Intra-articular knee injections as well as other peripheral joint injections have been successfully utilized for several decades [1]. Knee injections may be completed for both diagnostic and therapeutic goals. More recently, in 1997 exogenous high molecular weight hyaluronan viscosupplementation was approved to treat knee osteoarthritis in the United States by the FDA.
1. LIMITATIONS OF THE CURRENT SURFACE LANDMARKS TECHNIQUE
Incorrect placement of hyaluronic acid may lead to increased pain and reduced therapeutic effect [2]. Unlike corticosteroids, hyaluronic acid has little effect if injected in periarticular tissue [3]. While injecting multiple joints and using contrast with follow-up radiographs to determine their accuracy, Jones et al demonstrated that 66% knee joint injections were intra-articular, and almost a third of the injections were extra-articular [4]. In a study designed to measure the accuracy of intra-articular knee joint injections, Jackson et al demonstrated that blind injections through the lateral midpatellar portal were most accurate 93% of the time, while the anterior medial and anterior lateral approaches were only accurate 75% and 71%, respectively [5]. To date there is only one article evaluating the accuracy of ultrasound-guided intra-articular knee injections. Im et al reported 96% accuracy with US guidance vs. 77% accuracy with blind injections [6].
2. TECHNIQUE FOR ULTRASOUND-GUIDED KNEE JOINT INJECTION
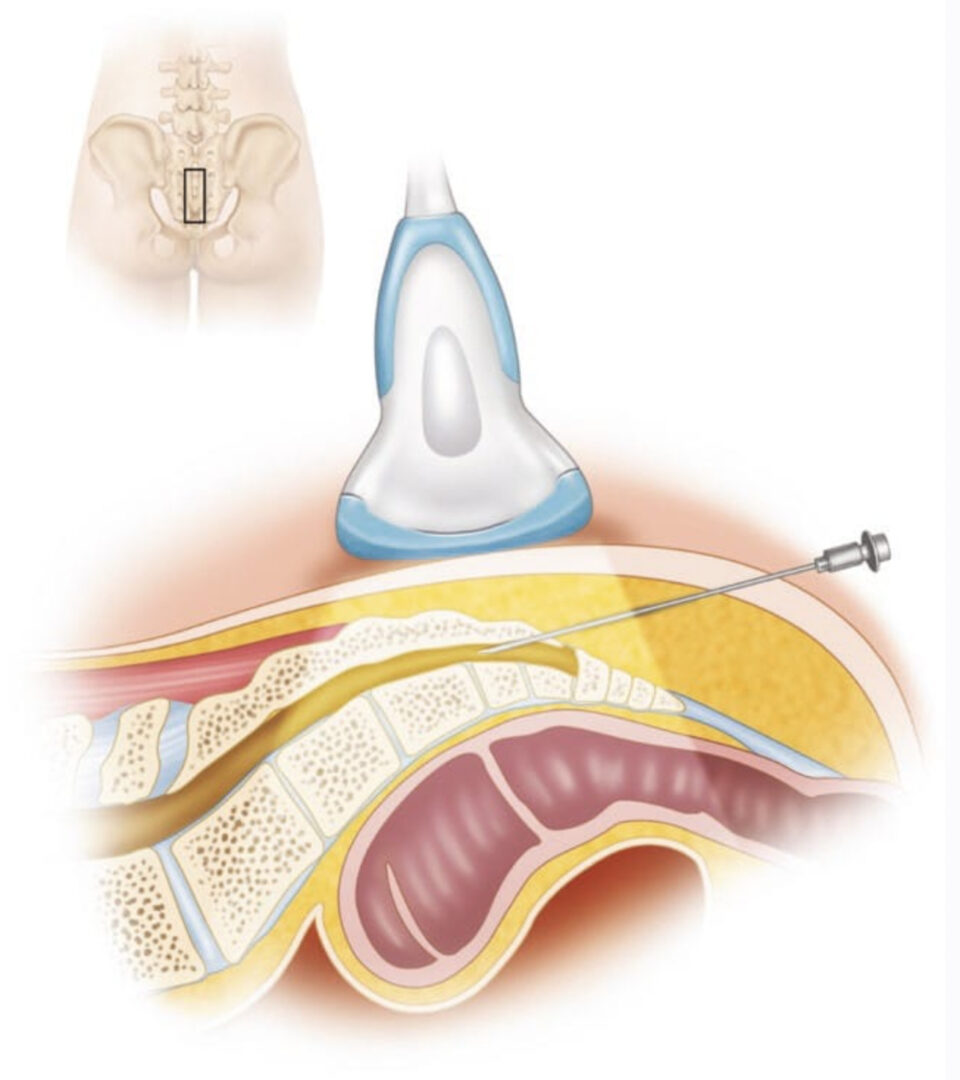
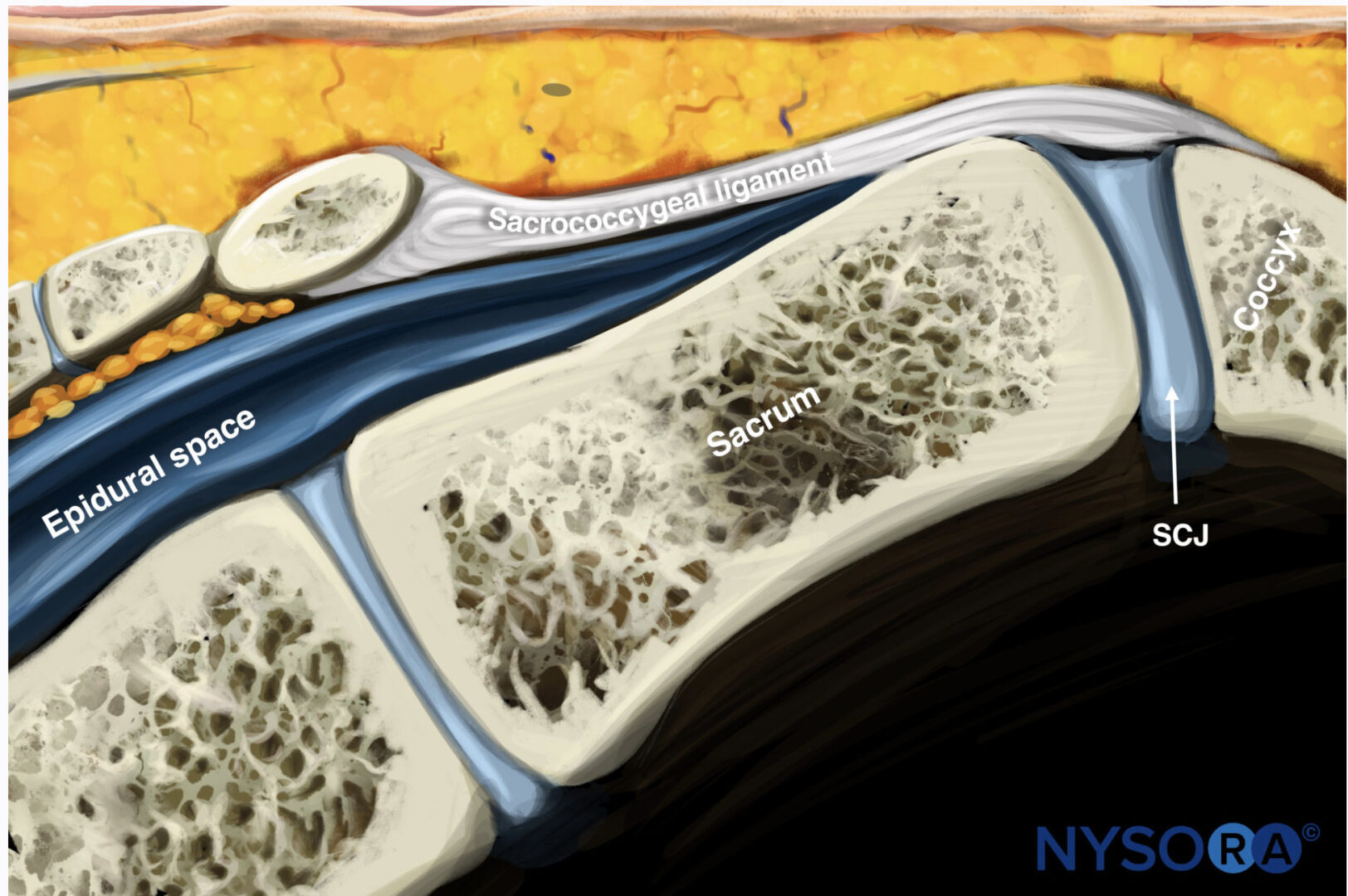
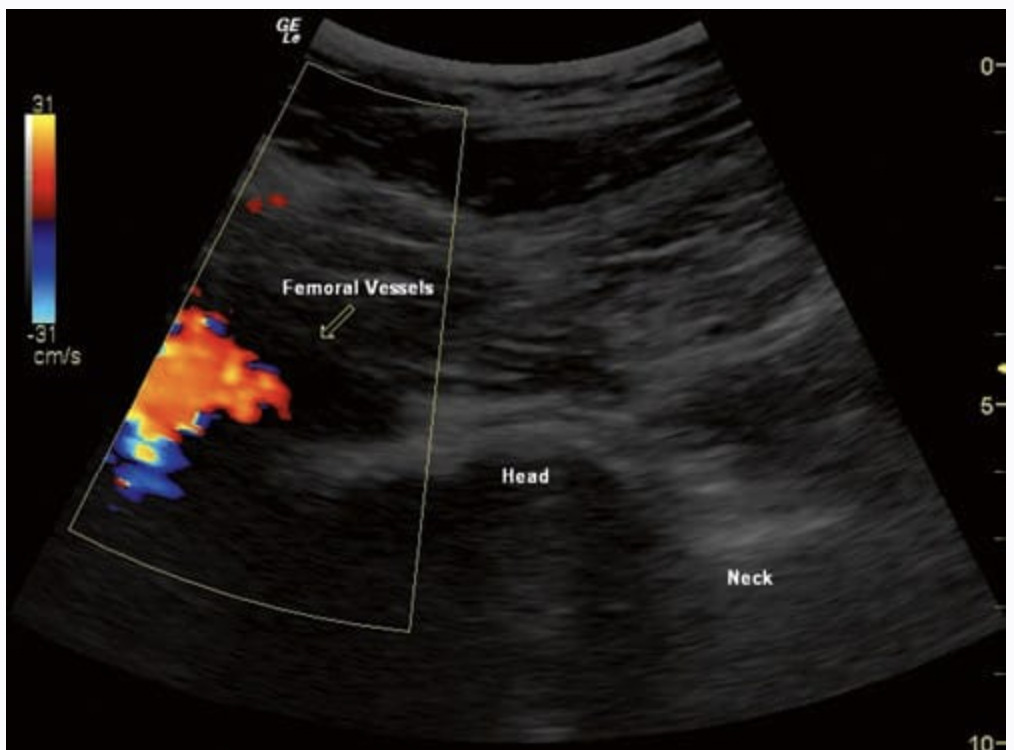
The patient is placed in the supine position with a pillow or support under the knee so the joint is flexed roughly 30°. A high-frequency linear probe is utilized to scan the suprapatellar and lateral pouches for an effusion (Figs. 1, 2, 3, 4, 5, 6, and 7). If an effusion is localized, this hypoechoic fluid collection becomes the target for the aspiration and injection. Typically, a subclinical effusion can be visualized under the quadriceps tendon just proximal to the patella. These effusions can be visualized by placing a linear probe on the patella in the transverse position and gently sliding proximally until the quadriceps tendon is visualized (Fig. 1). By avoiding excessive sonopalpation (compression), subtle effusions can be visualized without blotting out the capsular fluid. Deep to the quadriceps tendon between the quadriceps fat pad and prefemoral fat pad, the collapsed joint recess or joint effusion can be visualized in the short axis by turning the probe 90° (Fig. 2). The probe is kept in the transverse plane while the skin lateral to the probe is palpated (Fig. 6). Based on this tissue movement with palpation lateral to the probe under US visualization, a needle pathway is predetermined to avoid having to stick a needle through the quadriceps tendon. This area is then marked and prepped in a sterile fashion. Drapes are then applied. To minimize pain, a 25–27-gauge needle is used to administer lidocaine subcutaneously. Next, a 22- or 25-gauge needle is advanced into the joint recess or effusion.
