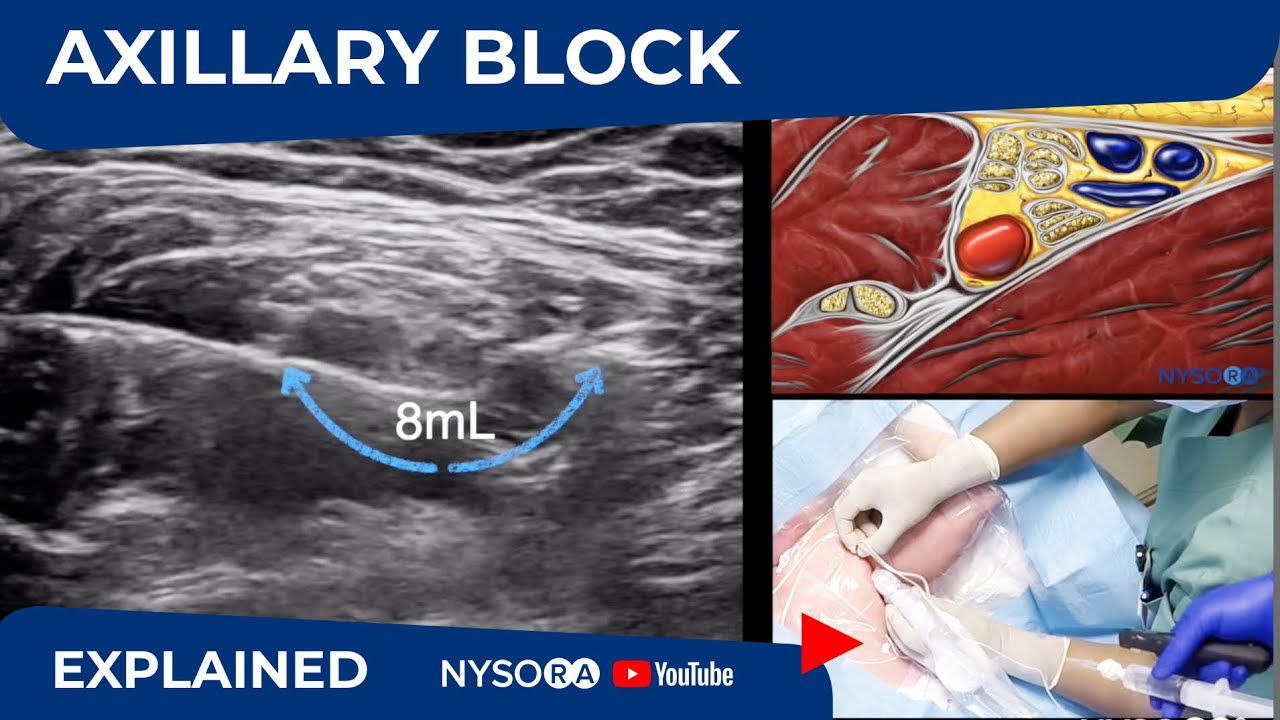
With the patient in the proper position, the skin is disinfected and the transducer is positioned in the parasagittal plane to identify the axillary artery (see Figure 3 and 4). This may require adjustment of the depth, depending on the thickness of the patient’s chest wall musculature. The axillary artery is typically seen between 3 and 5 cm. Once the artery has been identified, an attempt is made to identify the hyperechoic cords of the brachial plexus and their corresponding positions relative to the artery, although these may not always be identifiable. Fortunately, visualization of the cords are not necessary for successful block. The needle is inserted in-plane from the cephalad end of the probe, with the insertion point just inferior to the clavicle (see Figure 4). The needle is aimed toward the posterior aspect of the axillary artery and passes through the pectoralis major and minor muscles. If nerve stimulation is used concurrently (0.5–0.8 mA, 0.1 msec), the first motor response is often from the lateral cord (either elbow flexion or finger flexion). As the needle is advanced farther beneath the artery, a posterior cord motor response may appear (finger and wrist extension). After careful aspiration, 1–2 mL of local anesthetic is injected to confirm proper needle placement and spread. The injectate should spread cephalad and caudad to cover the lateral and medial cords, respectively (Figure 6).
