Anatomy The sacroiliac joint (SIJ) is a true diarthrodial joint with the articular surfaces of the sacrum and ilium separated by a joint space enclosed in a fibrous capsule [1]. It bears the characteristics of a synovial joint, especially in the superoanterior and inferior aspects. The superoposterior joint surface lacks a joint capsule and contains the interosseous ligament. The anterior joint capsule gives origin to the anterior sacroiliac ligament. The posterior aspect also contains the posterior sacroiliac, sacrotuberous, and sacrospinous ligaments that stabilize the joint. With increasing age, degenerative changes occur with narrowing of the synovial cleft inferiorly and subsequent fibrous ankylosis [2, 3]. The muscular and fascial support of the SIJ is derived from the gluteus maximus and medius, the erector spinae, the latissimus dorsi and thoracolumbar fascia, the biceps femoris, the piriformis and oblique muscles, and the transversus abdominis. The gluteus maximus, biceps, and piriformis attach to the sacrotuberous ligament while the thoracodorsal fascia connects to the remaining muscle groups. The anteroposterior and superoinferior wedgeshaped sacrum (forming a keystone configuration) and this extensive muscular support account for reduced mobility but high stability of the SIJ [2–5]. The posterior SIJ is predominantly innervated by lateral branches of the L4-S2 nerve roots with contributions from S3 and the superior gluteal nerve. The anterior SIJ innervation is from the L2-S2 segments [6, 7]. The synovial capsule and ligaments contain free nerve endings as well as mechanoreceptors that transmit proprioceptive and pain sensation from the joint [3].
1. INDICATIONS FOR SIJ INJECTION
Diagnostic SIJ injections are used to identify pain stemming from the SIJ. Most provocative tests for diagnosing SIJ pain are not definitive, and SIJ injections remain the gold standard. There are also no imaging studies that consistently provide findings to diagnose the SIJ as the source of pain.
Therapeutic SIJ injection is used after failure of conservative treatment, including anti-inflammatory medications and physical therapy.
2. LITERATURE REVIEW ON ULTRASOUND-GUIDED SIJ INJECTION
Pekkafahli and colleagues [8] studied the feasibility of ultrasound-guided SIJ injections and reported a 76.7% overall success rate (n = 60), with a steep learning curve. The success rate improved from 60% with the first 30 injections to 93.5% with the next 30 injections.
Klauser and coworkers [9] assessed the feasibility of ultrasound-guided SIJ injection in ten human cadavers bilaterally at two different puncture sites. The upper level was defined at the level of the first posterior sacral foramen and the lower level at the level of the second posterior sacral foramen. Then the injection was attempted in ten patients with unilateral sacroiliitis. Computed tomography confirmed correct intra-articular needle placement in cadavers by showing the tip of the needle in the joint and intra-articular diffusion of contrast media in 80% of cases (upper level 70%; lower level 90%). In patients, 100% of ultrasound-guided injections were successful (eight lower levels, two upper levels).
Perry and associates [10] studied the accuracy of ultrasound-guided SIJ injections using a cadaveric model. Seventeen SI joints were injected under ultrasound guidance and dissected to determine the accuracy of intra-articular injections. Ultrasound allowed intra-articular injection in 88.2% of joints in this cadaveric study. In addition, ultrasound allowed visualization of extra-articular spread when caused by extra-articular needle placement, which can allow for redirection of the needle to achieve intra-articular injection.
Soneji and coworkers [11] compared fluoroscopy and ultrasound guidance for SIJ injection in 40 patients with chronic low back pain secondary to SIJ arthritis. The patients were randomized to receive ultrasound- or fluoroscopyguided unilateral SIJ injections. The authors concluded that ultrasound-guided SIJ injection with fluoroscopic confirmation is similar in accuracy and efficacy to fluoroscopy alone for SIJ injections in patients with chronic low back pain secondary to SIJ arthritis.
