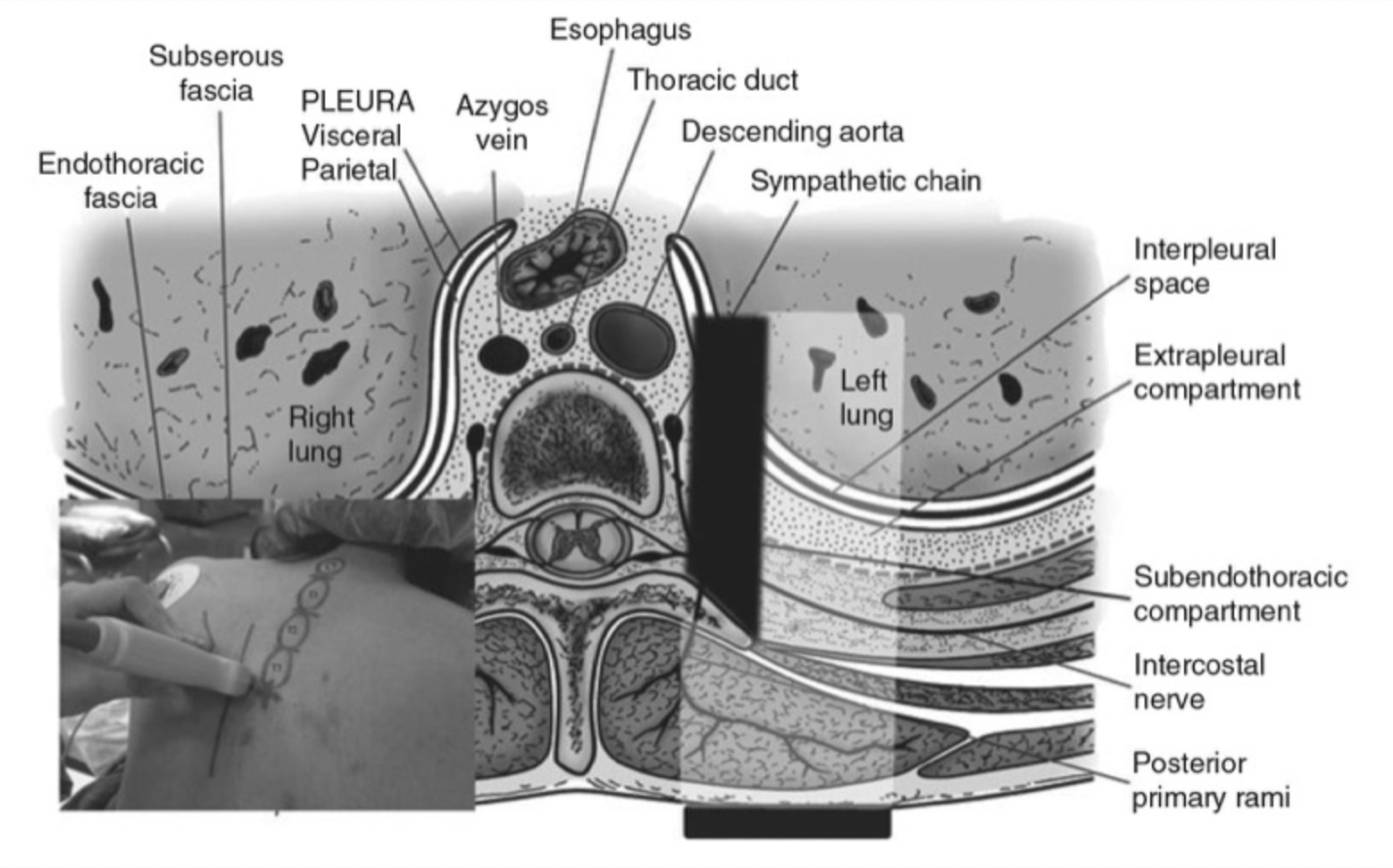
Peripheral nerve block techniques have traditionally been performed based on nerve identification from surface anatomical landmarks and neurostimulation. Anatomical variation among individuals often makes these techniques difficult and may result in variable success and serious complications such as bleeding, nerve injury, local anesthetic systemic toxicity (LAST), and pneumothorax. Ultrasound is the first imaging modality to be broadly used in regional anesthesia practice. Ultrasound-guided regional anesthesia (UGRA) uses real-time imaging to appreciate individual anatomic variations, precisely guide needle advancement, minimize local anesthetic dose, and visualize drug deposition around target structures (Fig. 1). These advantages over traditional methods have resulted in improved nerve block safety, efficacy, and efficiency [1, 2]. The brachial plexus and its branches are particularly amenable to sonographic examination, given their superficial location, with high-frequency (>10 MHz) linear array probes providing high-resolution images.
1. BRACHIAL PLEXUS ANATOMY
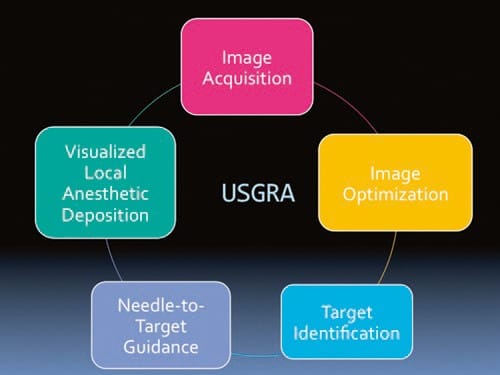
Fig. 1 The core components of safe ultrasound-guided regional anesthesia. The image is acquired in the desired anatomical region and is optimized through adjustments of depth of field, gain (brightness), and focus. A broad anatomical scan allows identification of the target structures and those to be avoided, such as vessels and lung, to plan a safe needle path. The needle is guided to the target in real time while maintaining a view of the needle tip. The deposition of local anesthetic is visualized in real time. (Reproduced with permission from www.usra.ca)
Thorough knowledge of brachial plexus anatomy is required to facilitate block placement and to optimize patient-specific block selection. The four traditional “windows” for brachial plexus block are the interscalene level (roots), supraclavicular level (trunks and divisions), infraclavicular level (cords), and axillary level (branches) (Fig. 2). However, the brachial plexus is best thought of as a continuum that may be imaged and anesthetized almost anywhere along its course.
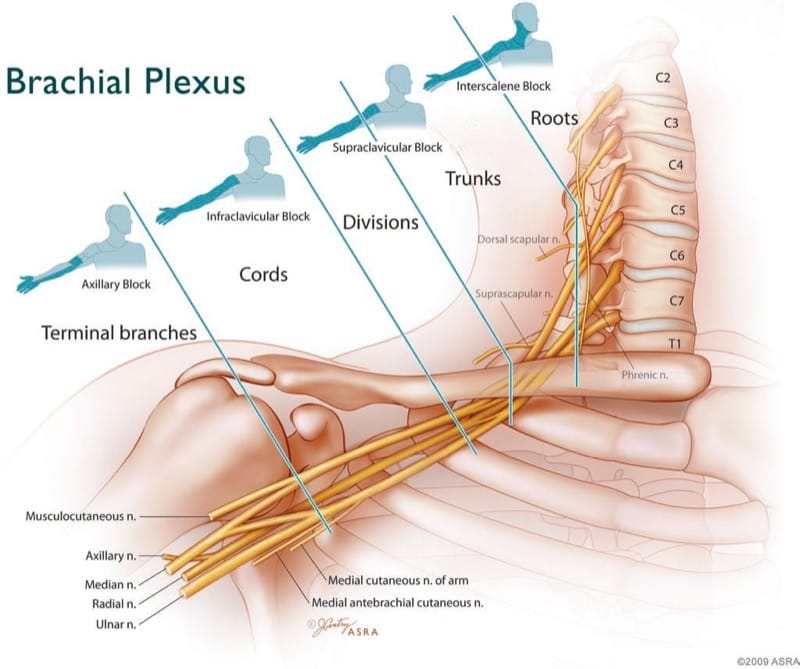
Fig.2 Idealized brachial plexus. Various approaches define individual brachial plexus blocks and their expected distribution of cutaneous anesthesia. (Copyright 2009 American Society of Regional Anesthesia and Pain Medicine. Used with permission. All rights reserved)
The brachial plexus provides sensory and motor innervation to the upper limb. It originates from the ventral primary rami of the fifth cervical (C5) to the first thoracic (T1) spinal nerve roots and extends from the neck to the apex of the axilla (Fig. 3). Variable contributions may also come from C4 to T2 nerves. The C5 and C6 rami typically unite near the medial border of the middle scalene muscle to form the superior trunk of the plexus. The C7 ramus becomes the middle trunk, and the C8 and T1 rami unite to form the inferior trunk. The C7 transverse process lacks an anterior tubercle, which facilitates the ultrasonographic identification of the C7 nerve root [3, 4]. The roots and trunks pass through the interscalene groove, a palpable surface anatomic landmark between the anterior and middle scalene muscles. The three trunks undergo primary anatomic separation into anterior (flexor) and posterior (extensor) divisions at the lateral border of the first rib [5]. The anterior divisions of the superior and middle trunks form the lateral cord of the plexus, the posterior divisions of all three trunks form the posterior cord, and the anterior division of the inferior trunk forms the medial cord. The three cords divide and give rise to the terminal branches of the plexus, with each cord possessing two major terminal branches and a variable number of minor intermediary branches. The lateral cord contributes the musculocutaneous nerve and the lateral component of the median nerve. The posterior cord supplies the dorsal aspect of the upper extremity via the radial and axillary nerves. The medial cord contributes the ulnar nerve and the medial component of the median nerve. Important intermediary branches of the medial cord include the medial cutaneous nerves of the arm and forearm and the intercostobrachial nerve (T2) to innervate the skin over the medial aspect of the arm [4, 5]. The lateral pectoral nerve (C5-7) and the medial pectoral nerve (C8, T1) supply the pectoral muscles; the long thoracic nerve (C5-7) supplies the serratus anterior muscle; the thoracodorsal nerve (C6-8) supplies the latissimus dorsi muscle; and the suprascapular nerve supplies the supraspinatus and infraspinatus muscles.
