Stellate ganglion block (SGB) is performed for the management of patients for a variety of pain conditions, including complex regional pain syndrome and peripheral vascular disease [1, 2]. The most widely practiced approach to SGB is the paratracheal approach, in which the needle is inserted toward the anterior tubercle of the cervical sixth vertebra (Chassaignac tubercle) [3]. This approach is essentially a block of the cervical sympathetic chain in proximity to the middle cervical ganglion instead of the stellate ganglion, which is located opposite to the neck of the first rib [4]. Thus, the classical approach is better termed cervical sympathetic block.
1. ANATOMY
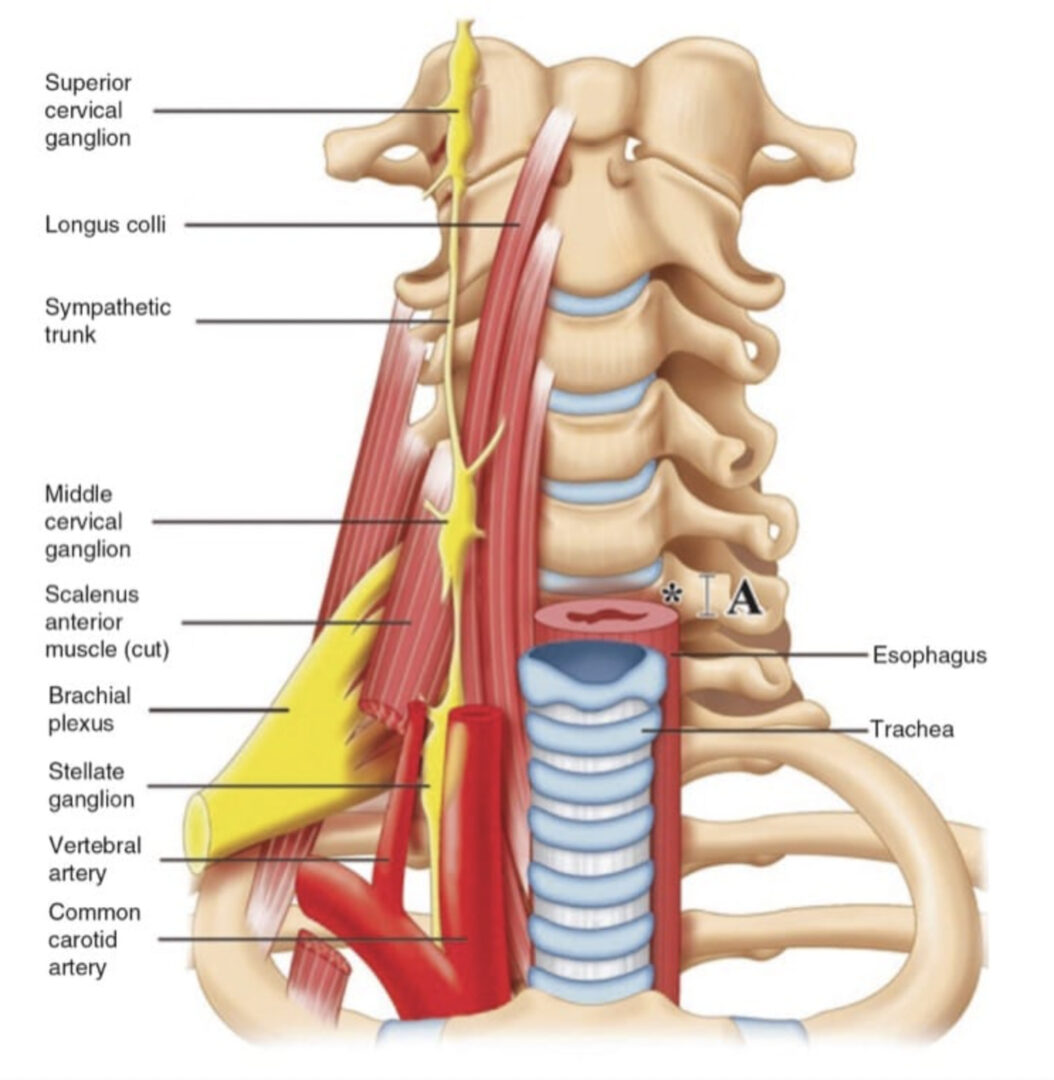
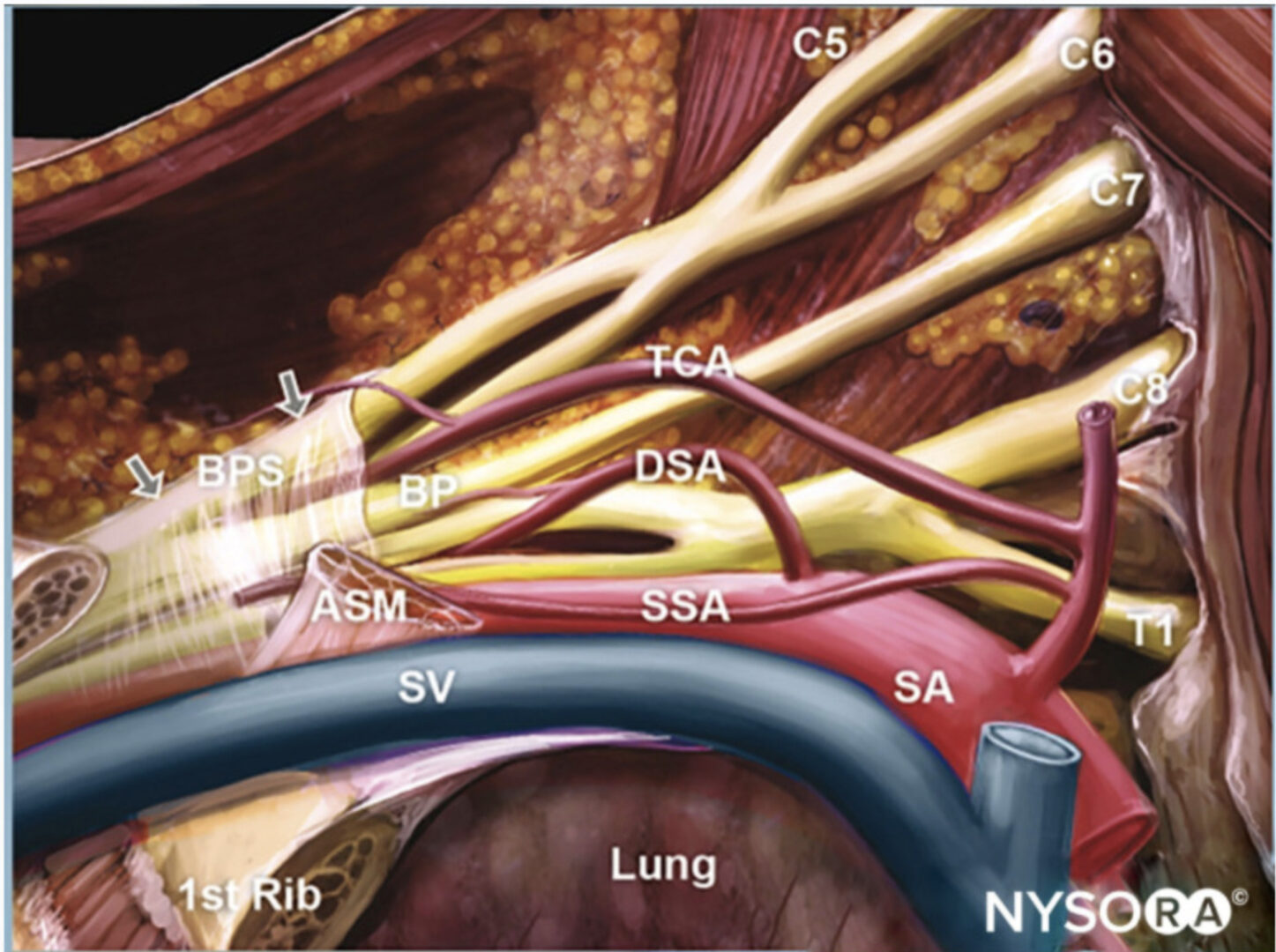
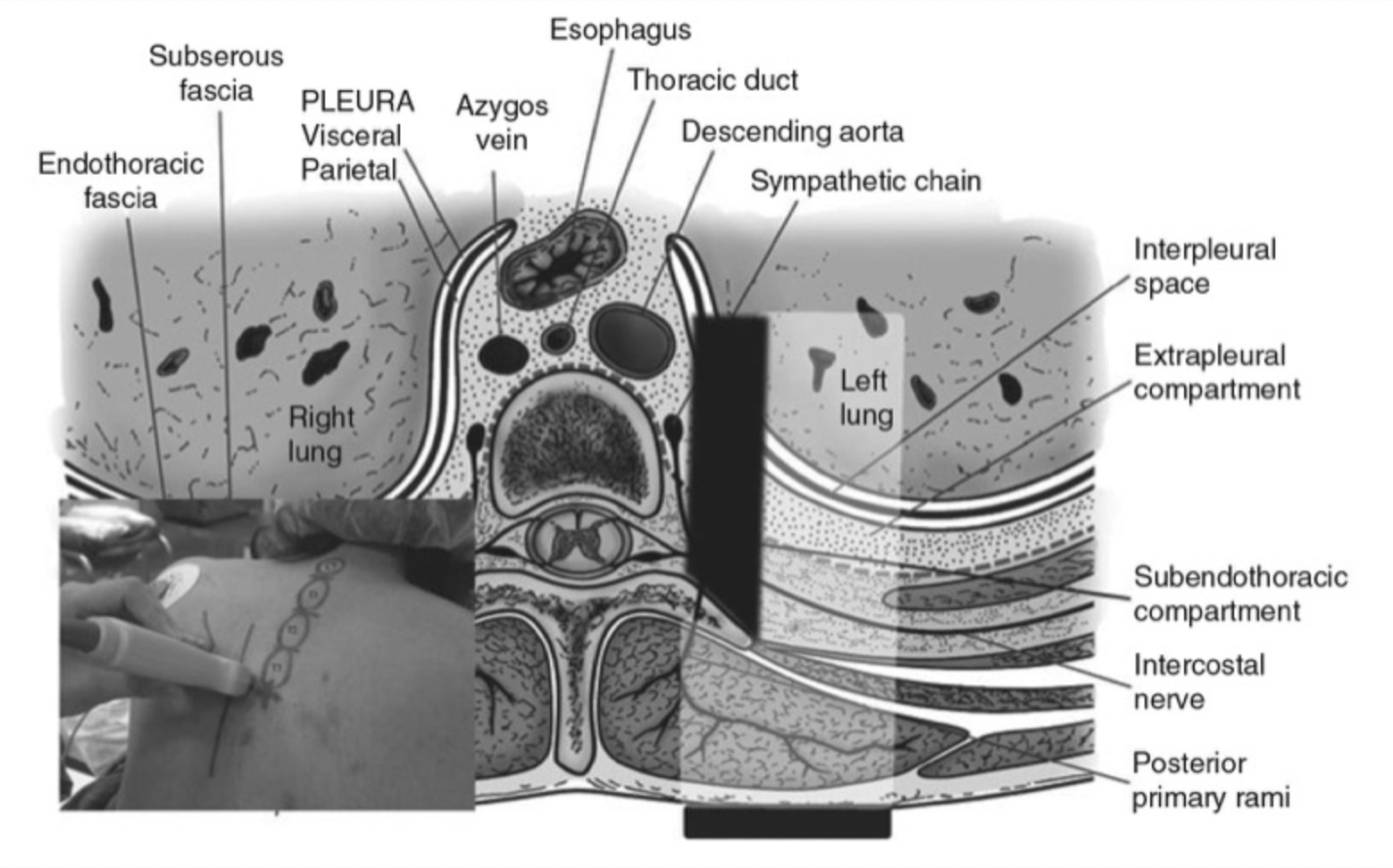
The sympathetic outflow arises from the preganglionic neurons located at the lateral gray horn of the spinal cord at the thoracic and upper two lumbar spinal segments. The sympathetic fibers for the head, neck, upper limbs, and heart arise from the first few thoracic segments, ascend through the sympathetic chains, and synapse in the superior, middle, and inferior cervical ganglion [4, 5]. The stellate ganglion, formed by fusion of the inferior cervical and first thoracic ganglion, extends from the level of the head of the first rib to the inferior border of the transverse process of C7 and lies medial or sometimes posterior to the vertebral artery immediately adjacent to the dome of pleura (Fig. 1).