3. TECHNIQUE OF ULTRASOUND-GUIDED SIJ INJECTION
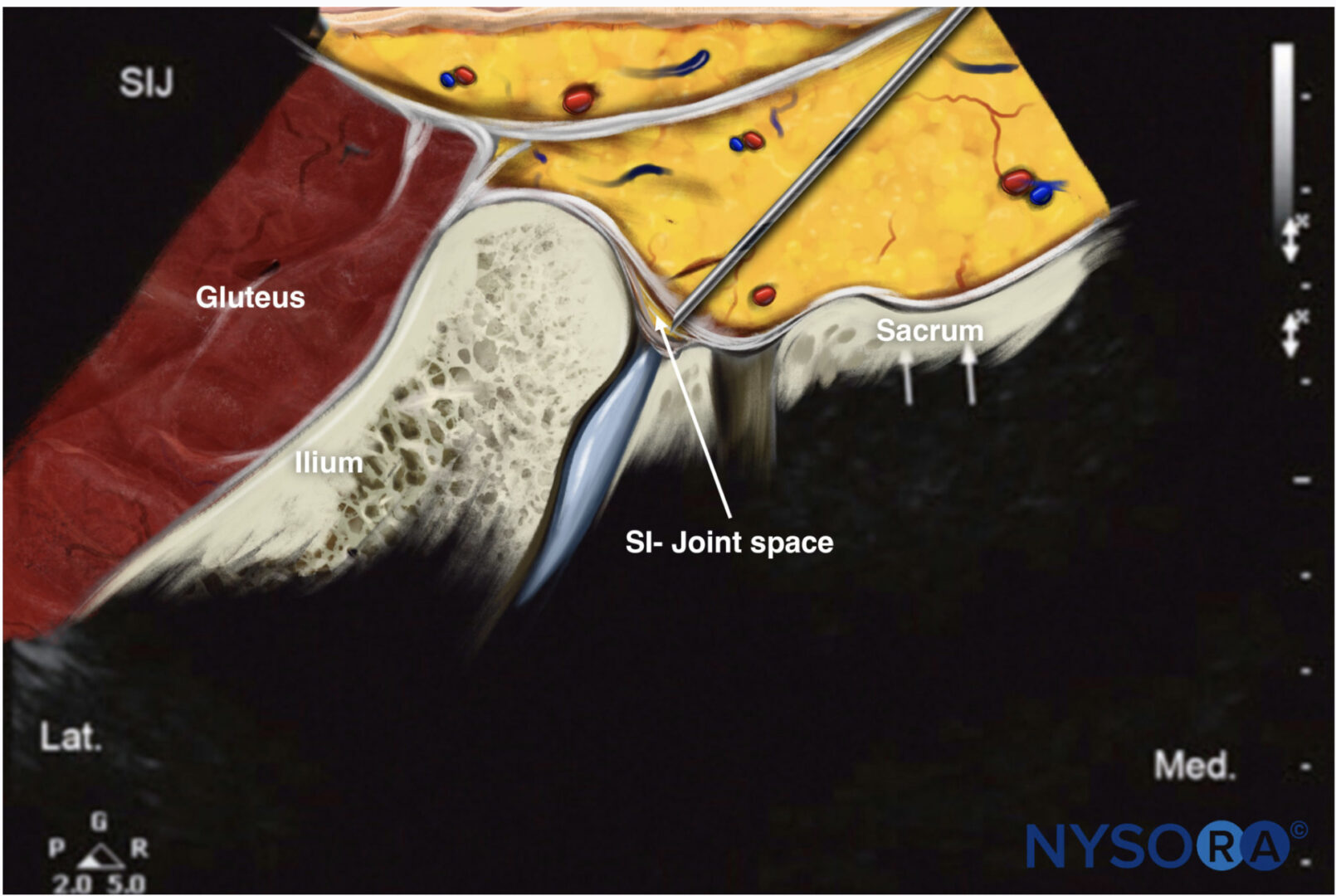
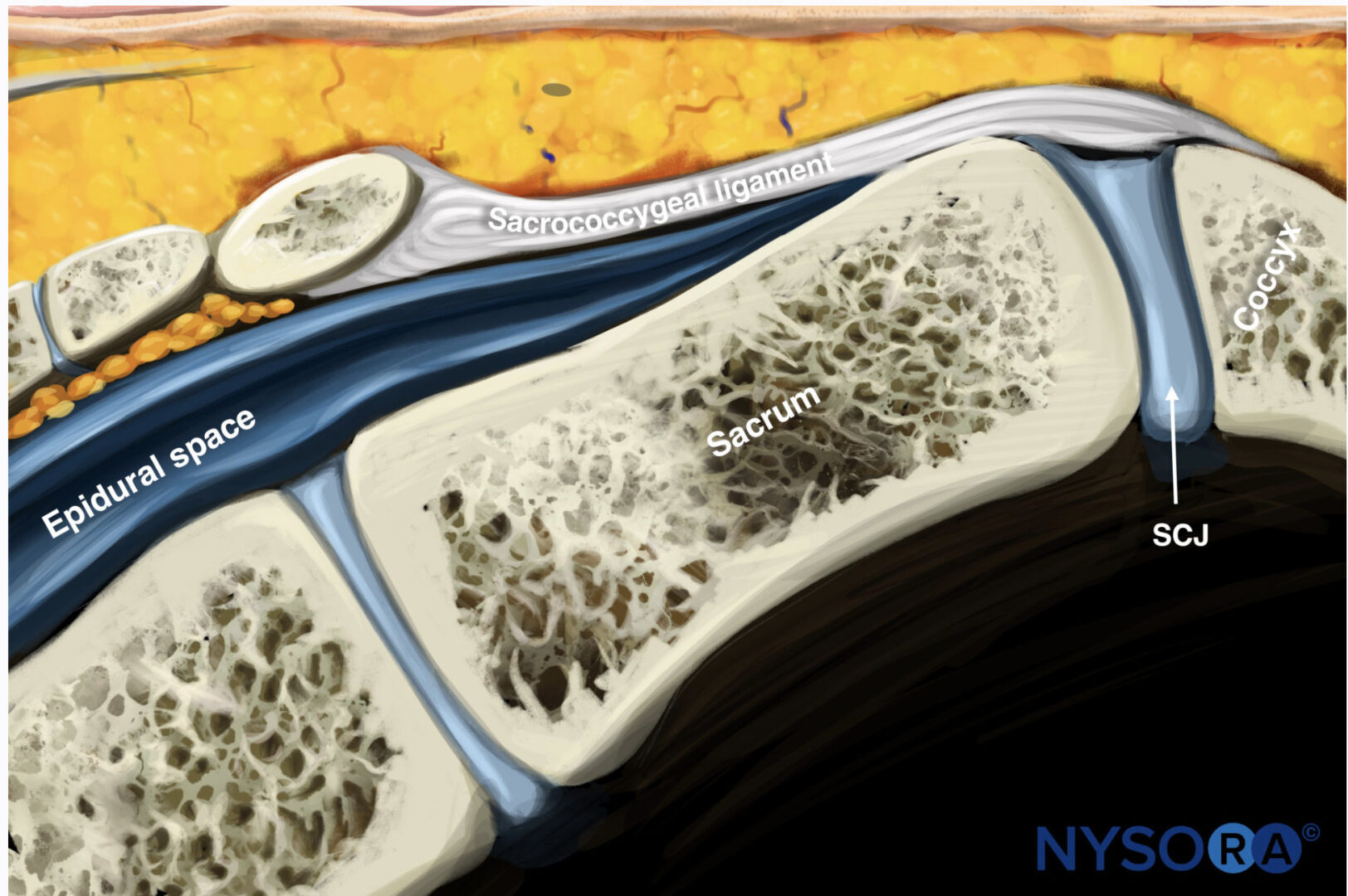
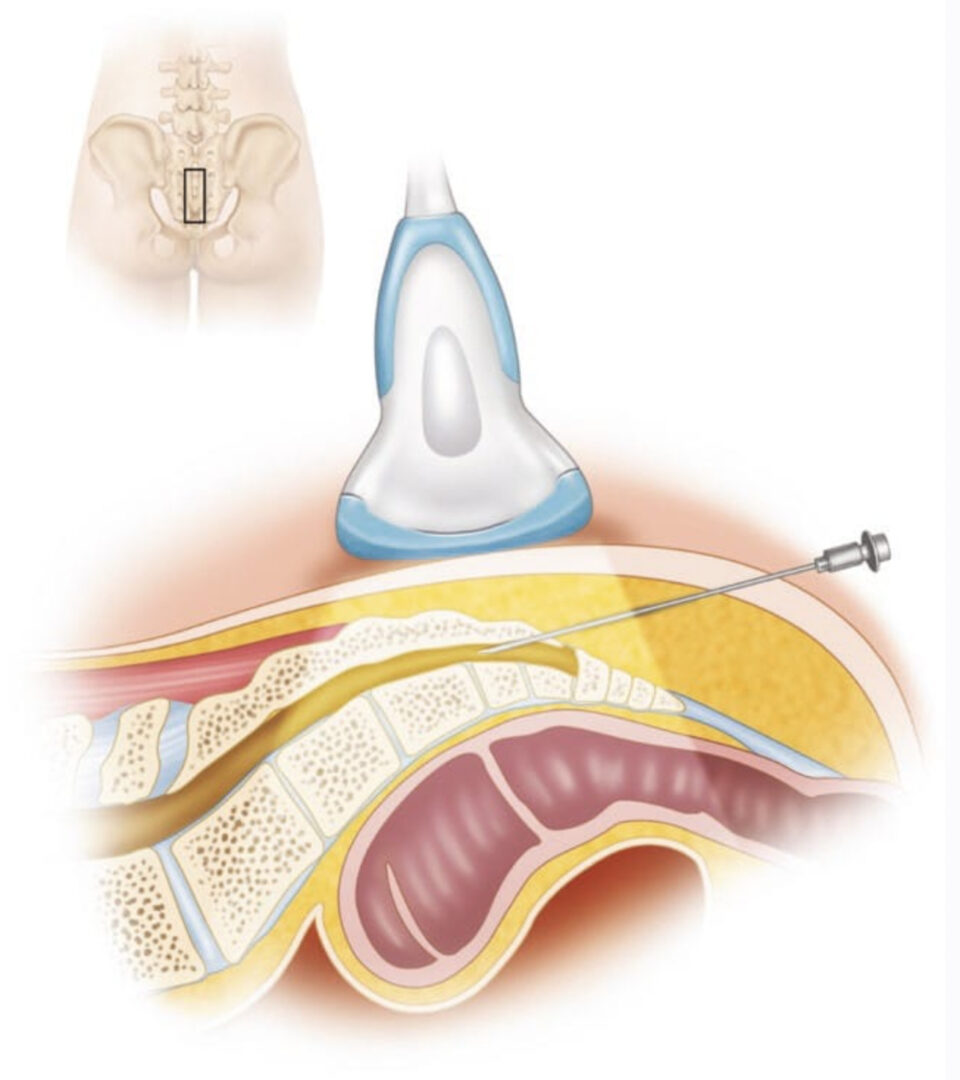
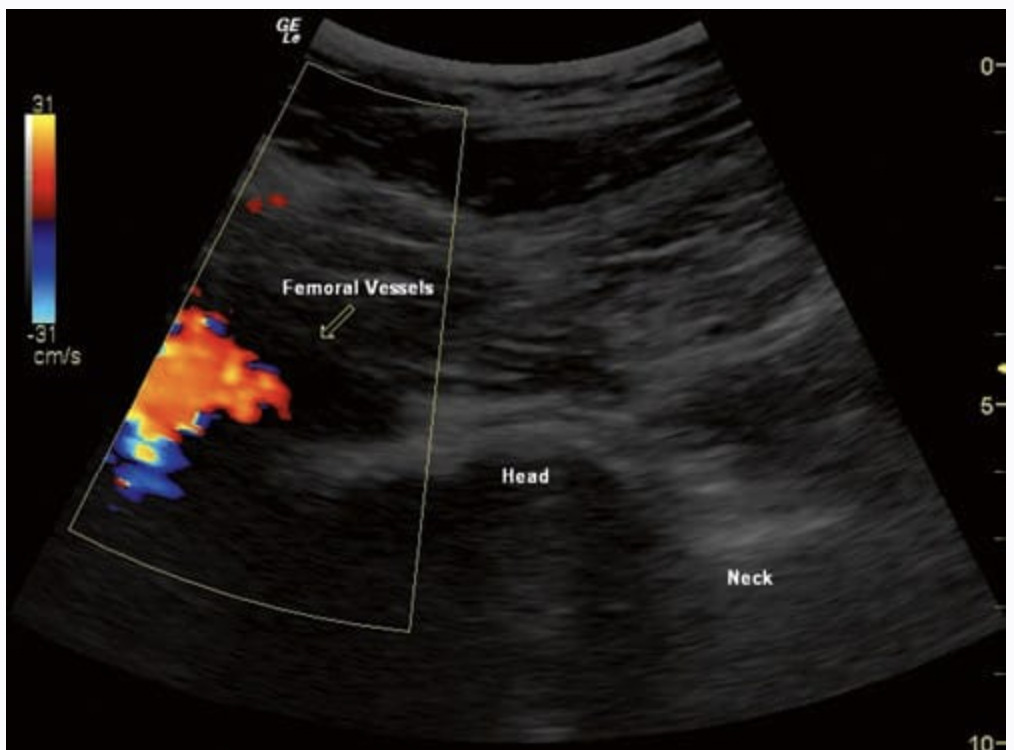
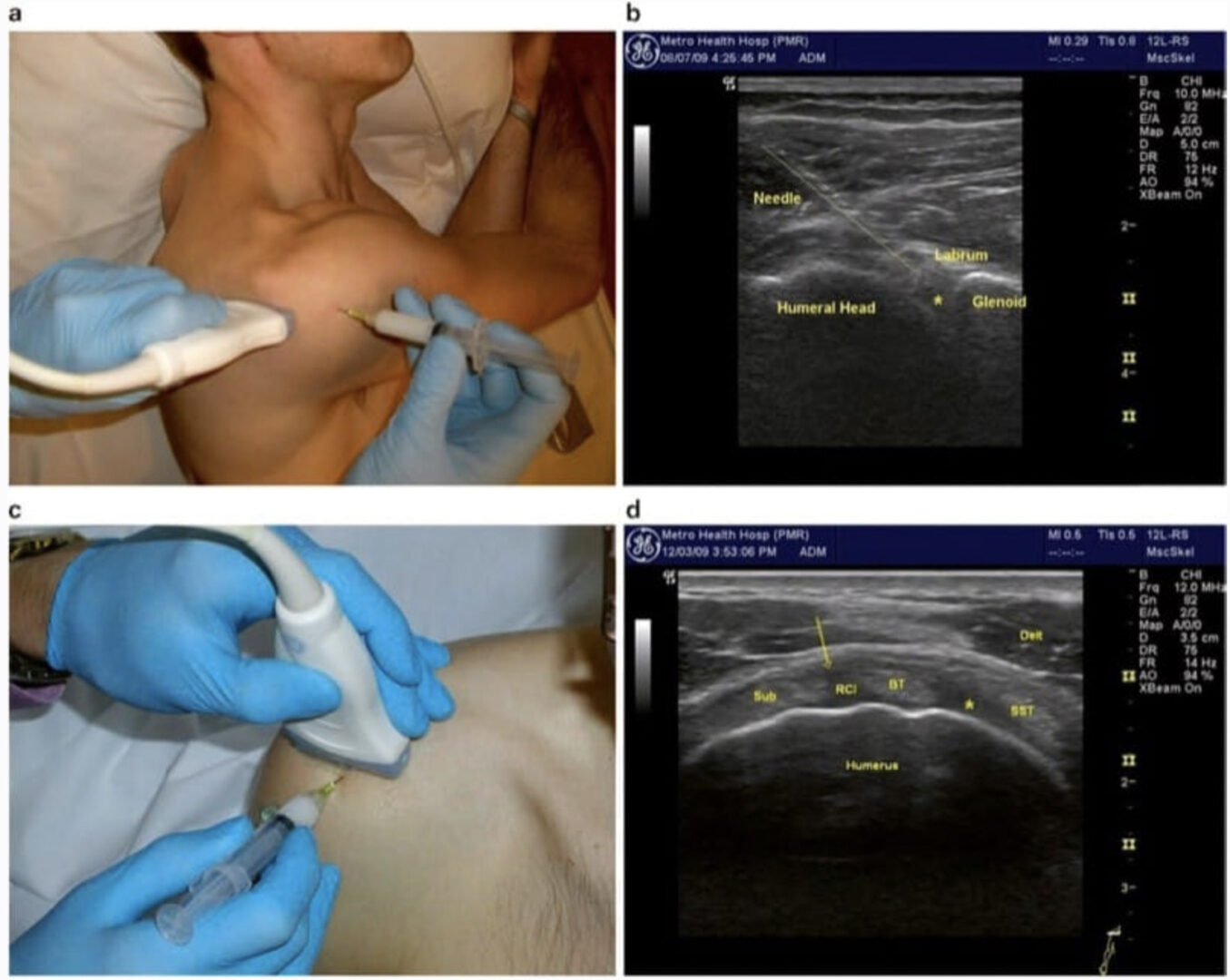
The patient is placed in the prone position with a pillow underneath the abdomen to minimize lumbar lordosis. Usually, a