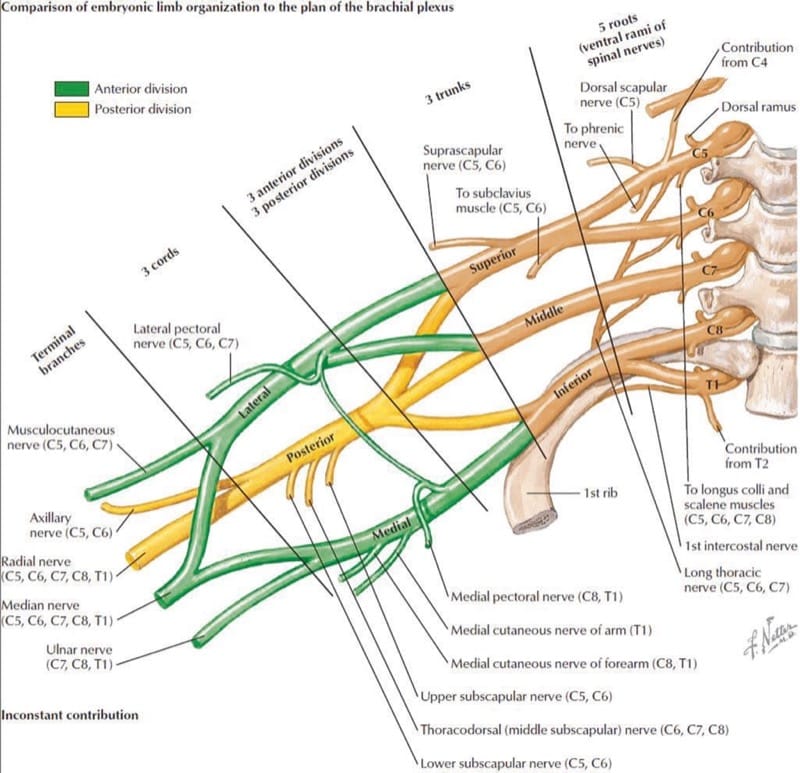
Fig.3 Anatomic representation of the embryonic limb organization of the brachial plexus. (Copyright Elsevier Netter Images. Used with permission)
The superficial cervical plexus (C1-4) lies in close proximity to the brachial plexus and gives rise to the phrenic nerve (C3-5), which supplies motor innervation to the diaphragm and lies ventral to the anterior scalene muscle; the supraclavicular nerve (C3-4) provides sensation from the “cape” of the shoulder to the lateral border of the scapula.
2. INTERSCALENE BLOCK
Anatomy
The roots of the brachial plexus are found in the interscalene groove defined by the anterior and middle scalene muscles. In slim patients, this groove can often be palpated along the lateral border of the sternocleidomastoid muscle at the level of the thyroid cartilage (C6).
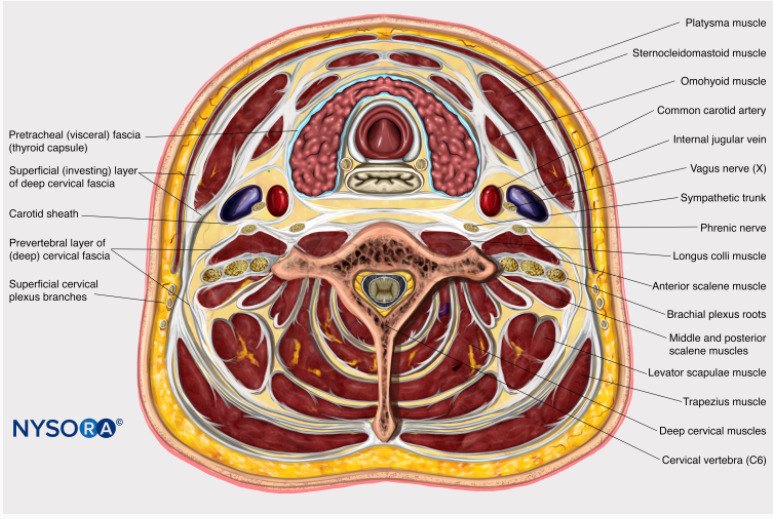
Cognitive aid: Transverse view of the brachial plexus at the level of the C6 vertebra.
For additional information check NYSORA Compendium: Interscalene Brachial Plexus Block
Indication
The interscalene block remains the approach of choice to provide anesthesia and analgesia for shoulder surgery, as it targets the proximal roots of the plexus (C4–C7). The inter- scalene space is not a contained fascial plane, as local anesthetic spread extends proximally to include the nonbrachial plexus supraclavicular nerve (C3–C4), which supplies sensory innervation to the “cape” of the shoulder and the phrenic nerve (C3-5), which supplies the ipsilateral hemidiaphragm [6]. The C5 and C6 roots are consistently blocked with this approach, therefore, offering reliable analgesia/anesthesia of the shoulder. Deltoid and bicep weakness are a typical finding. The more caudal roots of the plexus (C8–T1) are usually spared by this approach [7].
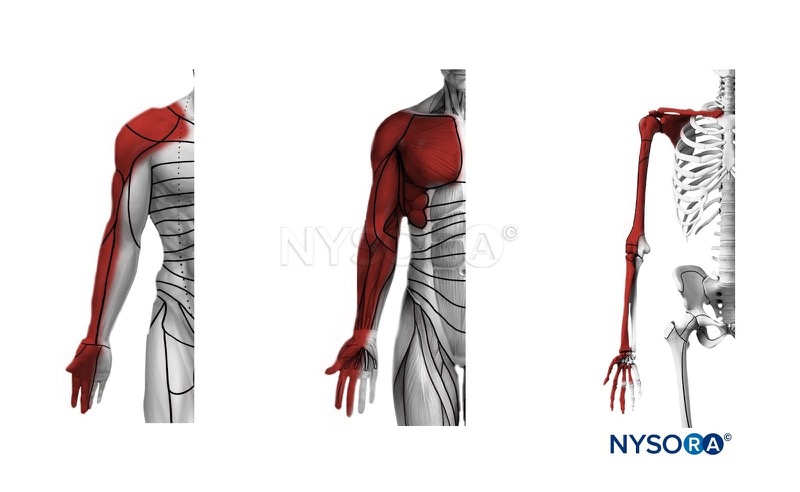
Cognitive aid: Anesthesia distribution with an interscalene brachial plexus block. Left: dermatomes, middle: myotomes, right: osteotomes.
For additional information check NYSORA Compendium: Interscalene Brachial Plexus Block
Procedure
The patient is positioned supine with the head turned 45° to the contralateral side and the arm adducted at the side. A high-frequency linear probe (>10 MHz) is recommended. As the plexus is usually very superficial (<3 cm) a 22-gauge, 50-mm block needle is sufficient. A transverse image of the plexus roots in the interscalene area is obtained on the lateral aspect of the neck in an axial oblique plane at the level of the cricoid cartilage (C6) (Fig. 4). The anterior and middle scalene muscles define the interscalene groove, located deep to the sternocleidomastoid muscle lateral to the carotid artery and internal jugular vein [8].