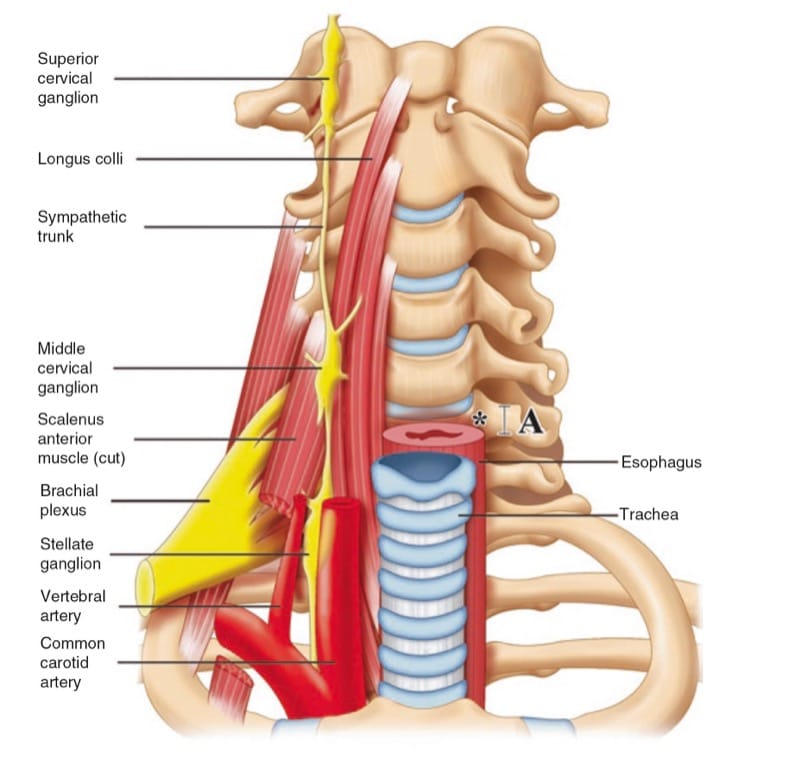
Fig. 1 Prevertebral region of the neck. The target site for needle insertion in classical approach is marked as asterisk. The breadth of the trans-verse process is marked as A. (Reproduced with permission from USRA (www.usra.ca))
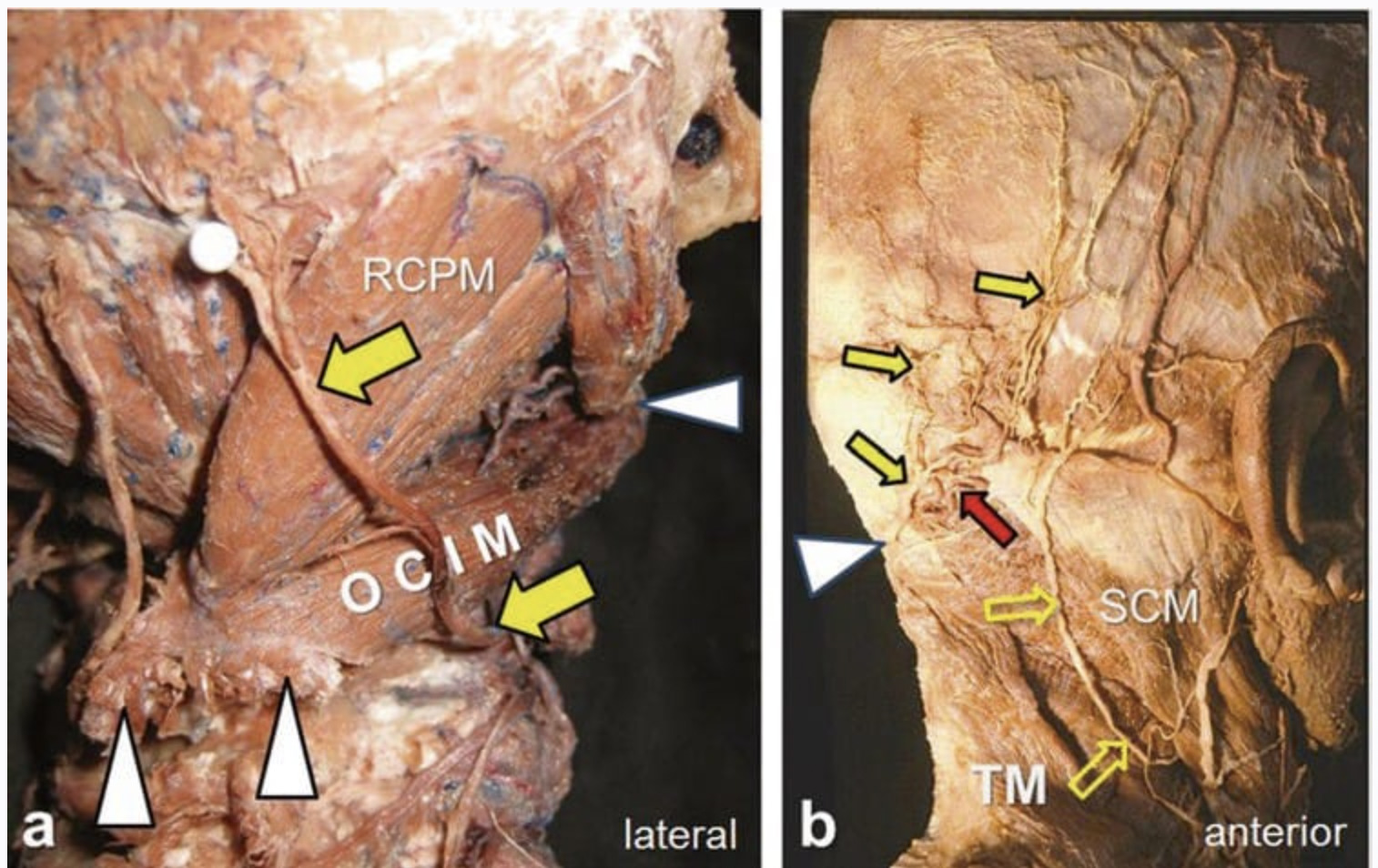
The postganglionic fibers from the stellate ganglion to the cervical nerves (seventh and eighth) and the first thoracic nerve provide sympathetic innervation to the upper limbs [4–7]. The preganglionic fibers of the head and neck region continue to travel cephalad to the superior and middle cervical ganglion through the cervical sympathetic trunk (CST). Injection of local anesthetic around the stellate ganglion interrupts the sympathetic outflow to the head, neck, and upper limbs through inactivation of both preganglionic and postganglionic fibers, while injection of local anesthetic around the CST results only in sympathetic block of the head and neck regions [5, 6]. The CST is located dorsal to the posterior fascia of the carotid sheath anteriorly and is embedded in the prevertebral fascia (personal communication Dr. E Civelek) [8–10].
2. EXISTING TECHNIQUES
As stated above, the popular approach is anterior paratracheal approach at sixth cervical vertebral level with or without fluoroscopic guidance because of the close relation of the stellate ganglion to the pleura and vertebral artery. These indirect approaches to CST assume that the medication will spread caudally to the stellate ganglion. A few concerns about these approaches are examined below.
The breadth (cephalocaudal distance) of the Chassaignac tubercle can be as narrow as 6 mm [3]. Thus, it can be easily missed with needle advancement with conventional technique. A consequence of this is potential puncture of the vertebral artery or nerve root, which is usually protected by the anterior tubercle of the C6. However, once the needle is in contact with the bone, the vertebral artery can still be at risk. The vertebral artery usually ascends and enters the foramen in the transverse process of C6 vertebra. Unfortunately, a cadaver study demonstrated that this arrangement applied in 90–93% of the cadavers examined and the vertebral artery may enter at the transverse process of C4 or C5 [11, 12]. Although contrast injection in fluoroscopy-guided technique helps to avoid inadvertent injection of local anesthetic into this artery, the intravascular injection can be recognized only after the artery has been punctured. A modified fluoroscopy-guided oblique approach may minimize the risk of vertebral artery puncture as the needle is directed to the junction of the uncinate process and the vertebra body [13]. However, this technique directs the needle much closer to the esophagus (see below).
