FACTS
- Indications: Postoperative analgesia for hip surgery, meralgia paresthetica, and muscle biopsy of the proximal lateral thigh
- Transducer position: Transverse, inferior to the anterior superior iliac spine; the lateral edge of the sartorius muscle should be visualized with ultrasound
- Goal: Local anesthetic spread around LFCN between the tensor fasciae latae and sartorius muscles
- Local anesthetic: 5 mL (adults)
GENERAL CONSIDERATIONS
The lateral femoral cutaneous nerve (LFCN) divides into several branches innervating the lateral and anterior aspects of the thigh. Of note, in 45% of patients, innervation of the LFCN extends even to the anterior thigh. The variable anatomy of the lateral femoral cutaneous nerve makes it challenging to perform an effective landmark-based block. US guidance, however, allows for more accurate needle insertion into the appropriate fascial plane through which the LFCN passes.
ULTRASOUND ANATOMY
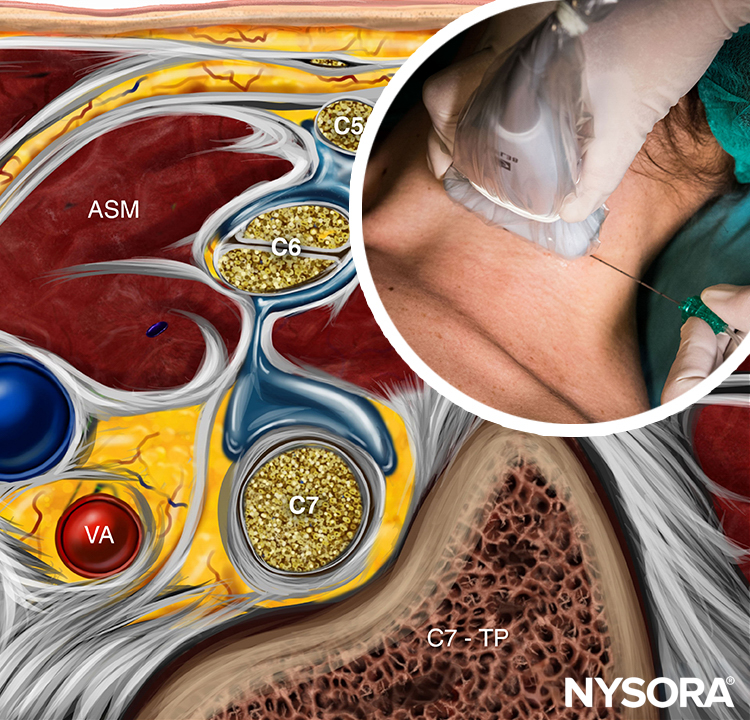
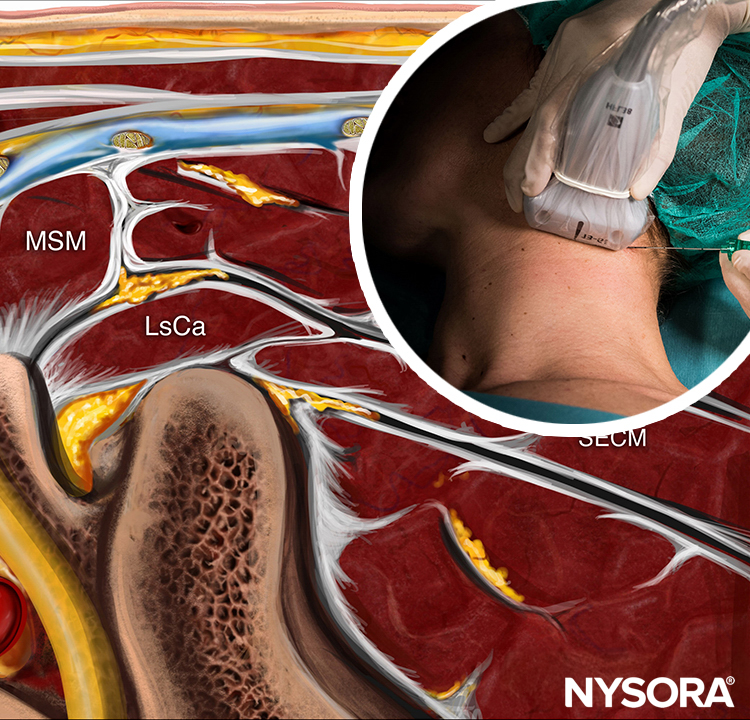
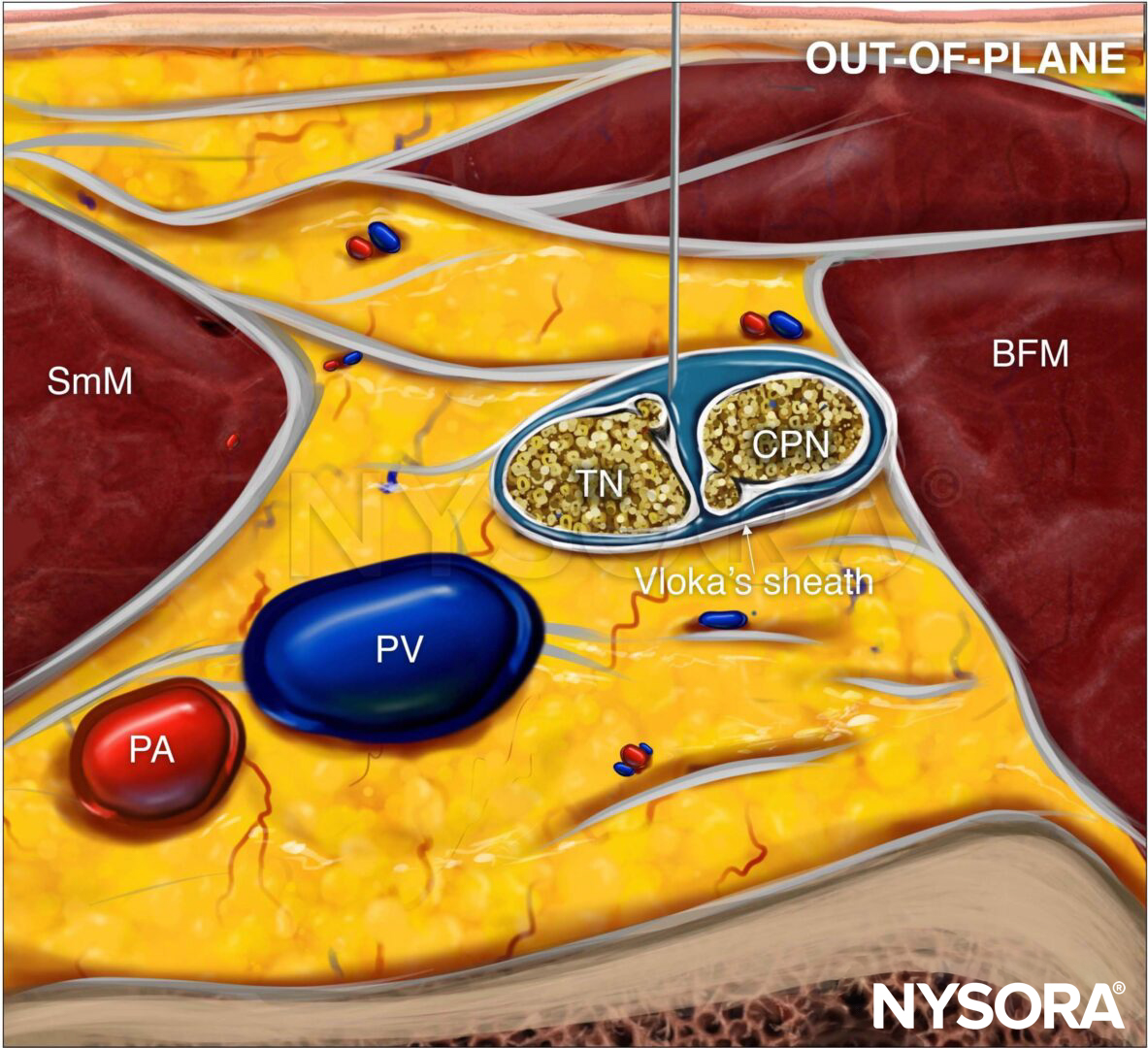
The LFCN typically is visualized between the tensor fasciae latae muscle (TFLM) and the sartorius muscle (SaM), 1–2 cm medial and inferior to the anterior superior iliac spine (ASIS) and 0.5–1.0 cm deep to the skin surface (Figure 1). Ultrasound (US) imaging of the LFCN yields an oval hypoechoic small structure with a hyperechoic rim that can be easily seen in the hypoechoic background. The LFCN can be traced proximally, as it runs from the lateral to the medial edge of the superficial fascia of the SaM. The lateral edge of the SaM is a useful landmark, and as such, it can be relied on throughout the procedure. The posterior branch of the LFCN may sometimes be seen across the anterior margin of the TFLM.