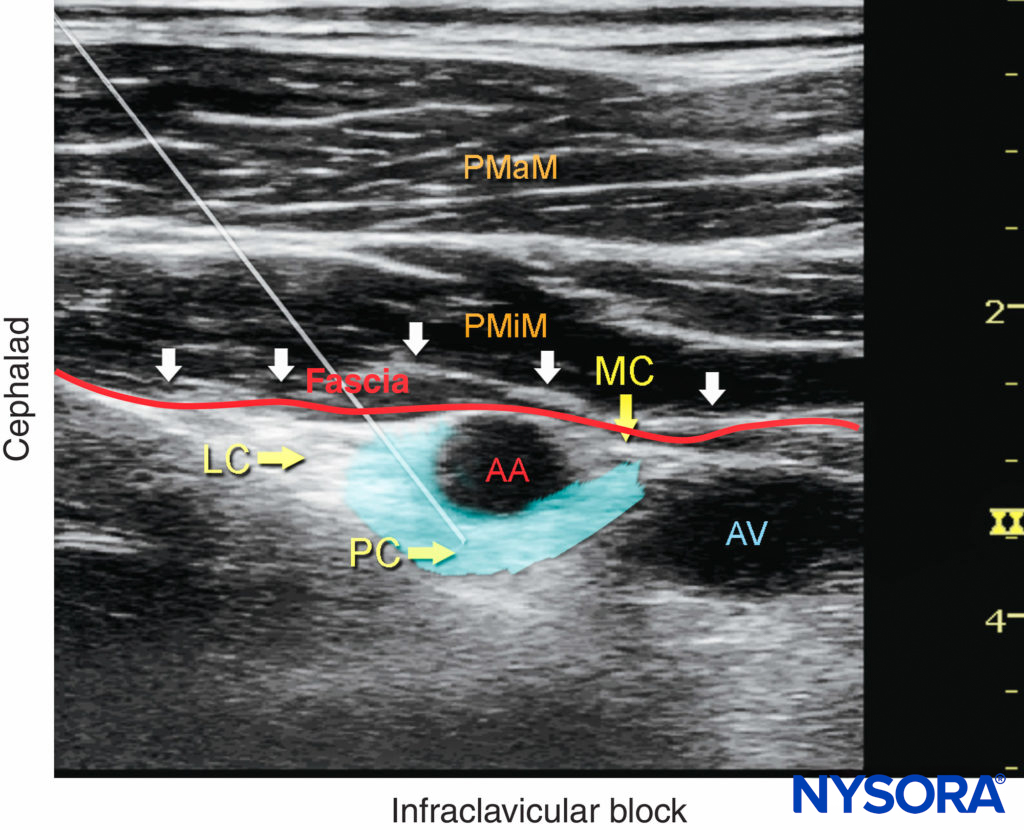
FIGURE 6. Ultrasound image demonstrating an ideal needle path for the infraclavicular brachial plexus nerve block. The blue-shaded area mimics an ideal spread of local anesthetic around the axillary artery (AA) and reaches all three cords of the brachial plexus (the lateral cord [LC], posterior cord [PC], and medial cord [MC]) below the fascia (red line) of the pectoralis minor muscle (PMiM), pectoralis major muscle (PMaM), and axillary vein (AV).
When a single injection of local anesthetic does not appear to result in adequate spread, additional needle repositioning and injections around the axillary artery may be necessary. In an adult patient, 20–30 mL of local anesthetic is usually adequate for successful block. Although a single injection of such a large volume of local anesthetic often suffices, it may be beneficial to inject two to three smaller aliquots at different locations to ensure local anesthetic spread in all planes containing the brachial plexus. There have been reports of septa hindering the diffusion of local anesthetic around the artery, and when that appears to be the case, repositioning the needle tip to achieve a U-shaped spread will ensure nerve block success. Alternative approaches to nerve block the brachial plexus distal to the clavicle have been described. A Single injection in between the cords at a more cephalad level (the costoclavicular space), where the brachial plexus can be visualized lateral to the artery (Figure 7).