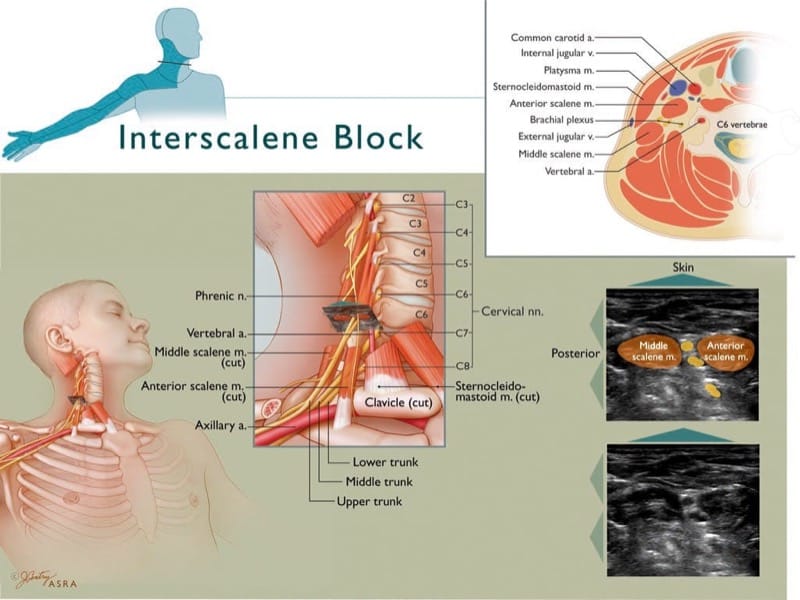
Fig.4 Interscalene block. The upper left inset depicts the expected distribution of anesthesia consequent to interscalene block. The roots converge to form trunks at the medial border of the middle scalene muscle. The vertebral artery lies medial to the anterior scalene muscle and anterior to the plexus. The classic ultrasound view depicts the hypoechoic upper roots (most likely C5–C7) stacked on each other, within the interscalene groove. The upper right inset depicts the closeness of the brachial plexus to major arteries and the spinal canal. (Copyright 2009 American Society of Regional Anesthesia and Pain Medicine. Used with permission. All rights reserved)
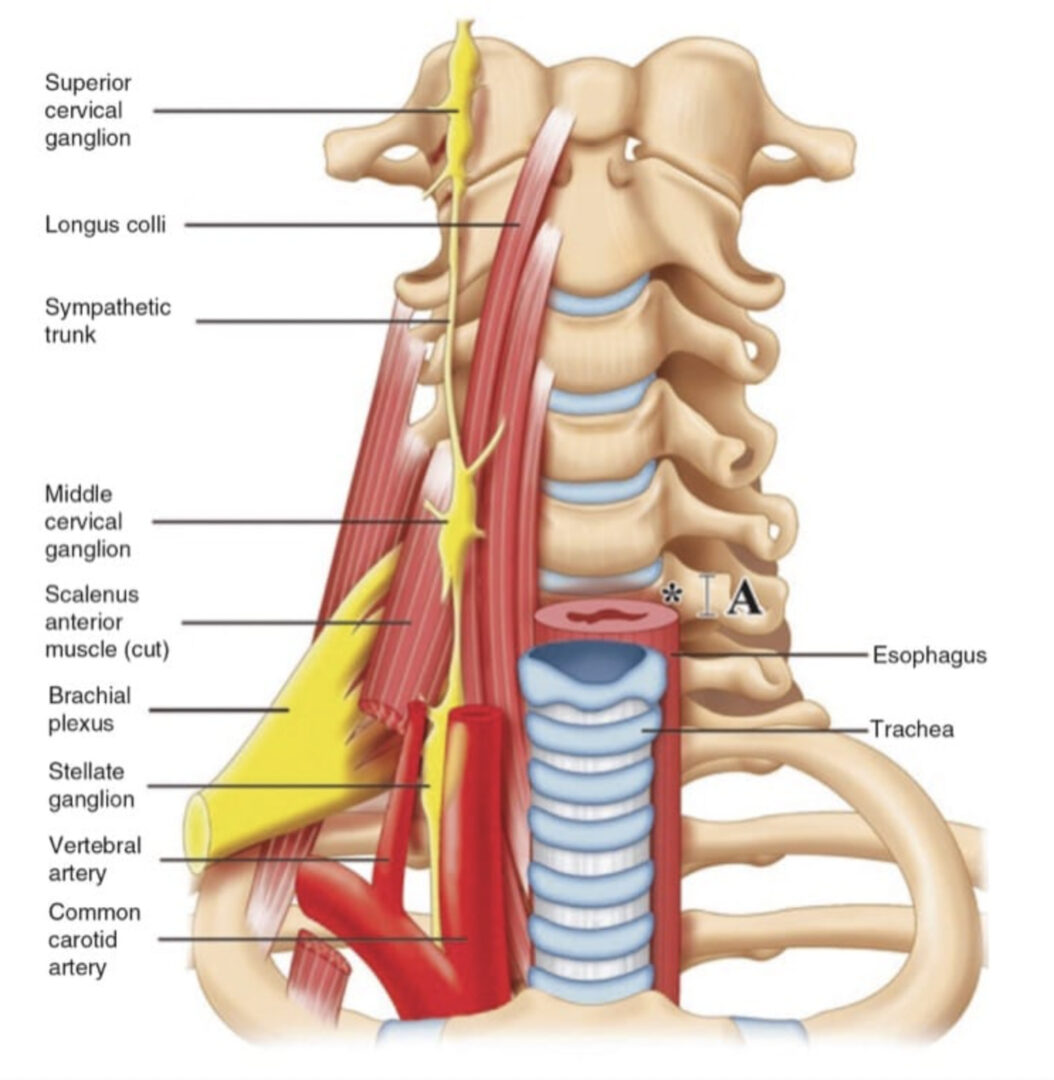
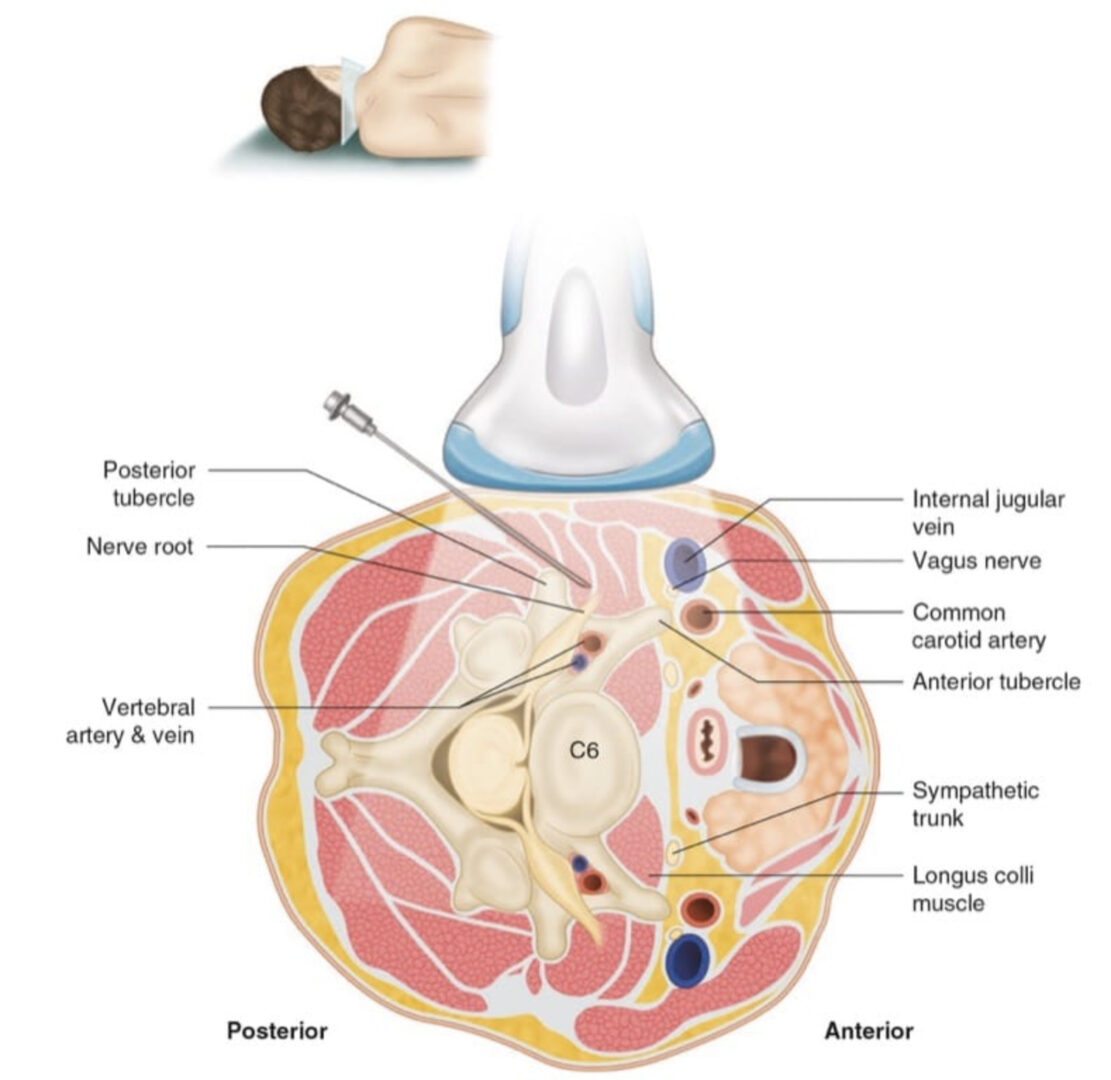
The interscalene nerve roots are best imaged at the C5-7 level, where they have a round or oval appearance in cross-section. The compact anatomy of the neck region and the hypoechoic nature of both the nerves and vessels make it prudent to first locate the plexus trunks at the supraclavicular level, where the anatomic relationship to the subclavian artery is highly reliable. The interscalene roots may then be located by using a “traceback” method in a cephalad direction. The individual root levels are identified by using the bony landmarks of the cervical vertebrae. Unlike the more proximal cervical vertebrae, the C7 vertebra lacks an anterior tubercle (Fig. 5), so the transverse processes of the C6 and C7 cervical vertebrae can be readily differentiated by the presence (in C6) or absence (in C7) of an anterior tubercle. Color Doppler may be used to identify the vertebral artery and vein located adjacent to the transverse process, which lies deep to the interscalene space. The transverse process of the C6 vertebra has both anterior and posterior tubercles (Fig. 6). The anterior tubercle of C6 (Chassaignac’s tubercle) is the most prominent of all the cervical vertebrae; it is bounded by the carotid artery anteriorly and the vertebral artery posteriorly. Recent data suggest that ultrasound guidance reduces the number of needle passes required to perform an interscalene block and achieves more consistent anesthesia of the lower trunk [9, 10].
