Hip pain is caused by many conditions, including osteoarthritis (OA), rheumatoid arthritis, and acetabular labral tears. Incidence of hip OA is expected to increase over time with the aging population and with the increase in obesity in the United States. Overall, 14.3% of US adults aged 60 years and older reported significant hip pain on most days over the previous 6 weeks [1]. Management options for pain in the hip include analgesics, including nonsteroidal antiinflammatory agents, intra-articular steroids, and viscosupplementation and hip replacement for advanced stages [2]. Intra-articular injections are performed based on landmarks or using fluoroscopy, CT, and ultrasound imaging [2–8]. This chapter discusses the various imaging methods, their advantages and disadvantages, and finally the technique for ultrasound-guided intra-articular hip injections.
1. ANATOMY OF THE HIP JOINT
The hip joint is a synovial joint that permits movement in all directions because of the “ball and socket” configuration of the femoral head and the acetabulum. The depth of the acetabular cavity is enhanced by the fibrocartilaginous labrum that lines the rim. The ligamentum teres femoris attaches the center of the femoral head to the acetabulum and hence is intra-articular. The capsule has various thickenings formed by the longitudinally oriented iliofemoral, ischiofemoral, and pubofemoral extracapsular ligaments.
The femoral neurovascular bundle is separated from the hip joint by the iliopsoas. It is located in the femoral triangle formed by the sartorius laterally, the adductor longus medially, and the inguinal ligament superiorly. The femoral artery gives off the deep femoral artery, which divides into the medial and lateral circumflex arteries supplying the femoral head and neck. The posterior division of the obturator artery also contributes a major branch traversing the ligamentum teres and supplying the femoral head.
Branches from the femoral, obturator, and sciatic nerves provide articular branches to the hip joint.
2. INTRA-ARTICULAR HIP INJECTIONS
Some of the commonly adopted methods of providing temporary pain relief in hip joint pain are the injection of local anesthetics, steroids, and viscosupplementation. Intraarticular injection of local anesthetics facilitates the identification of the source of pain [9, 10]. Precision in the injection contributes significantly to its diagnostic value. Intraarticular steroid injections decrease pain and inflammation [11]. Robinson et al. compared two different doses of steroids with fluoroscopic guidance in 120 patients and found that there is a dose response to the effectiveness of intraarticular steroid injections in increasing range of motion and pain relief [12]. Viscosupplementation is injecting hyaluronate into the joints to improve lubrication and relieve pain; it thus may delay joint replacement [13]. Although extensively studied for knee joints, there are few reports on the use of hip joint viscosupplementation. Two randomized controlled studies on the use of viscosupplementation did not find any benefit in hip OA [14, 15]. A retrospective study by Park et al. compared intra-articular ketorolac versus corticosteroid injection for hip OA and noted comparable outcomes at 6 months [16].
3. LIMITATIONS OF THE BLIND TECHNIQUE
Because the hip joint is deeply located, blind landmark-based injections suffer from a lack of accuracy, in addition to the possibility of damage to neurovascular structures in proximity to the joint. With the anterior approach, the needle is very close to the femoral nerve and may sometimes impale the nerve. The reported success rate with landmark-based injections varies from 50% to 80% depending on the technique and the practitioner. Leopold et al. placed needles into the hip joints of cadavers based on landmarks and found that the needle passed within 4.5 mm of the femoral nerve with an anterior approach and 58.9 mm with the lateral approach [3].
This risk begs for the use of image guidance for intraarticular hip injections. Utilizing fluoroscopy or CT guidance for the performance of these injections entails cost considerations as well as radiation exposure to both the patient and the practitioner [6, 7]. In addition, although fluoroscopy is extensively used for intra-articular injections, it does not permit visualization of the neurovascular bundle.
4. EVIDENCE FOR ULTRASOUND-GUIDED HIP INJECTIONS
Experimentation with the use of ultrasound led to its use in diagnostic musculoskeletal imaging and naturally transitioned to needle guidance. Ultrasound machines are portable, relatively inexpensive, have no known major bioeffects in humans, and permit delineation of soft tissue structures besides bone. Sonography has been shown to be useful in diagnosing various pathologies, including arthritis, soft tissue masses, effusion, and labral tears, besides facilitating joint aspiration of effusions [17, 18].