low-frequency curvilinear transducer is used, especially in obese patients to increase penetration. The transducer is placed transversely over the lower part of the sacrum (at the level of the sacral hiatus), and the lateral edge of the sacrum is identified. Then the transducer is moved laterally and cephalad till the bony contour of the ileum is clearly identified (Fig. 1). The cleft seen between the medial border of the ileum and the lateral sacral edge represents the SI joint, and the inferior-most point is targeted [12]. A 22-gauge needle is then inserted at the medial end of the transducer and advanced laterally under direct vision in plane with the ultrasound beam until it is seen entering the joint (Fig. 2)
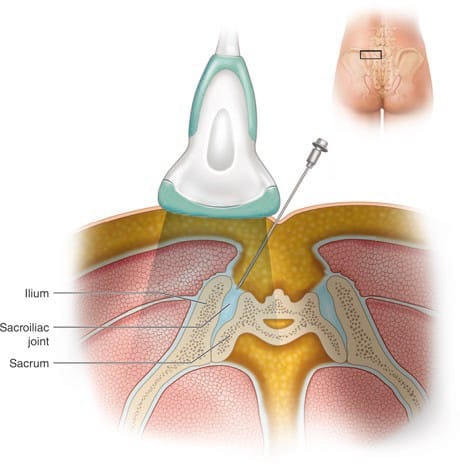
Fig.1 The placement of the ultrasound probe over the sacroiliac joint (SIJ) to obtain a short axis view is shown

Fig.2 Short-axis sonogram showing the needle (in-plane) inside the SIJ (arrowheads). The dotted lines outline the bony surface of the ilium and the arrows point at the dorsal surface of the sacrum