Both landmark-based technique and fluoroscopy-guided technique do not reveal the soft tissues transverse by the needle path [14]. In most of the anatomy atlas, the esophagus is often seen as a structure located behind the cricoid and trachea. However, the literature contradicts those assumptions. Esophagus is found deviated from the midline in 53% of the subjects [15]. In 5% of the subjects, approximately 40–60% of the esophagus is unopposed by the cricoid and lies ventral to the medial part of the transverse process, which is part of the needle path (Fig. 2) [15]. Mediastinitis can result especially if the patient has an unrecognized diverticulum [16]. Moreover, this probably is the cause of the “foreign body” sensation that is often attributed in the past to the block of external laryngeal branch of superior laryngeal nerve or recurrent laryngeal nerve [17].
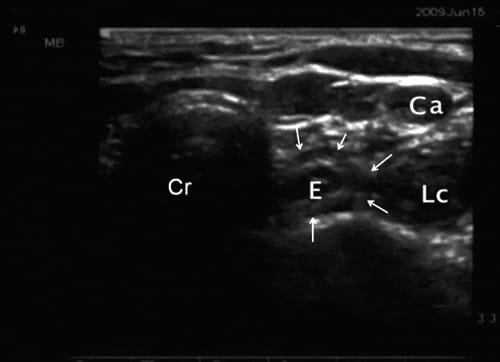
Fig.2 Ultrasonographic image of the neck at C6 showing the devi-ation of esophagus (outlined by line arrows). Cr cricoid, LC longus colli muscle, E esophagus, CA carotid artery. (Reproduced with permission from USRA (www.usra.ca))
Certain artery, especially inferior thyroidal artery, can be seen passing in the needle path (Fig. 3) [18]. Another artery that can be found anterior to transverse process of C6 or C7 is the ascending cervical artery, which has been described to form an anastomosis with either vertebral artery or anterior spinal artery [19]. The major consequence of not recognizing this variation will be the formation of hematoma [20, 21]. As a matter of fact, hematoma was fairly commonly encountered (25%) in the first case series comparing ultrasound-guided with “blind” injection technique [22]. The consequence of larger hematoma can be life-threatening, as demonstrated by a review of those patients with retropharyngeal hematoma following SGB [23].
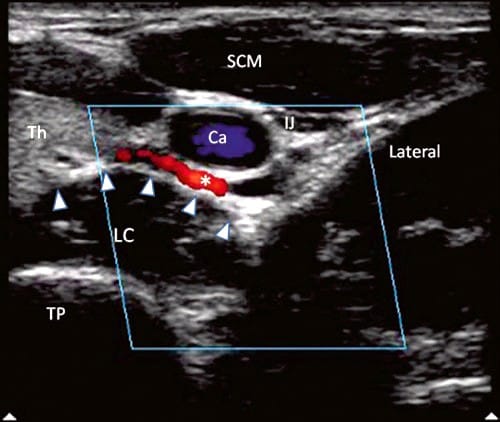
Fig.3 Ultrasonographic image with color Doppler. The inferior thyroidal artery was indicated with asterisk; the prevertebral fascia is marked by solid arrowheads. TP transverse process of C6, Th thyroid, LC longus colli muscle, IJ internal jugular vein. (Reproduced with per-mission from USRA (www.usra.ca))
The key to the success of the block of CST is to deposit the local anesthetic around the CST with caudal spread of the local anesthetic to the stellate ganglion. The location of CST is in the prevertebral fascia which is a loose connective tissue. Without reference to this key anatomy landmark, both the landmark-based and fluoroscopy-guided techniques rely on the surrogate landmark, C6 or C7 transverse process, as the target. The technique involves directing the needle to the bone and withdrawing the needle. The spread of solution following “bone contact and needle withdrawal” has been studied and the injectate spread anterior to the prevertebral fascia and in the paratracheal space in most of the patients, without much caudal spread [24]. It has been suggested that subfascial injection results in more caudal spread, higher rate of sympathetic block of upper limb, and lower risk of hoarseness [25, 26]. Too deep an injection into the longus colli muscle also renders the sympathetic block ineffective [27]. Given the anatomical position of the CST, the ideal location is into prevertebral fascia.