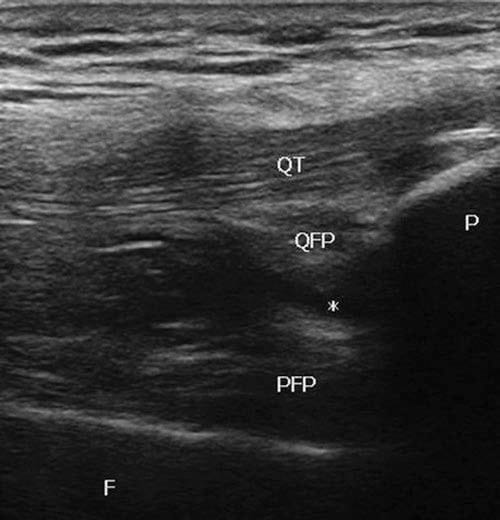
Fig.1 Long-axis view of the proximal anterior knee with a sub-clinical effusion (asterisk). QT quadriceps tendon, P patella, QFP quadriceps fat pad, PFP prefemoral fat pad, F femur
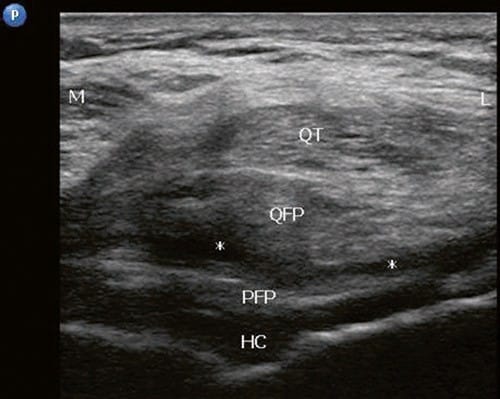
Fig.2 Short-axis view of the proximal anterior knee with a sub-clinical effusion (asterisks) in the suprapatellar pouch. QT quadriceps tendon, P patella, QFP quadriceps fat pad, PFP prefemoral fat pad, HC hypoechoic hyaline cartilage
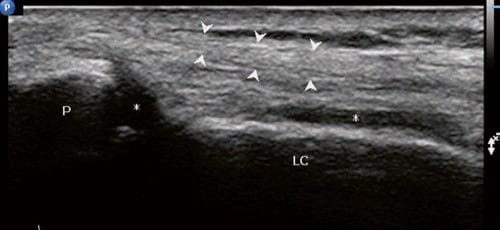
Fig.3 Transverse view on the lateral side of the patella. Arrowheads lateral patellar retinaculum, P patella, LC lateral femoral condyle, asterisks collapsed joint space

Fig.4 Transverse view of the lateral pouch with a well-defined effusion
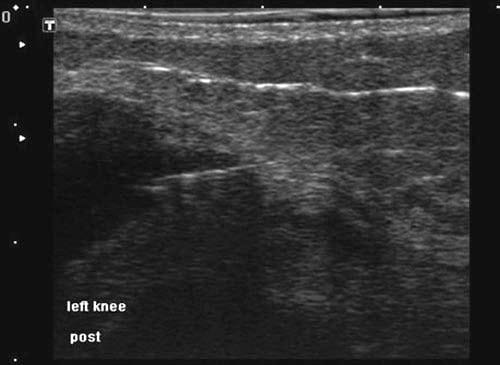
Fig.5 Transverse view of lateral patella and a needle placed in the medial portion of the lateral pouch

Fig.6 Short-axis approach to the suprapatellar pouch from lateral to medial
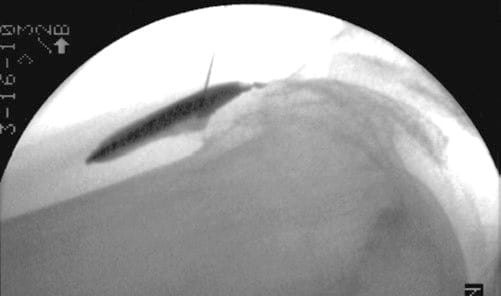
Fig.7 Fluoroscopic confirmation of suprapatellar pouch approach under US guidance
A test dose containing 1–2 ml of local anesthetic can be utilized to confirm proper intrasynovial needle tip placement. Fluoroscopic confirmation can also be obtained with a lateral view of the knee joint (Fig. 7). There should be minimal resistance while 2–6 ml of viscosupplementation or corticosteroid is injected. A medial patellar approach was also described with the knee fully extended [6] (Figs. 8 and 9).
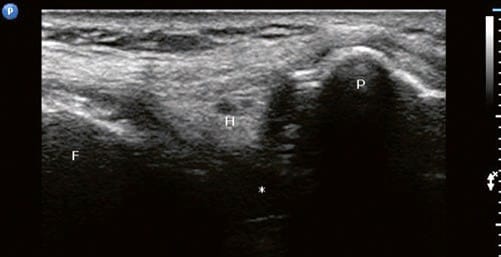
Fig.8 Transverse view of mid-medial patella. Site of the medial patellar portal approach described by Im. F femur, H Hoffa’s fat pad, P patella, asterisk joint space
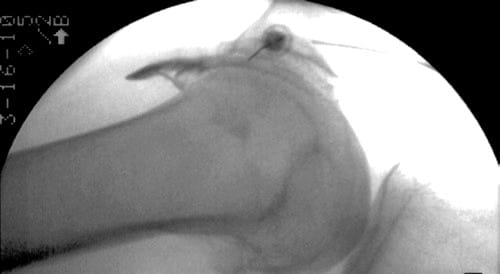
Fig.9 Fluoroscopically confirmed patellofemoral approach with contrast flowing freely between the patella and femur
3. CONCLUSION
In conclusion, blind knee injections are relatively accurate in skilled hands. However, guided injections should be seriously considered when a definitive diagnosis is needed, synovial fluid is required, biologic material with regenerative qualities is injected or viscosupplementation is utilized.