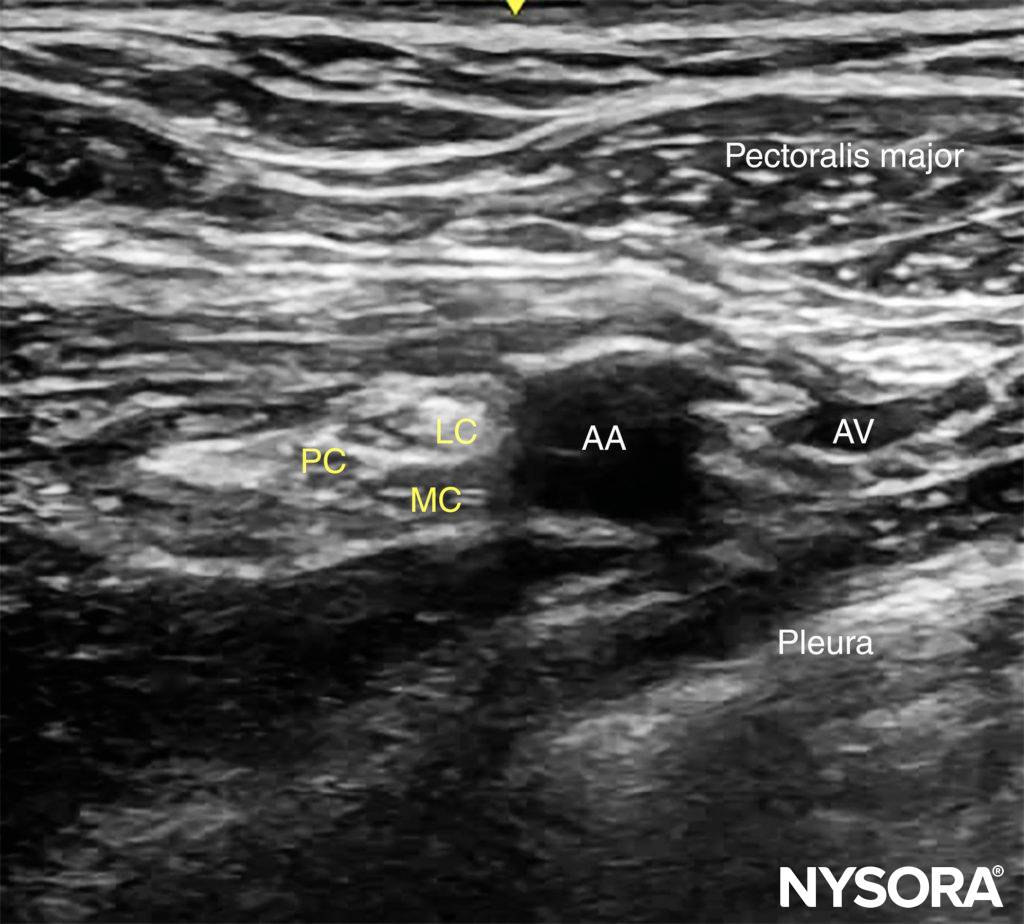
FIGURE 7. Ultrasound view of the brachial plexus at the costoclavicular space. The lateral (LC), medial (MC) and posterior (PC) cords are clustered together lateral to the axillary artery lying more superficial. At this level, the pectoralis minor is not seen deep to the pectoralis major.
TIPS
• An artifact posterior to the artery is often misinterpreted as the posterior cord. Figure 6.
• A “heel-up” maneuver (rocking the probe toward the patient’s head in a parasagittal plane, depressing the tissues caudad to the probe) makes it easier to change the needle’s angle as needed (see Figure 4).
• To decrease the risk of complications, adhere to the following guidelines:
• Aspirate intermittently every 5 mL to decrease the risk of intravascular injection.
• Do not inject if the injection resistance is high (> 15 psi).
CONTINUOUS ULTRASOUND-GUIDED INFRACLAVICULAR NERVE BLOCK
The goal of the continuous infraclavicular nerve block is similar to the non–ultrasound-based techniques: to place the catheter within the vicinity of the cords of the brachial plexus beneath the pectoral muscles. The procedure consists of three phases: (1) needle placement; (2) catheter advancement; and (3) securing the catheter. For the first two phases of the procedure, ultrasound can be used to ensure accuracy in most patients. The needle is typically inserted in-plane from the cephalad to caudad direction, similar to the single-injection technique (Figure 8). As with the single-injection technique, the needle tip should be placed posterior to the axillary artery prior to injection and catheter advancement. Proper needle placement can also be confirmed by obtaining a motor response of the posterior cord (finger or wrist extension), at which point 1–2 mL of local anesthetic is injected. The rest of the technique, advancing and securing the catheter is the same as previously described (continuous nerve block section, Ultrasound-Guided Interscalene Brachial Plexus Nerve Block). A typical starting infusion regimen is 5 mL/h, followed by 8-mL patient-controlled boluses every hour. The larger bolus volume is necessary for the adequate spread of the injectate around the artery so that all cords of the brachial plexus are reached.

FIGURE 8. The patient position, imaging, and needle placement for continuous infraclavicular brachial plexus nerve block are similar to those for a single-injection technique. Once proper needle tip placement is determined by the injection of a small volume of local anesthetic, the catheter is inserted 2–4 cm beyond the needle tip.
Follow the link to Continuous Peripheral Nerve Blocks for additional information.
Clinical updates
Aguilera et al. (Regional Anesthesia & Pain Medicine, 2025) demonstrate that for ultrasound-guided infraclavicular brachial plexus block with perineural epinephrine and dexamethasone, 0.5% bupivacaine alone significantly prolongs motor block (≈28 vs 19 h), sensory block (≈29 vs 19 h), and postoperative analgesia (≈38 vs 24 h) compared with a 0.25% bupivacaine–1% lidocaine mixture, at the cost of a slower onset (35 vs 20 min). Rebound pain and block success rates were similar, with no increase in complications. These data suggest that avoiding lidocaine maximizes block duration when prolonged analgesia is prioritized and rapid onset is less critical.
- Read more about the study HERE.