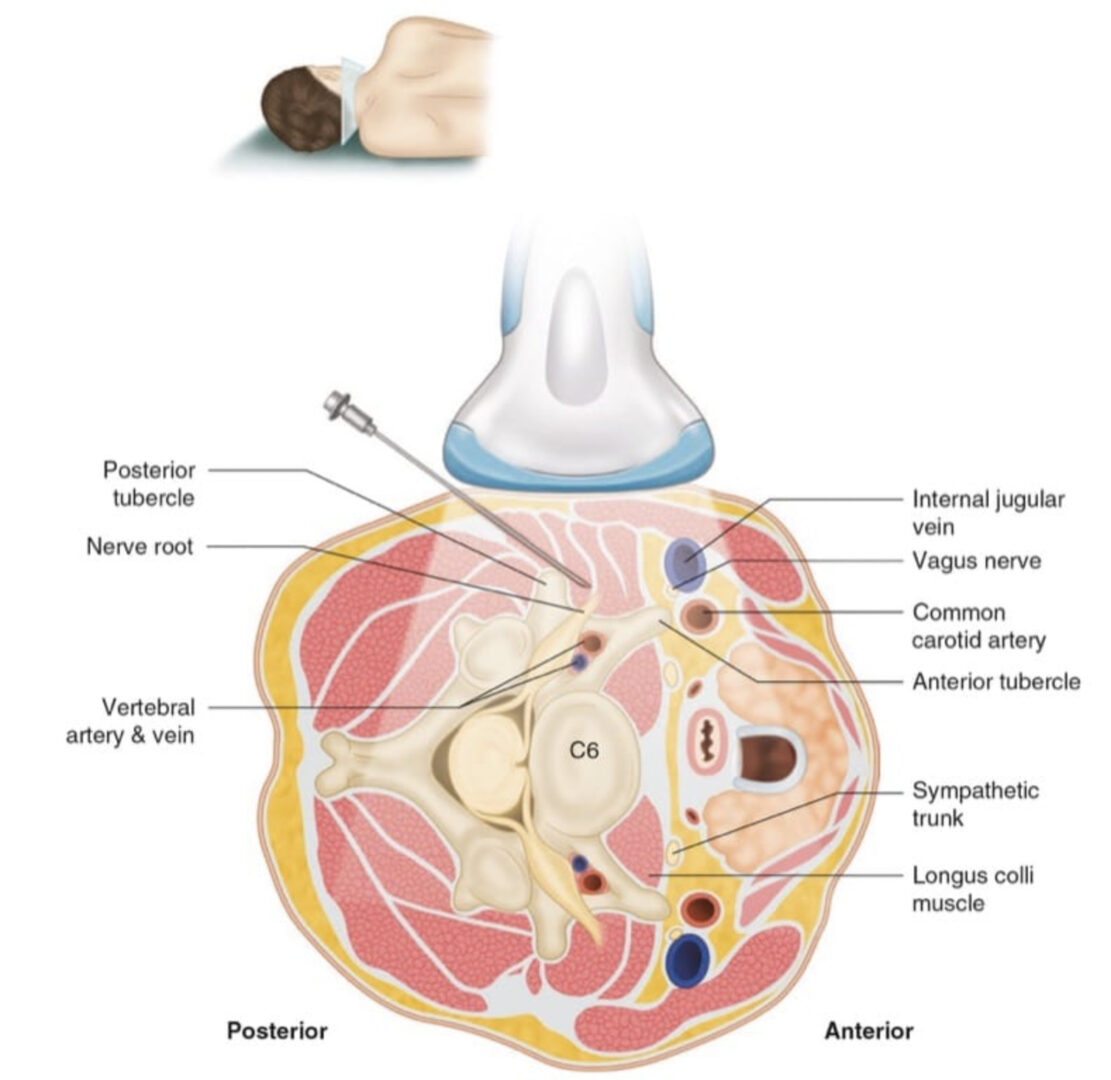
3. TECHNIQUE FOR ULTRASOUND-GUIDED INJECTION
The patient is placed in the supine position with the neck in slight extension. A high-frequency linear transducer (6–13 MHz) is placed at the level of C6 to allow cross-sectional visualization of anatomic structures, including the transverse process and anterior tubercle of C6, longus colli muscle and prevertebral fascia, and carotid artery and thyroid gland (Figs. 4 and 5) [14, 17]. A prescan is important in planning the path of needle insertion as the presence of the esophagus and the inferior thyroidal artery may obviate the needle insertion path between the carotid artery and trachea [28]. In that situation, the needle may be inserted lateral to the carotid artery, which is the author’s preferred route.