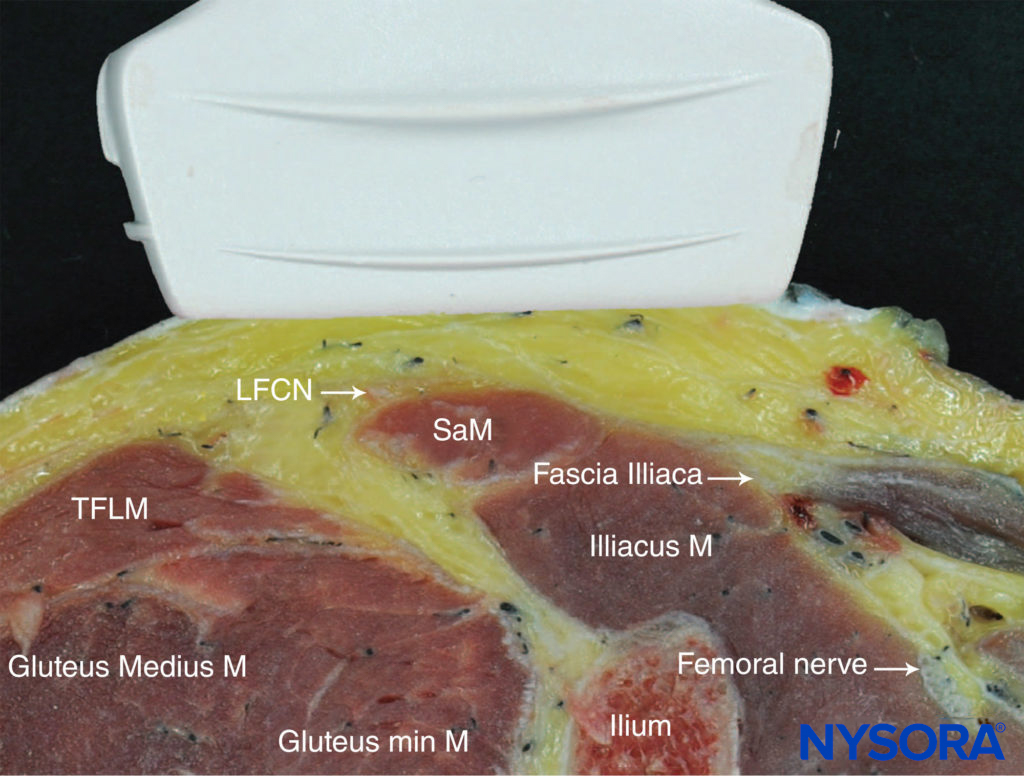
FIGURE 1. Cross-sectional anatomy of the lateral femoral cutaneous nerve (LFCN). Shown are the LFCN, sartorius muscle (SaM), and tensor fasciae latae muscle (TFLM). (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
DISTRIBUTION OF ANESTHESIA
Block of the LFCN provides anesthesia or analgesia in the anterolateral thigh. There is a large variation in the area of sensory coverage among individuals because of the highly variable course of the LFCN and its branches (Figure 2).

EQUIPMENT
The equipment recommended for an LFCN block is as follows:
- Ultrasound machine with a linear transducer (18-6 MHz), sterile sleeve, and gel
- Standard nerve block tray
- Syringe(s) with 10 mL of local anesthetic
- 3–5 cm, 22- to 24-gauge needle
- Sterile gloves
Learn more about Equipment for Regional Anesthesia.
LANDMARKS AND PATIENT POSITIONING
Block of the LFCN is performed with the patient in the supine or lateral position. Palpation of the anterior superior spine provides the initial landmark for transducer placement; the transducer is first positioned at 2 cm inferior and medial to the ASIS and adjusted accordingly. Typically, the nerve is identified slightly more distally in its course. Additional confirmation of the correct identification of the LFCN may be made by eliciting a tingling sensation on the lateral side of the thigh using a nerve stimulator.
GOAL
The goal is to inject local anesthetic in the plane between the TFLM and the SaM, typically 1–2 cm medial and inferior to the ASIS.