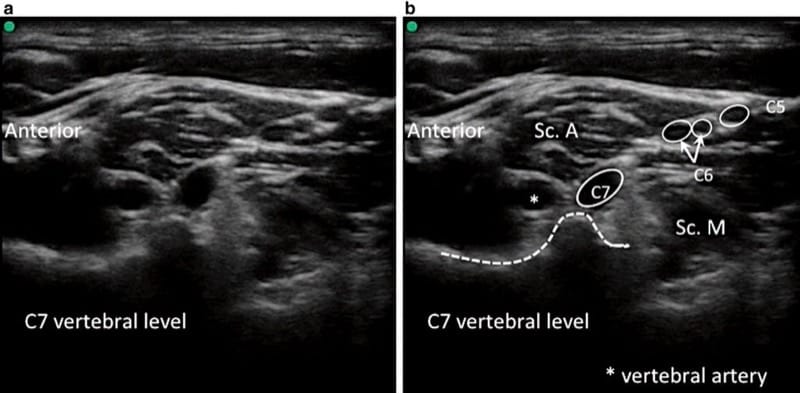
Fig.5 (a, b) The C7 vertebra. The C7 nerve root is posterior to the vertebral artery (asterisk) as it passes between the anterior scalene muscle (Sc. A) and the middle scalene muscle (Sc. M). The nerve roots of C6 (split) and C5 are also visible. Note that C7 lacks an anterior tubercle. (Reproduced with permission from www.usra.ca)
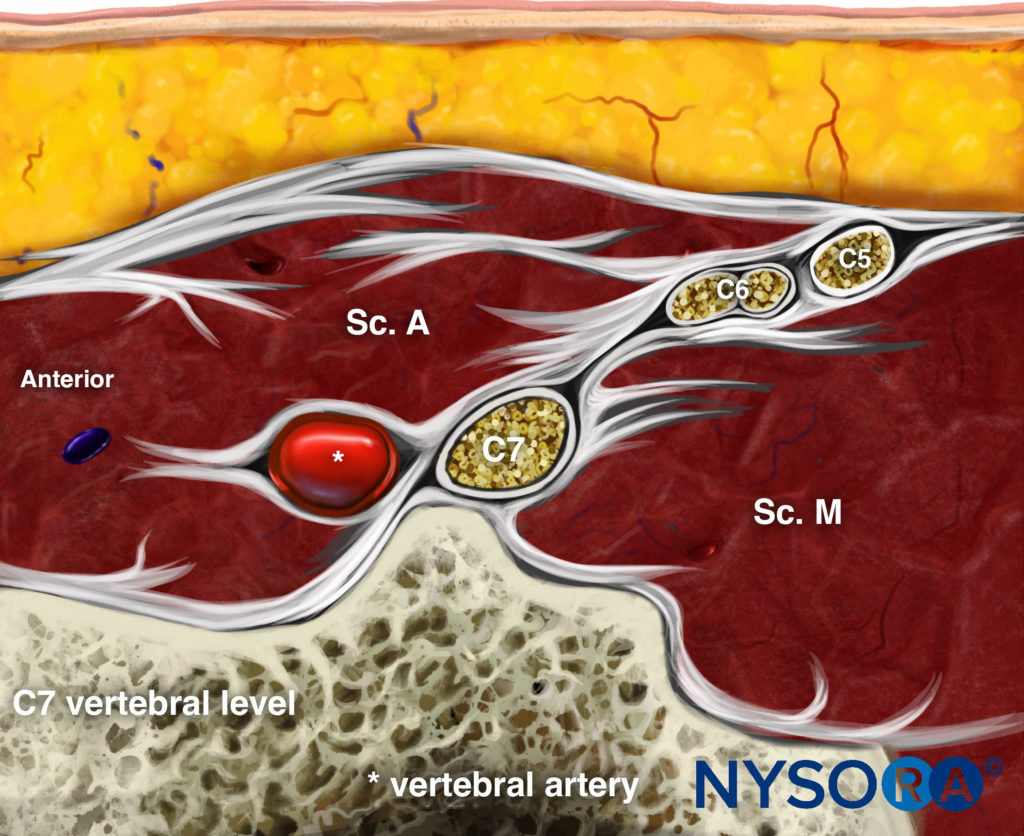
Reverse Ultrasound Anatomy illustration of figure 5. Sc. A, anterior scalene muscle; Sc. M, middle scalene muscle.
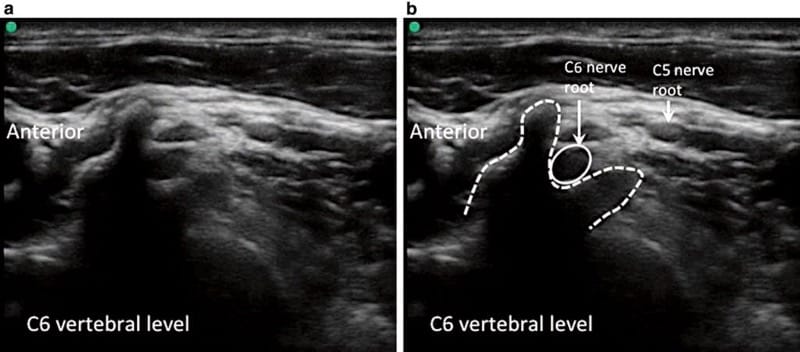
Fig.6 (a, b), The C6 vertebra. The C6 nerve root is visible between the anterior and posterior tubercles. The C5 nerve root is also visible more superficially. (Reproduced with permission from www.usra.ca)
One of the most common side effects of interscalene block is phrenic nerve palsy resulting in transient hemidiaphragmatic paresis [11]. Although it is usually asymptomatic in healthy patients, it may be poorly tolerated in patients with limited respiratory reserve. As a result, the interscalene block is relatively contraindicated in patients with significant respiratory disease. An ultrasound-guided interscalene block may provide adequate postoperative analgesia with only 5 mL of local anesthetic. There is a decreased incidence and severity of hemidiaphragmatic paresis with a low-dose block, compared with the more commonly used dose of 20 mL of the same local anesthetic solution [12]. An alternative to the interscalene block for patients in whom hemidiaphragmatic paresis is a concern is the combination of a suprascapular nerve block and an axillary nerve block [13].
Mechanical nerve injury may manifest as neurologic symptoms such as persistent pain, loss of motor function, and transient or permanent paresthesias. The brachial plexus above the clavicle has very high ratio of neural to nonneural connective tissue, so a high level of care is required, as it is postulated that the nerve roots may be at an increased risk of mechanical injury [14, 15]. Inadvertent intraneural injection during regional anesthesia practice is more common than previously thought [16]. An emerging area of study is focusing on defining the optimal plane of local anesthetic deposition, to be close enough to the neural targets to produce conduction anesthesia but also far enough to prevent inadvertent intraneural injection (Fig. 7) [17, 18]. Unintentional epidural or spinal anesthesia and spinal cord injury are very rare complications of interscalene block [19].
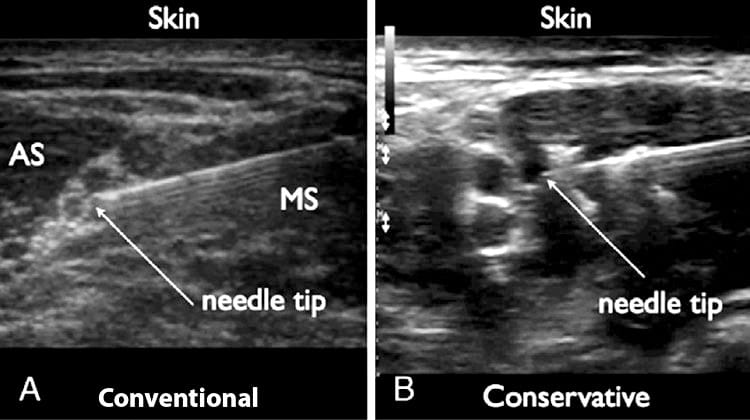
Fig.7 (a) “Conventional” interscalene block in which the needle tip is located between two roots. (b) More conservative needle tip position between the brachial plexus roots and the scalene muscle. The more conservative injection results in a “half-moon” spread of local anesthetic. AS, anterior scalene muscle; MS, middle scalene muscle. (Reproduced with permission from Sites et al. [18]
The close proximity of the vertebral artery to the nerve roots requires a high level of vigilance when performing interscalene block. The artery has a similar caliber to the nerve roots and also appears hypoechoic on ultrasound. Even a very small injection of local anesthetic into the vertebral artery may result in direct central nervous system toxicity and seizure. The routine use of color Doppler to aid in the identification of vascular anatomy can help prevent this complication.
3. SUPRACLAVICULAR BLOCK
Anatomy
In the supraclavicular area, the brachial plexus presents most compactly at the level of the trunks (superior, middle, and lower) and their respective anterior and posterior divisions. This explains its traditional reputation for a short latency and complete, reliable anesthesia [20]. The brachial plexus is located lateral and posterior to the subclavian artery as they both cross over the first rib and under the clavicle toward the axilla.