Hoeber et al. conducted the first systematic review and meta-analysis that revealed significantly higher accuracy for ultrasound-guided hip injections compared with a blind technique [19]. The accuracy of ultrasound-guided hip injections reported in multiple studies is between 97% and 100% [20–23]. Another smaller study also attests to the effectiveness of ultrasound guidance for intra-articular hip injections [23]. In addition, Pourbagher et al. confirmed intra-articular hip hyaluronate injection under ultrasound guidance with postinjection CT verification [22].
Fluoroscopy has been the standard for intra-articular hip injections, but when Byrd et al. compared it with ultrasound guidance, they reported higher patient convenience scores with the use of ultrasound and patient preference for ultrasound-guided injections [24].
Along with effectiveness, ultrasound guidance for hip injections provides additional safety measures. Sofka et al. conducted a retrospective review of 358 adult hip ultrasound-guided aspirations/injections and found no cases of inadvertent vascular or femoral nerve puncture [25]. Similarly, Berman et al. reported no major complications in 800 successful sonographically guided hip injections [26].
5. TECHNIQUE OF ULTRASOUND-GUIDED HIP INJECTIONS
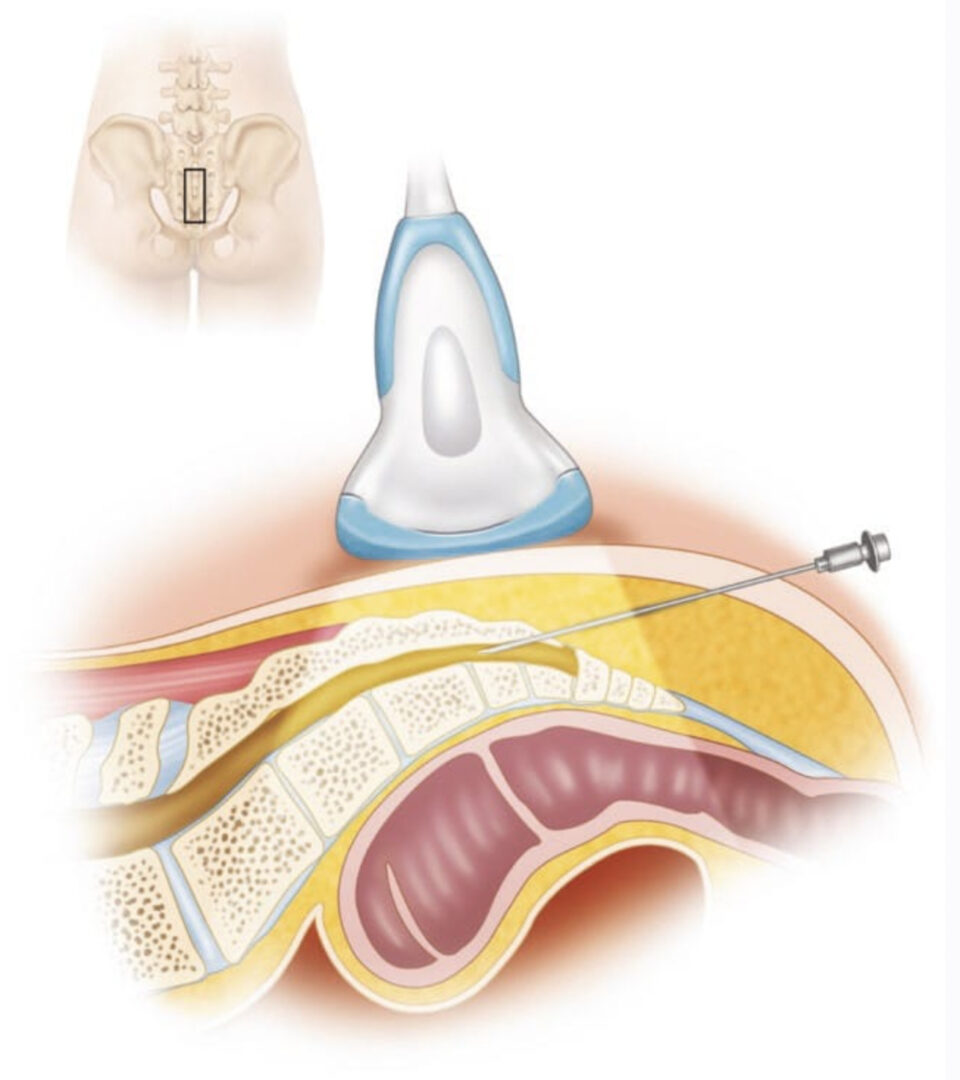
The authors prefer the anterior sagittal approach. The patient is positioned supine, with the hip maintained in the neutral position; a pillow beneath the knee may provide some comfort and relax the joint.