TECHNIQUE
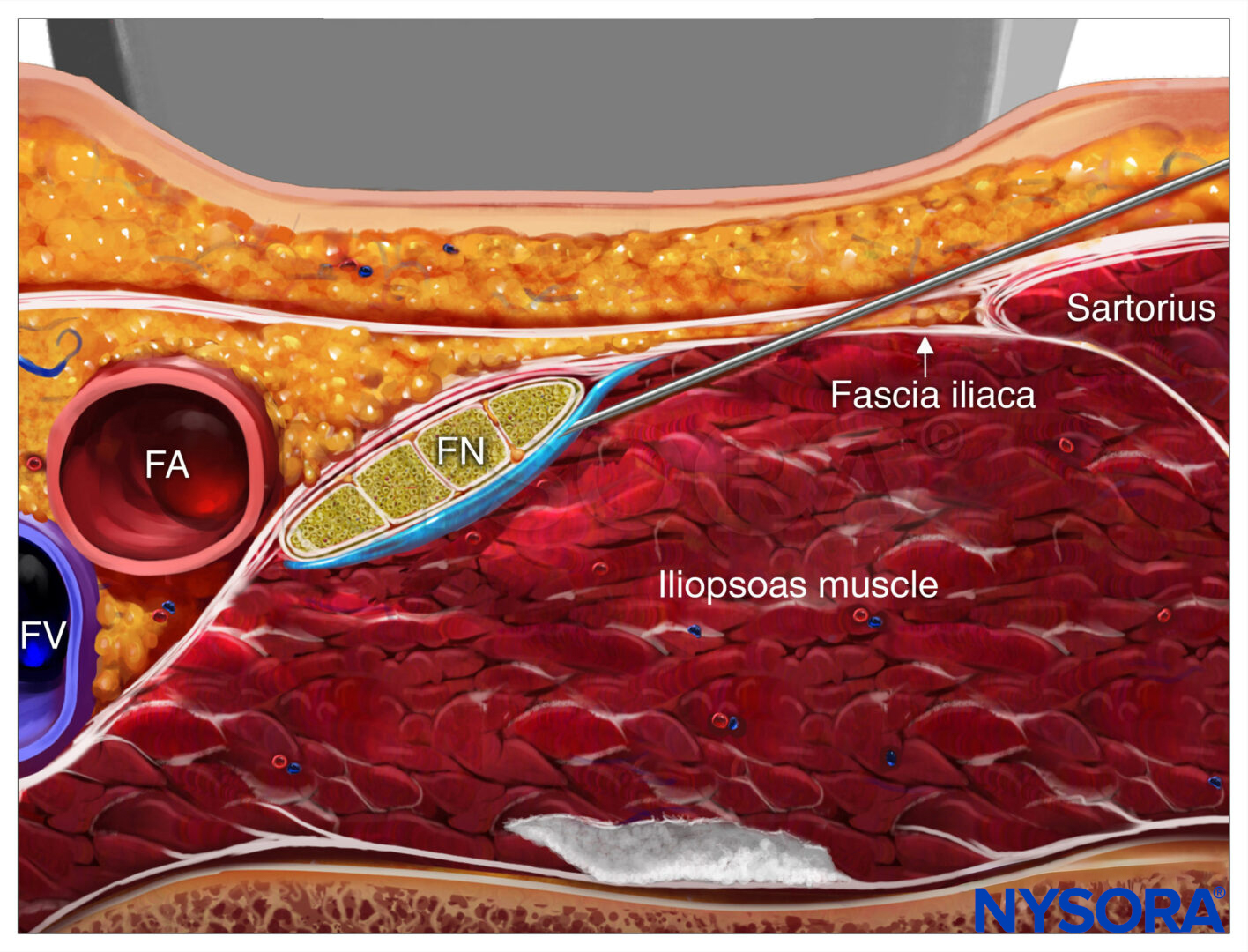
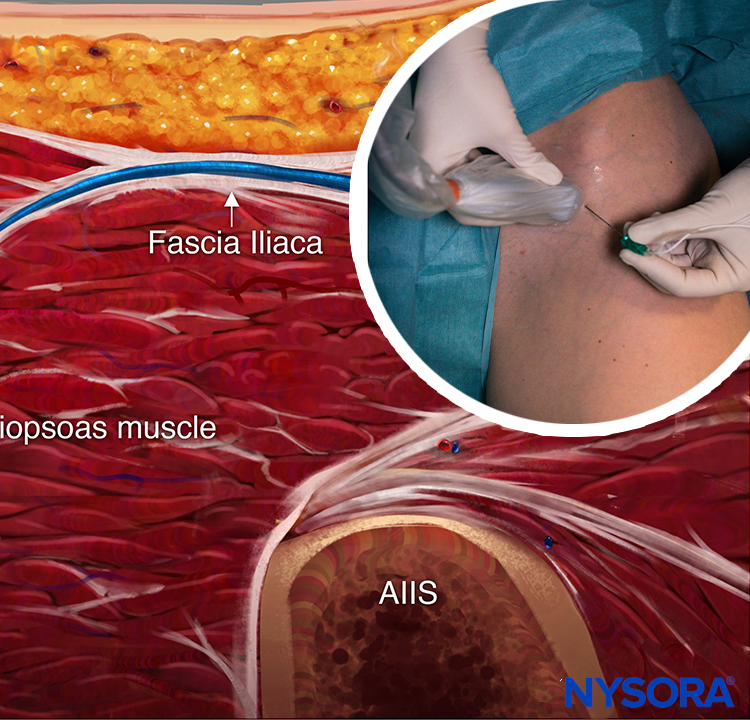
With the patient supine, the skin is disinfected and the transducer placed immediately inferior to the ASIS, parallel to the inguinal ligament (Figure 3). The TFLM and SaM are then identified. The nerve should appear as a small hypoechoic oval structure with a hyperochoic rim between the TFLM and SaM in a short-axis view or superficial to the SaM (Figure 4a).