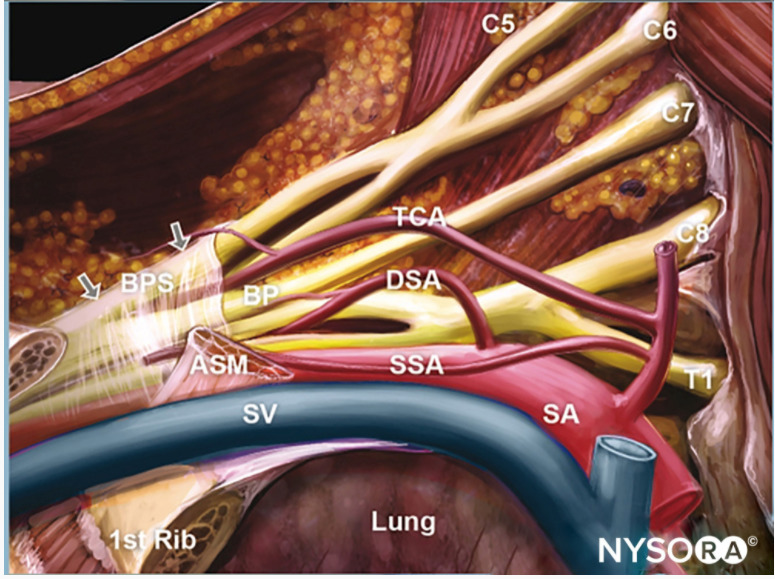
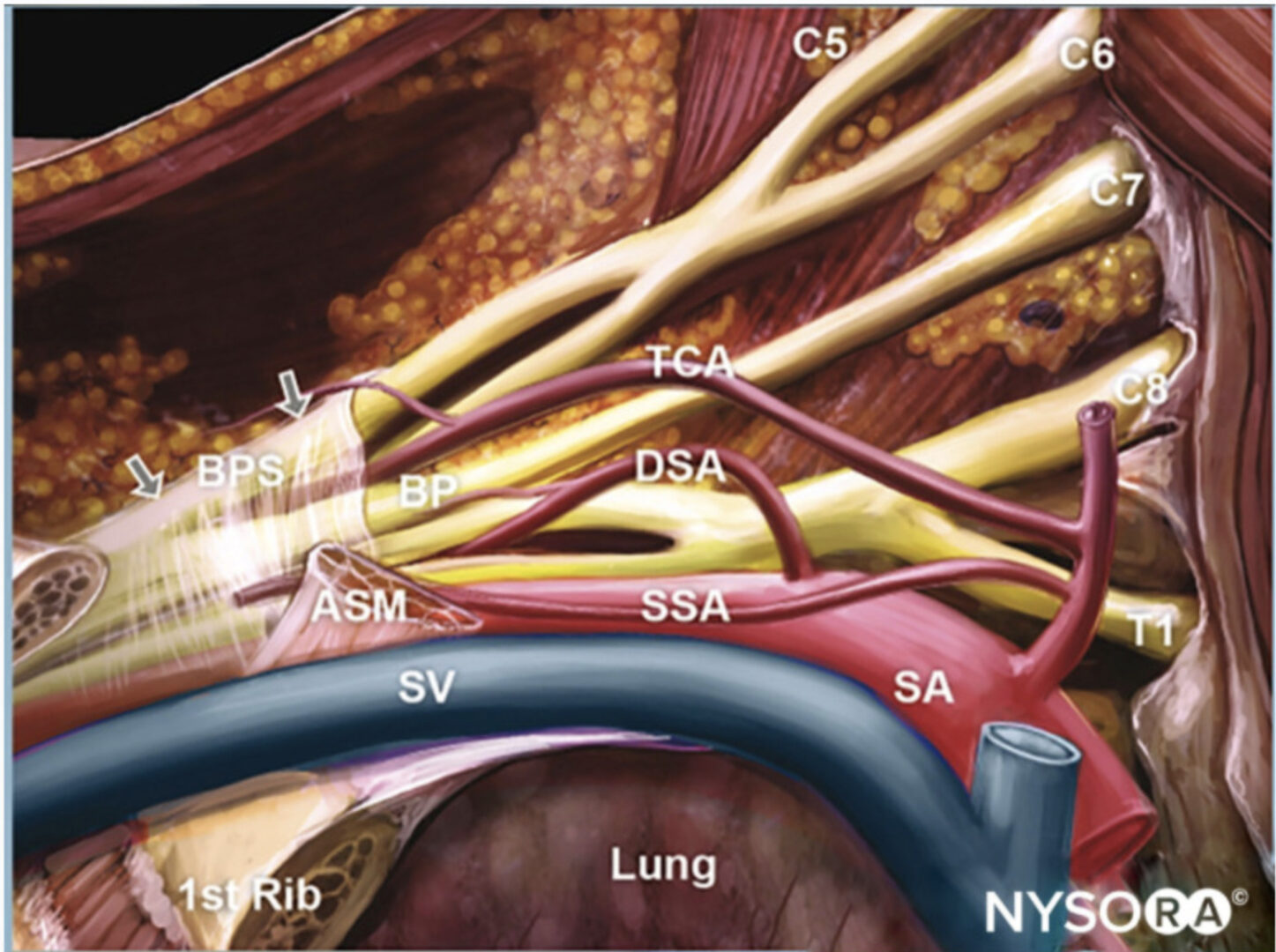
Cognitive aid: Anatomy of the brachial plexus and the subclavian artery. BPS, brachial plexus sheath; CL, clavicle; ASM, anterior scalene muscle; SA, subclavian artery; SV, subclavian vein; SSA, suprascapular artery; TCA, transverse cervical artery; DSA, dorsal scapular artery.
For additional information check NYSORA Compendium: Supraclavicular Brachial Plexus Block.
Indication
The supraclavicular approach to the brachial plexus is indicated for surgeries of the arm, forearm, or hand.
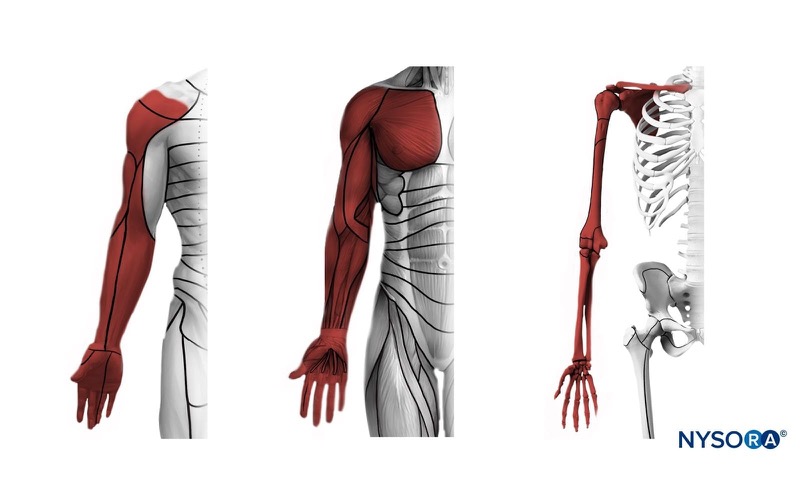
Cognitive aid: Anesthesia distribution with a supraclavicular brachial plexus block. Left: dermatomes, middle: myotomes, right: osteotomes.
For additional information check NYSORA Compendium: Supraclavicular Brachial Plexus Block.
Procedure
The patient is positioned supine with the head turned 45° contralaterally and the arm adducted at the side and slightly stretched to “open” the supraclavicular fossa. A high-frequency linear probe (>10 MHz) is recommended. The plexus is usually superficial (<3 cm from the skin surface), so a 22-gauge, 50-mm block needle is sufficient in most patients. A transverse view of the subclavian artery and the brachial plexus is obtained by scanning over the supraclavicular fossa in a coronal oblique plane parallel to the clavicle, aiming the ultrasound beam toward the chest cavity (Fig. 8). The subclavian artery is the primary ultrasonographic landmark, ascending from the mediastinum and traversing laterally over the pleural surface on the dome of the lung and later on the first rib. The hypoechoic nerve trunks are found cephalad to the first rib and posterolateral to the subclavian artery, appearing like a “cluster of grapes.”
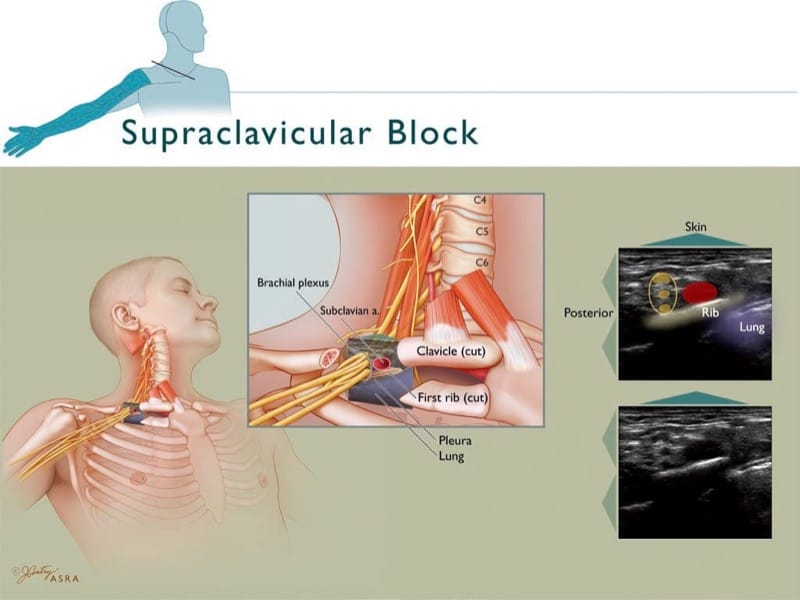
Fig.8 Supraclavicular block. The inset depicts the expected distribution of anesthesia consequent to supraclavicular block. The trunks begin to diverge into the anterior and posterior divisions as the brachial plexus courses below the clavicle and over the first rib. The plexus is posterior and lateral to the subclavian artery and both overlie the first rib in close approximation to the pleura and lung. The classic ultrasound view depicts the hypoechoic trunks bundled together lateral to the subclavian artery and over the first rib, which casts an acoustic shadow as the ultrasound beam is attenuated by bone. Note that the pleura do not impede the passage of the ultrasound beam to the same extent. (Copyright 2009 American Society of Regional Anesthesia and Pain Medicine. Used with permission. All rights reserved)
It is critical for the safe performance of supraclavicular block and the prevention of pneumothorax to properly recognize the sonoanatomy of the above structures. Although both rib and pleural surface appears as hyperechoic linear surfaces on ultrasound imaging, a number of characteristics can help differentiate one from the other. A dark, anechoic area underlies the first rib, whereas the area under the pleura often presents a shimmering quality with a “comet tail” sign. The pleural surface moves both with normal respiration and with subclavian artery pulsation, whereas the rib has no appreciable movement [21].