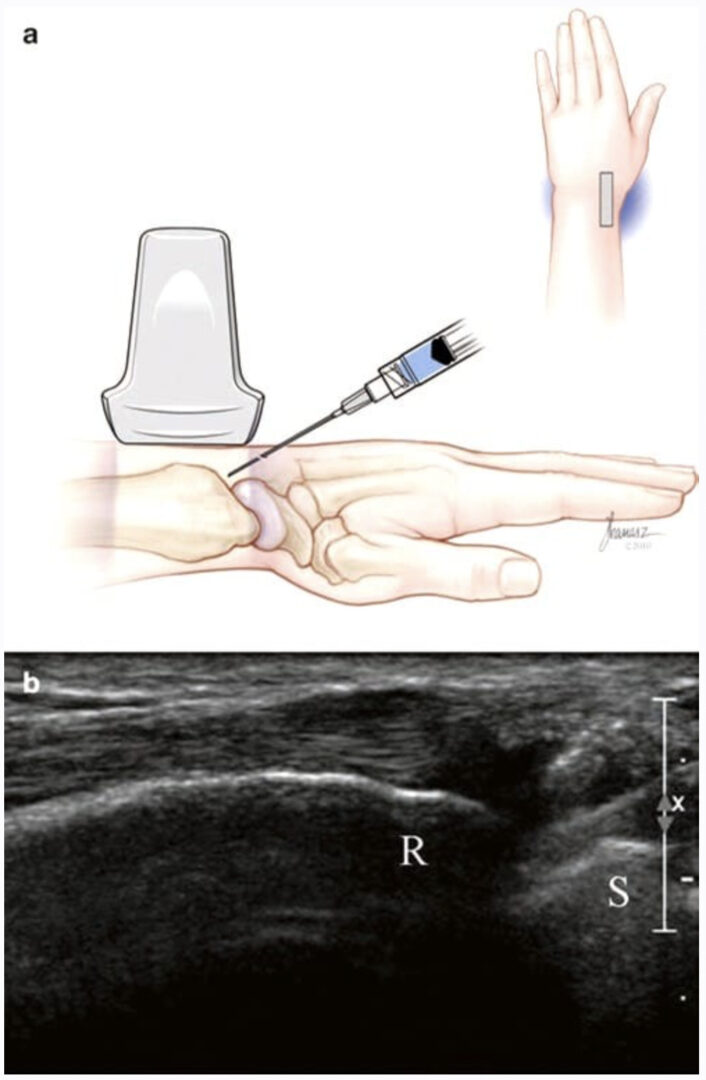
A curved array transducer is typically used. In patients with a smaller body habitus, a linear array transducer with higher frequencies may provide better resolution. The frequency is adjusted for the depth of penetration required to visualize the femoral head and neck. The target for injection is the anterior synovial recess, which is located at the junction of the femoral neck and the femoral head. Effusions may sometimes be seen at this location as hypoechoic areas.