FIGURE 3. Transducer position to accomplish a lateral femoral cutaneous nerve (LFCN) block.
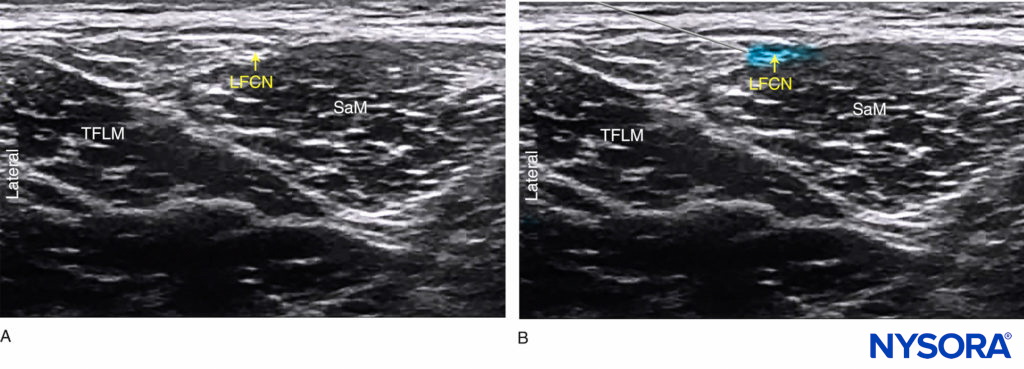
FIGURE 4. (A) Ultrasound anatomy of the lateral femoral cutaneous nerve (LCFN). (B) Simulated needle path and local anesthetic spread (blue-shaded area) to anesthetize the LFCN.
The needle is inserted in plane in a lateral-to-medial orientation, through the subcutaneous tissue. A fascial “pop” or “click” may be felt as the needle tip enters the plane between the TFLM and SaM. A volume of 1–2 mL of local anesthetic is injected to verify the needle tip position. The correct position is achieved by visualizing the spread of local anesthetic in the described plane between the TFLM and SaM or around the LFCN superficial to the SaM (Figure 4b).
TIPS
- A “subinguinal” technique has also been described, in which the US probe straddles the ASIS and the anterior inferior iliac spine (AIIS). Local anesthetic is injected under the inguinal ligament, 1–2 cm medial to the ASIS, without necessarily attempting to visualize the nerve.
- In an adult patient, 5 mL of local anesthetic is usually sufficient. In children, a volume of 0.15 mL/kg per side is adequate for effective analgesia.
For a more comprehensive review continue reading Ultrasound-Guided Fascia Iliaca Block
Clinical updates
Liang et al. (Journal of Anesthesia, 2023) report in a randomized trial of 92 total hip arthroplasty patients that pericapsular nerve group (PENG) block combined with lateral femoral cutaneous nerve (LFCN) block enabled earlier ambulation than supra-inguinal fascia iliaca compartment block (S-FICB), with a ~7-hour reduction in time to first postoperative walk. The PENG+LFCN strategy also produced greater early hip flexion and stronger quadriceps at 6 hours, indicating superior early motor preservation, whereas pain scores, opioid rescue, PONV, and block-related complications were similar between groups. These findings suggest PENG+LFCN may better support enhanced recovery pathways by facilitating early mobility without sacrificing analgesic safety or efficacy.
- Read more about the study HERE.