Once the image is optimized, a needle is advanced in-plane in either a medial or lateral direction. Local anesthetic is delivered within the plexus compartment, ensuring spread to the superior, middle, and inferior trunks. The inferior trunk is usually found in what has been called the “corner pocket” (Fig. 9) immediately above the first rib and lateral to the subclavian artery [22]. It may need to be specifically targeted to ensure lower trunk block.
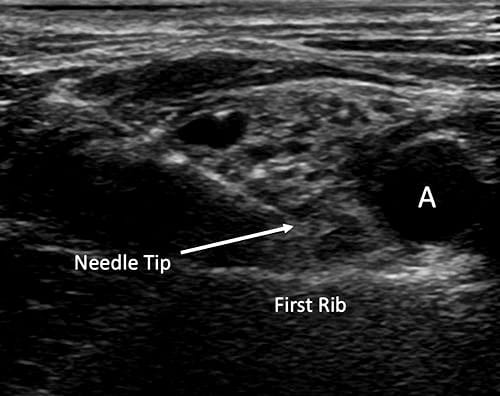
Fig.9 Supraclavicular block with the needle tip in the “corner pocket” between the subclavian artery (a) and the first rib. (Reproduced with permission from www.usra.ca)
The supraclavicular block remained unpopular for several decades prior to the introduction of ultrasound guidance because of a significant risk of pneumothorax. The ability to consistently image the first rib and pleura in real-time during block performance can conceivably minimize this risk, although direct comparative studies have not been done. A case series of 3000 nerve stimulator-guided supraclavicular perivascular blocks estimates the risk of pneumothorax to be 0.1% [23, 24].
The incidence of hemidiaphragmatic paresis in ultrasound-guided supraclavicular nerve block has not been clearly established, but it is considerably lower than the 50% incidence associated with the nerve stimulation technique [25, 26]. In a case series of 510 consecutive cases of ultrasound-guided supraclavicular block in patients without respiratory dysfunction, symptomatic hemidiaphragmatic paresis occurred in 1% of cases [21]. Caution should still be exercised when performing this block in patients who would be intolerant to the loss of the contribution of the ipsilateral diaphragm. Other uncommon complications in this case series were Horner’s syndrome (1%), unintended vascular puncture (0.4%), and transient sensory deficit (0.4%). The minimum volume of anesthetic required for UGRA supraclavicular block in 50% of patients is 23 mL, which is similar to recommended volumes for traditional nerve localization techniques [27]. Concomitant use of nerve stimulation does not seem to improve the efficacy of ultrasound-guided brachial plexus block [28].
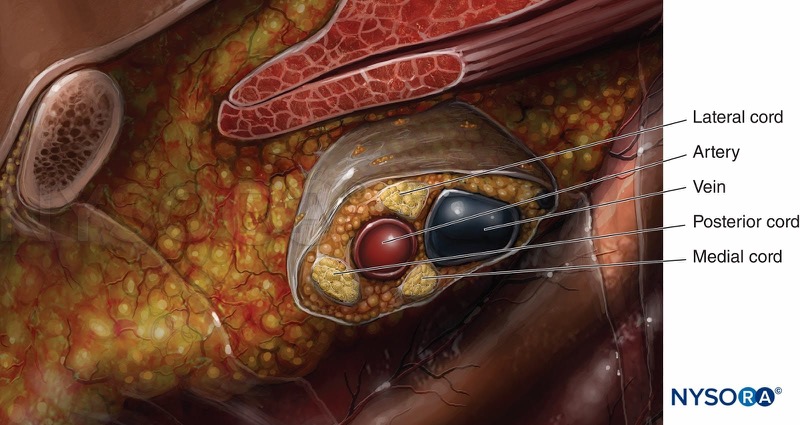
4. INFRACLAVICULAR BLOCK
Anatomy
At the level of the infraclavicular plexus, the cords are located posterior to the pectoralis major and minor muscles around the second part of the axillary artery; the lateral cord of the plexus lies superior and lateral, the posterior cord lies posterior, and the medial cord lies posterior and medial to the artery. The infraclavicular approach is the deepest of the windows to the brachial plexus, with the cords approximately 4–6 cm from the skin [29].
Cognitive aid: Brachial plexus cords and their relationship with the axillary artery.
For additional information check NYSORA Compendium: Infraclavicular Brachial Plexus Block.
Indication
This approach to the brachial plexus has similar indications to the supraclavicular block [30].
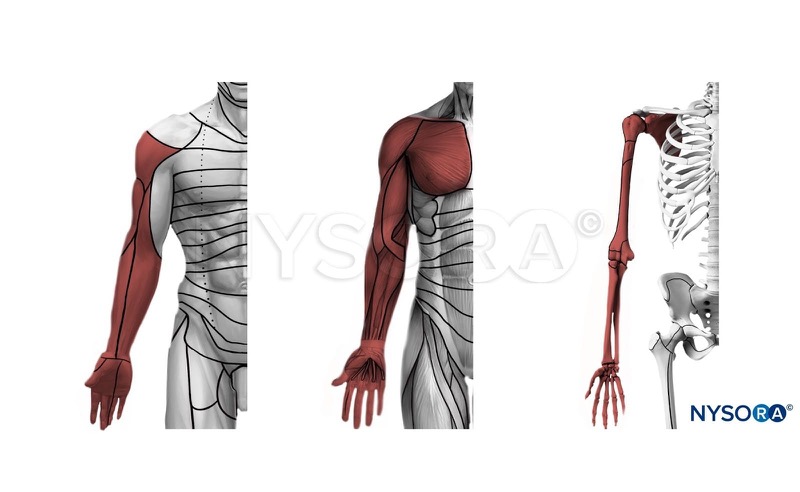
Cognitive aid: Anesthesia distribution with an infraclavicular brachial plexus block. Left: dermatomes, middle: myotomes, right: osteotomes.
For additional information check NYSORA Compendium: Infraclavicular Brachial Plexus Block.
Procedure
The patient is positioned supine with the arm adducted at the side or abducted 90° at the shoulder. Both linear and curved probes may be used to image the plexus in this area near the coracoid process in a parasagittal plane [31]. In children or slim adults, a 10-MHz probe may be used [32]. For many adults, however, a probe of lower resolution may be needed (e.g., 4–7 MHz) to obtain the required image penetration of up to 5–6 cm. A 22-gauge, 80-mm block needle is usually required. The axillary artery and vein can be readily identified in a transverse view, scanning in a parasagittal plane (Fig. 10). The three adjacent brachial plexus cords appear hyperechoic, with the lateral cord most commonly superior in the 9 o’clock to 12 o’clock position relative to the artery, the medial cord inferior to the artery (12–3 o’clock position), and the posterior cord posterior to the artery (5–9 o’clock position) [33]. Abducting the arm 110° and externally rotating the shoulder moves the plexus away from the thorax and closer to the surface of the skin, often improving identification of the cords [34]. A block needle is usually inserted in- plane with the ultrasound beam oriented along the parasagittal plane in a cephalocaudal direction. Medial needle orientation toward the chest wall must be avoided, as pneumothorax remains a risk with this approach [35]. The deposition of local anesthetic in a “U” shape posterior to the artery provides consistent anesthesia to the three cords [36, 37] (Fig. 11). Low-dose ultrasound-guided infraclavicular blocks (16 ± 2 mL) can be performed without compromise to block success or onset time [38]. The advantages of anesthetizing the brachial plexus at the infraclavicular level are the ability to consistently anesthetize the arm, including the axillary and musculocutaneous nerves, with limited risk of pneumothorax and hemidiaphragmatic paresis [39].