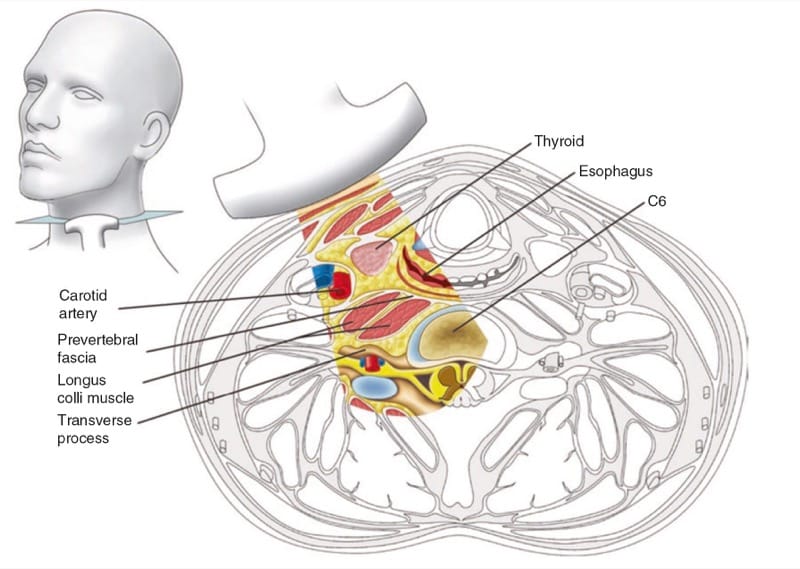
Fig.4 Cross section of the neck at the sixth cervical vertebral level correlating with the ultrasonographic image. (Reproduced with permission from USRA (www.usra.ca))
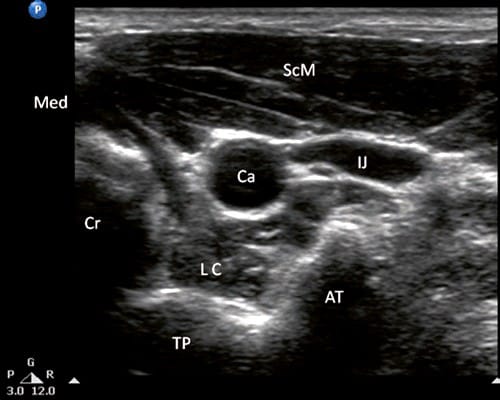
Fig.5 Ultrasonographic image of the neck at C6. SCM sternoclei-domastoid muscle, CA carotid artery, TP transverse process of C6, AT anterior tubercle, LC longus colli muscle, IJ internal jugular vein, Cr cricoids, Med medial. (Reproduced with permission from USRA (www. usra.ca))
For the lateral approach, the tip of the needle is directed to the prevertebral fascia between the carotid artery and the tip of C6 anterior tubercle (Fig. 1.6). This needle path will avoid hitting the cervical nerve root. The internal jugular vein can be visualized by decreasing the probe pressure and avoided by “pushing” away with the needle. A total of 5 ml of local anesthetic is injected. Visualization of the spread of injectate under real-time scanning is important, as the absence of this may suggest unsuspected intravascular injection.
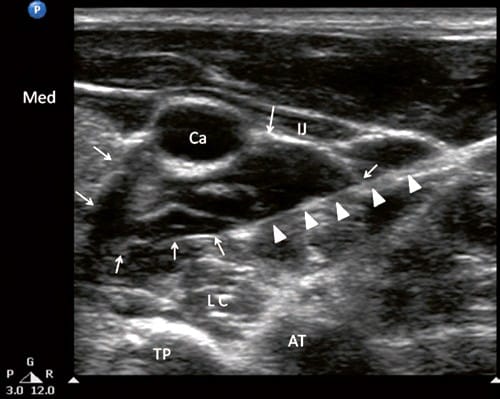
Fig.6 Ultrasonographic image of the neck at C6 as in Fig.5 following injection of local anesthetic. The needle was indicated by solid arrows and the local anesthetic was outlined by the line arrows. Ca carotid artery, IJ internal jugular vein, LC longus colli muscle, TP transverse process, AT anterior tubercle. (Reproduced with permission from USRA (www.usra.ca))