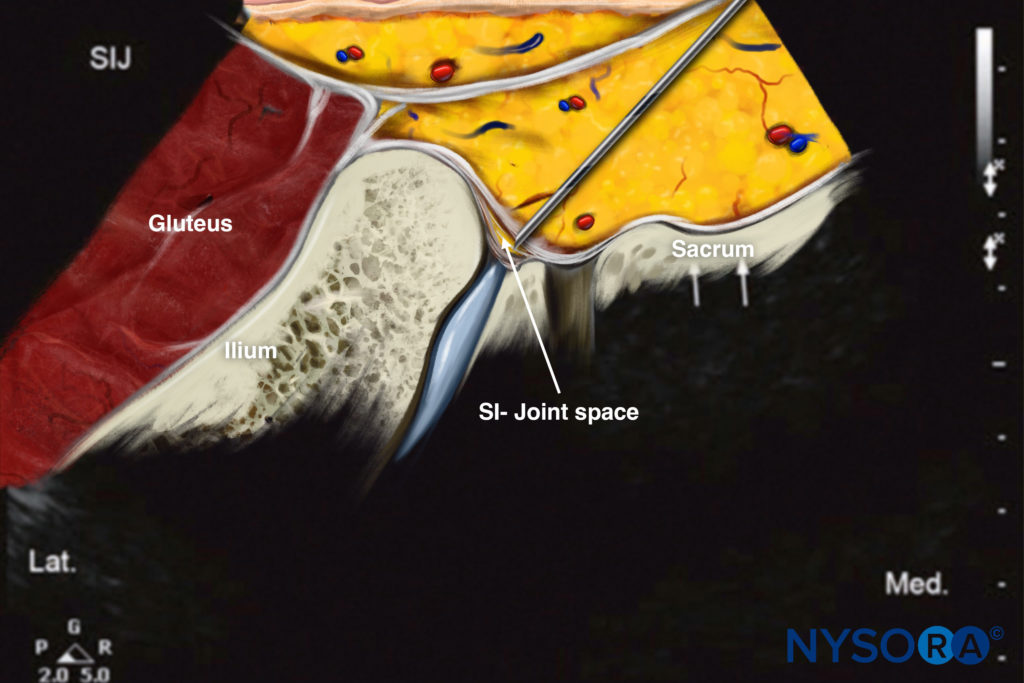
Reverse Ultrasound Anatomy illustration of figure 2. SIJ, sacroiliac joint.
4. LIMITATIONS OF ULTRASOUND-GUIDED SIJ INJECTION
The potential for periarticular rather than intra-articular injection may be increased compared to fluoroscopic or CT-guided SIJ injections because an arthrogram with contrast agent injection can be reliably obtained in most cases with the latter technique. Also, ultrasound is not very reliable in detecting intravascular injection while performing SIJ injections (Fig. 3).
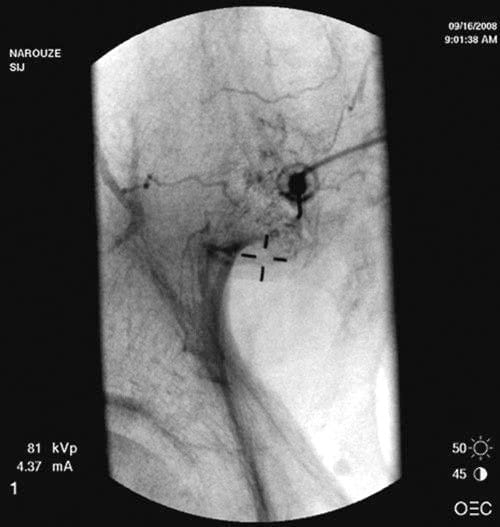
Fig.3 Anteroposterior radiograph showing intravascular spread of the contrast agent during SIJ injection. (Reprinted with permission from Ohio Pain and Headache Institute)