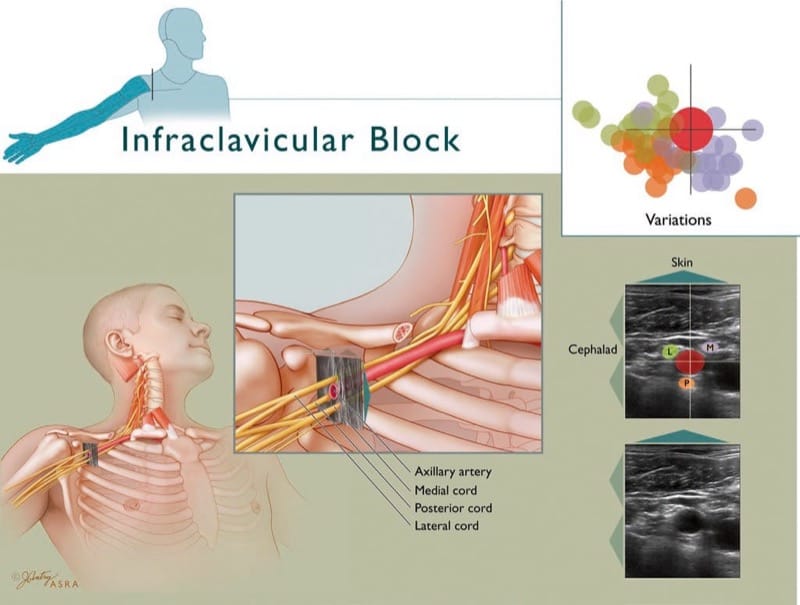
Fig.10 Infraclavicular block. Inset depicts the expected distribution of anesthesia consequent to infraclavicular block. The cords take on their characteristic position lateral, posterior, and medial to the second part of the axillary artery in this illustration of the coracoid approach. The medial cord frequently lies between the axillary artery and vein (at 4 o’clock). There is considerable variation in the relationship of the artery to the cords, as depicted by the color-coded cords in the upper right inset (lateral cord, green; medial cord, blue; posterior cord, orange). The color saturation correlates with the expected frequency of the cord residing in a specific location: the deeper the saturation, the more frequently the cord is found in that position. (Copyright 2009 American Society of Regional Anesthesia and Pain Medicine. Used with permission. All rights reserved)
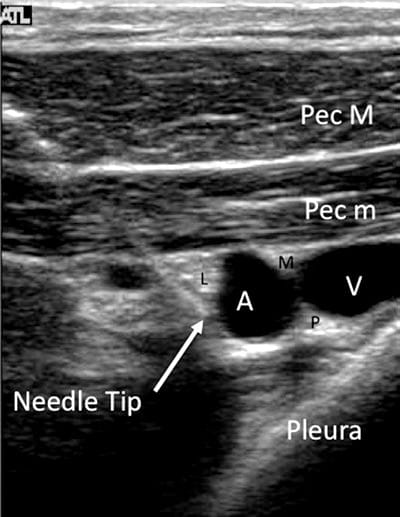
Fig.11 Infraclavicular block with the needle approaching the axillary artery (A) from cephalad. The lateral (L), medial (M), and posterior (P) cords are located around the artery. The axillary vein (V) and the pectoralis major (Pec M) and minor (Pec m) muscles, as well as the pleura, are clearly visible. (Reproduced with permission from www. usra.ca)
5. AXILLARY BLOCK
Anatomy
The axillary approach to the brachial plexus targets the terminal branches of the plexus, which include the median, ulnar, radial, and musculocutaneous nerves. The musculocutaneous nerve often departs from the lateral cord in the proximal axilla and is commonly spared by the axillary approach, unless specifically targeted.
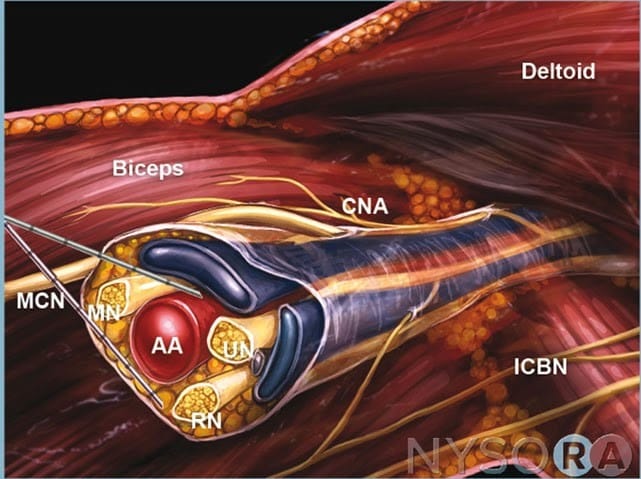
Cognitive aid: Terminal nerves of the brachial plexus at the axilla. CNA, cutaneous nerve of the arm; MN, median nerve; RN, radial nerve; UN, ulnar nerve; McN, musculocutaneous nerve; AA, axillary artery; IcbN, intercostobrachial nerve.
For additional information check NYSORA Compendium: Axillary Brachial Plexus Block.
Indication
Axillary brachial plexus block is best suited for upper limb surgery distal to the elbow.
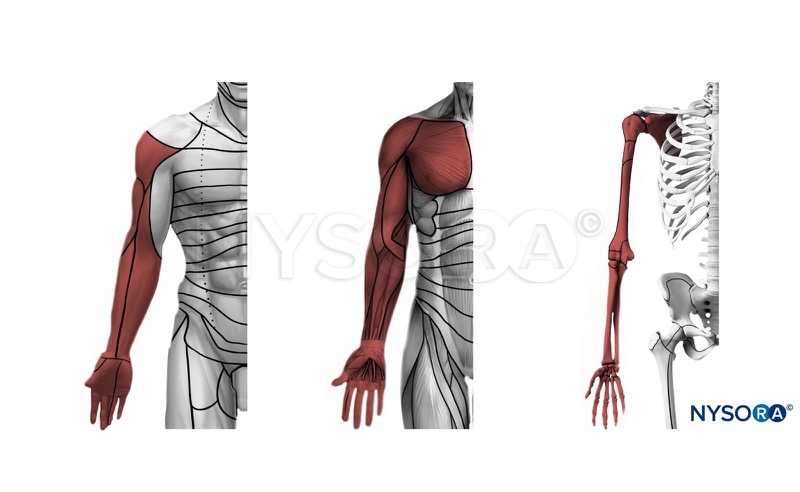
Cognitive aid: Anesthesia distribution with an axillary brachial plexus block. Left: dermatomes, middle: myotomes, right: osteotomes.
For additional information check NYSORA Compendium: Axillary Brachial Plexus Block.
Procedure
The patient is positioned supine with the arm abducted 90° at the shoulder. A high-frequency linear probe (>10 MHz) is recommended, and a 22-gauge, 50-mm needle is sufficient. The transducer is placed along the axillary crease, perpendicular to the long axis of the arm at the apex of the axilla. The median, ulnar, and radial nerves are usually located in close proximity to the axillary artery between the anterior muscle compartment of the proximal arm (biceps and coracobrachialis) and the posterior compartment (latissimus dorsi and teres major) [40] (Fig. 12). The conjoint tendon is the primary ultrasonographic landmark, arising from the confluence of the tendons of the latissimus dorsi and teres major muscles [41]. The nerve branches and the axillary artery lie superficial to this tendon. The nerve branches at the level of the axilla have mixed echogenicity and a “honeycomb” appearance representing a mixture of hypoechoic nerve fascicles and hyperechoic nonneural fibers. The median nerve is commonly found anteromedial to the artery, the ulnar nerve medial to the artery, and the radial nerve posteromedial to it, along the conjoint tendon (Fig. 13). The musculocutaneous nerve often branches off more proximally and may be located in a plane between the biceps and coracobrachialis muscles [42]. Separate block of each individual nerve is recommended to ensure complete anesthesia. Similar to other brachial plexus approaches, it is useful to use a needle-in-plane approach because of the superficial location of all terminal nerves. Ultrasound guidance has been associated with higher rates of block success and lower volumes of local anesthetic solution required, compared with nonimage-guided techniques [43, 44].
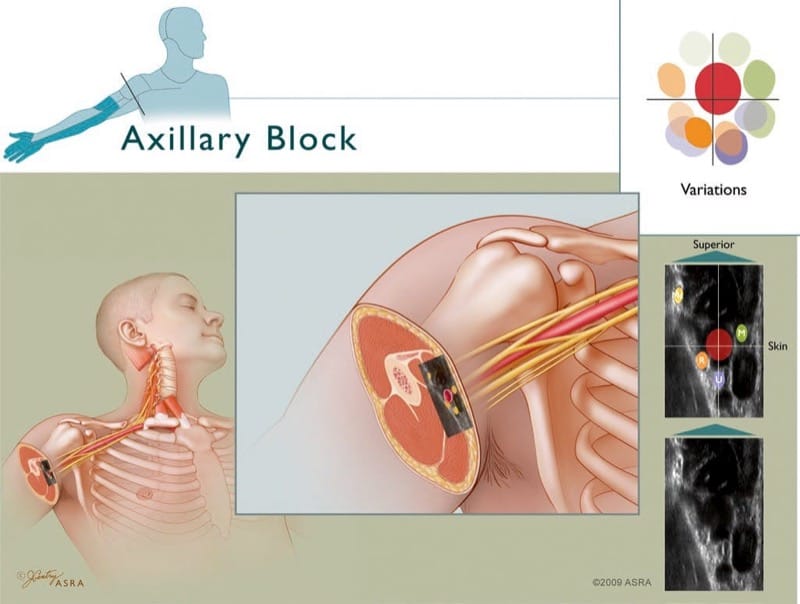
Fig.12 Axillary block. Top left inset depicts the expected distribution of anesthesia consequent to axillary block. The four terminal nerves are drawn in their classic relationship to the axillary artery, which in turn is correlated to ultrasonic anatomy that shows the hyper-echoic nerves. Note: to correlate with the illustration, the ultrasound inset is rotated 90° clockwise from the way it is normally viewed in a patient. There is significant variation in how the terminal nerves relate to the axillary artery. The upper right inset depicts these variations as color-coded nerves in various positions around the artery (radial nerve, orange; ulnar nerve, blue; median nerve, green). The color saturation correlates with the expected frequency of the nerve residing in a specific location; the deeper the saturation, the more frequently the nerve is found in that position. The musculocutaneous nerve (MC) lies in the fascial plane between the coracobrachialis and biceps muscles. (Copyright 2009 American Society of Regional Anesthesia and Pain Medicine. Used with permission. All rights reserved)
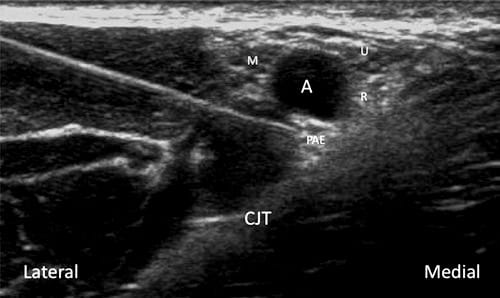
Fig.13 Axillary block at the level of the conjoint tendon (CJT). The median (M), ulnar (U), and radial (R) nerves are in close proximity to the axillary artery (A). The posterior acoustic enhancement (PAE) effect can sometimes be misinterpreted as the radial nerve. This can be verified by tracing the course of the radial nerve. (Reproduced with permission from www.usra.ca)
6. ANESTHETIZING DISTAL PERIPHERAL NERVES IN THE UPPER EXTREMITY
Anesthetizing individual nerves in the distal arm or forearm may be useful supplemental blocks if a single nerve territory is “missed” with a plexus approach. Scanning along the upper extremity, these peripheral nerves may be followed and blocked in many locations along their course. Generally, 5 mL of local anesthetic solution is sufficient to block any of the terminal nerves individually.
Some locations in the arm are frequently used: the median nerve can be located just proximal to the elbow crease and medial to the brachial artery (Fig. 14). The radial nerve can be located in the lateral aspect of the distal part of the arm, deep to the brachialis and brachioradialis muscles and superficial to the humerus (Fig. 15). The ulnar nerve may be blocked in the distal arm (proximal to the ulnar groove) or in the forearm, where it travels longitudinally, close to the ulnar artery (Fig. 16).
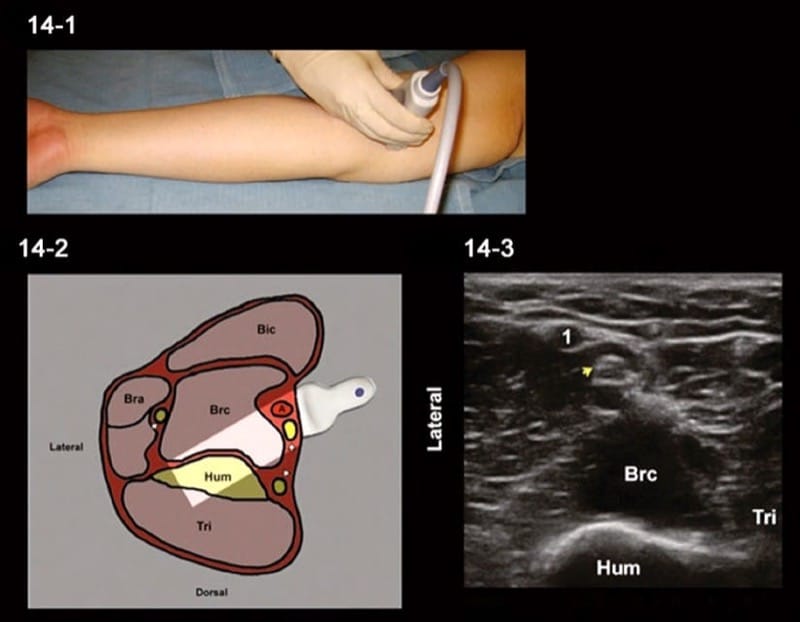
Fig.14 Median nerve block in the distal arm. (1) Ultrasound probe placement. (2) Anatomical structures within the ultrasound transducer range. (3) Ultrasound image of median nerve (arrowhead) in the distal arm. BA brachial artery, BM biceps muscle, Bra brachioradialis muscle, Brc brachialis muscle, Hum humerus, Tri triceps muscle
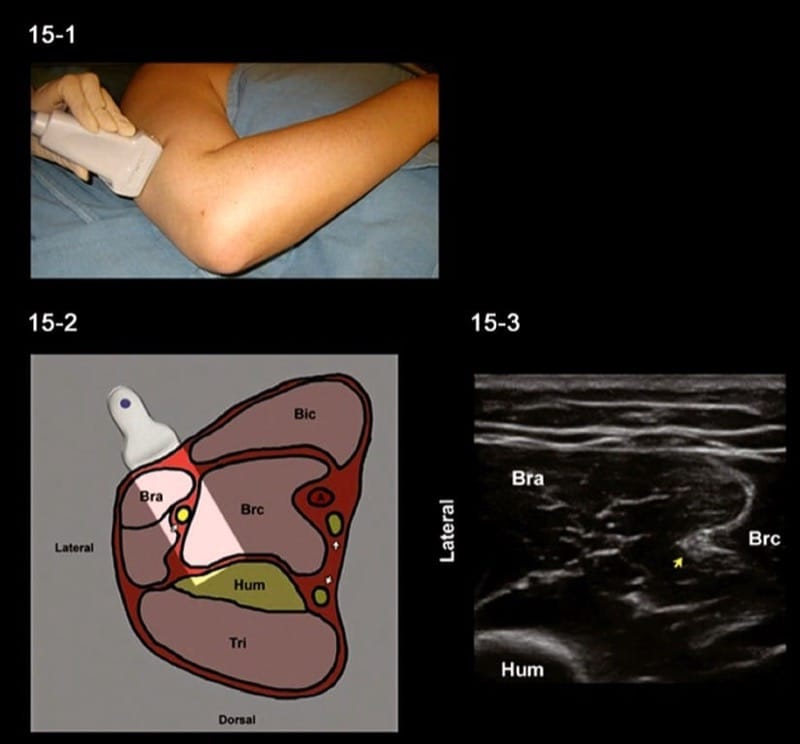
Fig.15 Radial nerve block in the distal arm. (1) Ultrasound probe placement. (2) Anatomical structures within the ultrasound transducer range. (3) Ultrasound image of the radial nerve (arrowhead) in the distal arm. BA brachial artery, BM biceps muscle, Bra brachioradialis muscle, Brc brachialis muscle, Hum humerus, Tri triceps muscle
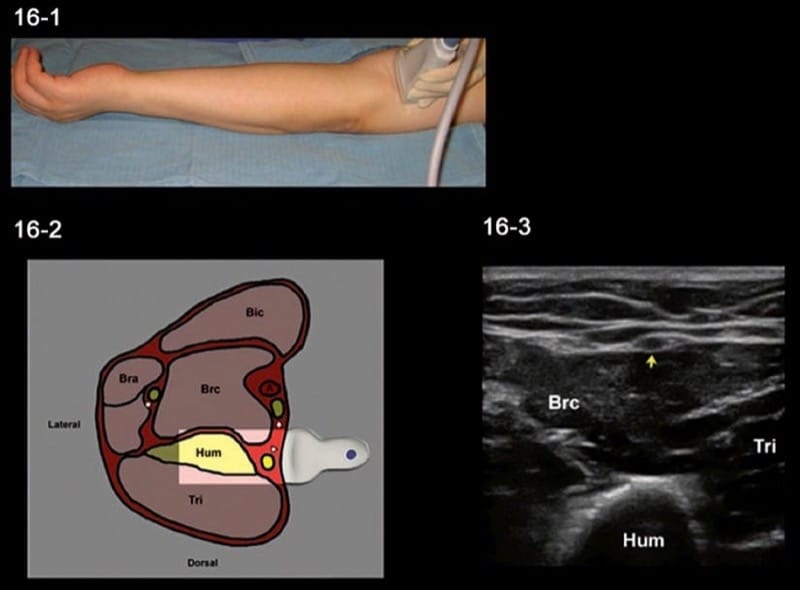
Fig.16 Ulnar nerve block in the distal arm. (1) Ultrasound probe placement. (2) Anatomical structures within the ultrasound transducer range. (3) Ultrasound image of the ulnar nerve (arrowhead) in the distal arm. BA brachial artery, BM biceps muscle, Bra brachioradialis muscle, Brc brachialis muscle, Hum humerus, Tri triceps muscle
7. SUMMARY
This course has outlined some common approaches of ultrasound-guided blocks of the brachial plexus and its terminal nerves. Ultrasound-guided regional anesthesia is a rapidly evolving field. Recent advances in ultrasound technology have enhanced the resolution of portable equipment and improved the image quality of neural structures and the regional anatomy relevant to peripheral nerve block. The ability to image the anatomy in real-time, guide a block needle under image, and tailor local anesthetic spread is a unique advantage of ultrasound imaging over traditional techniques, and comparative studies increasingly suggest advantages in terms of both efficacy and safety.