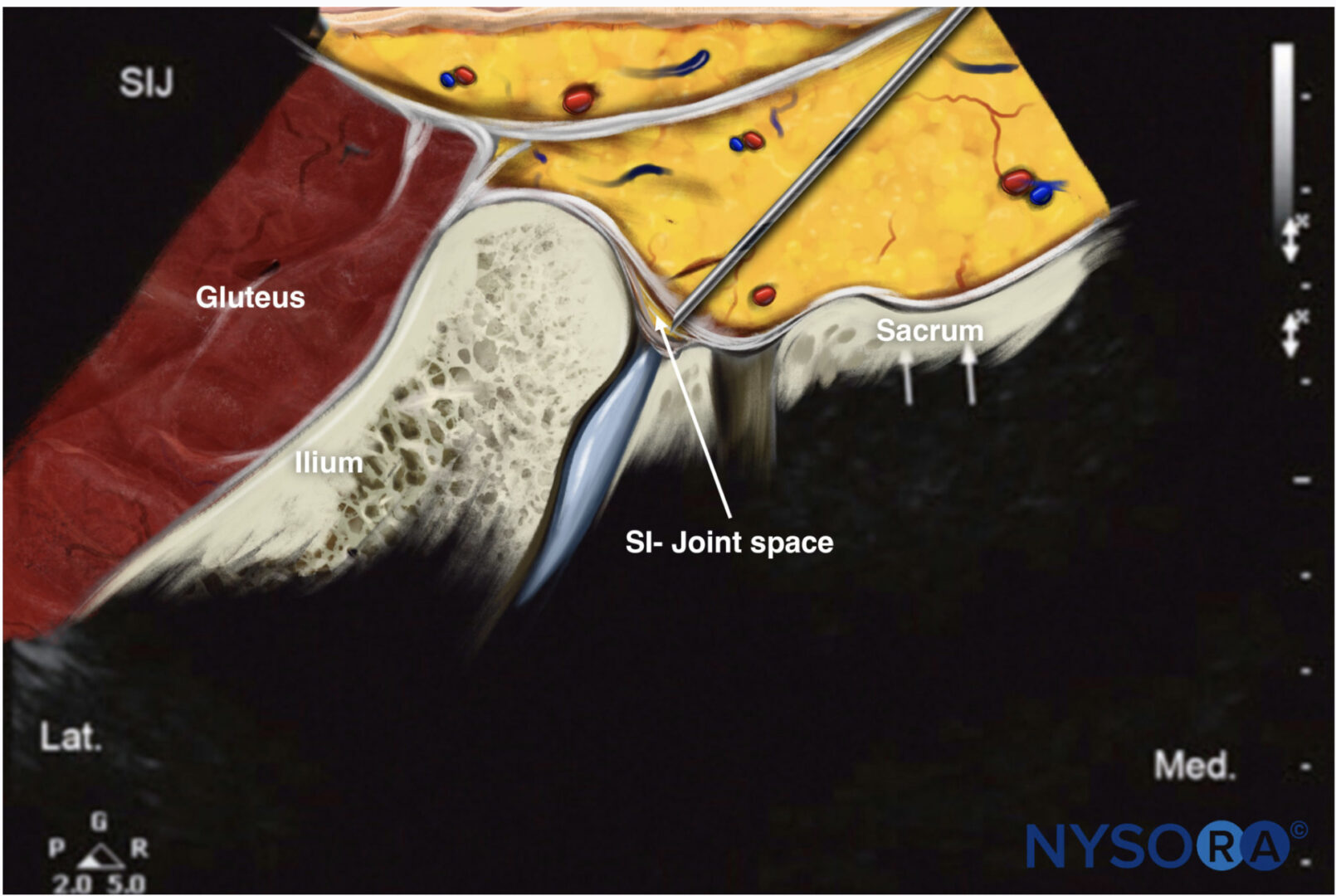
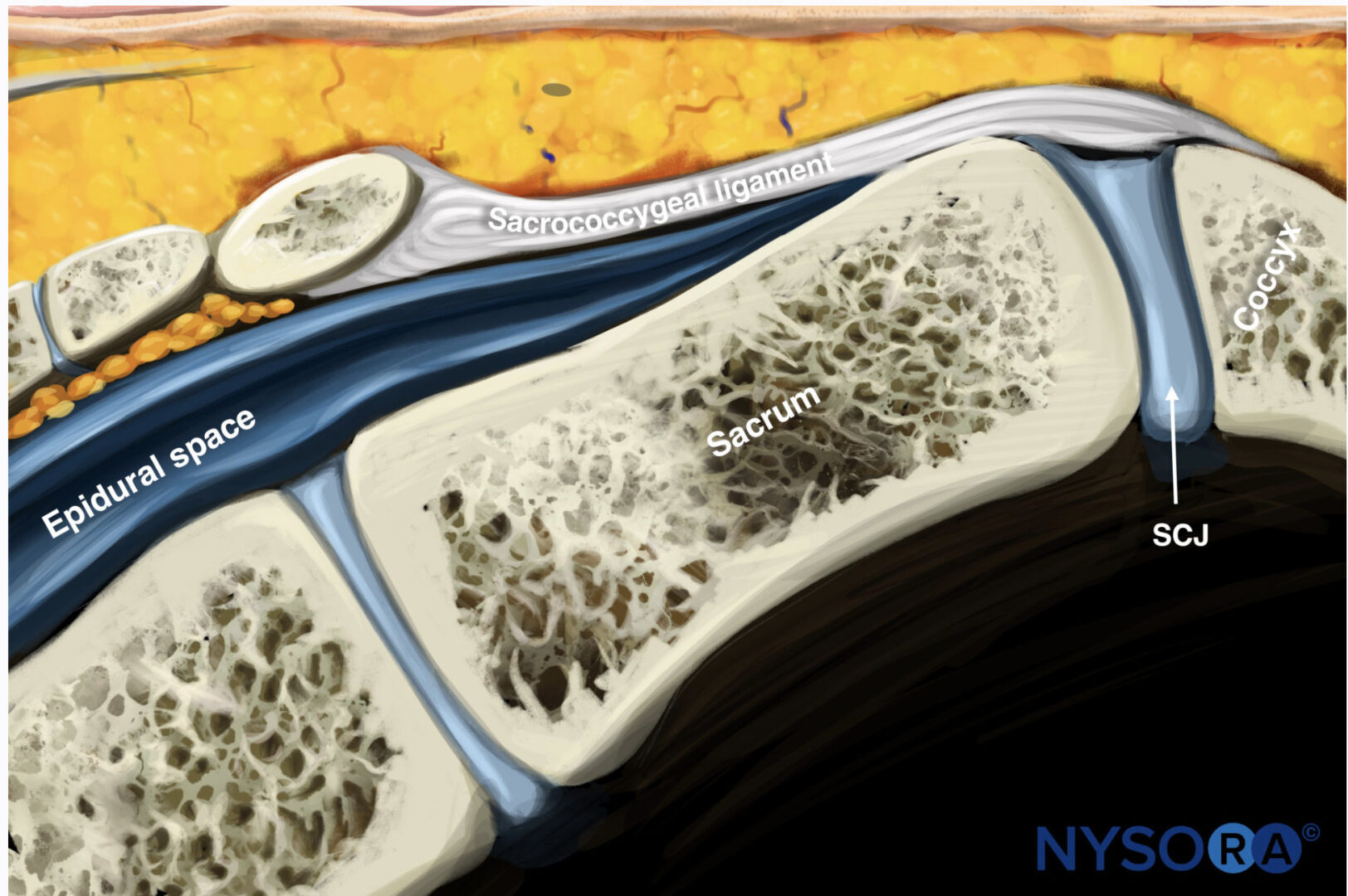
The hip joint may be visualized by starting from the shaft of the femur in a transverse view and working up to the intertrochanteric level. Then the transducer is moved medially and rotated to align with the head of the femur. An alternative approach, called the anterior sagittal approach, involves moving the transducer oriented longitudinally, from the lateral edge of the thigh to the medial until the head of the femur is seen as a hyperechoic, curved line. Subsequent fine-tuning to orient the transducer along the neck provides visualization of the hip joint (Fig. 1). Cephalad to the femoral head, the labrum may be seen as a triangular, hyperechoic structure.
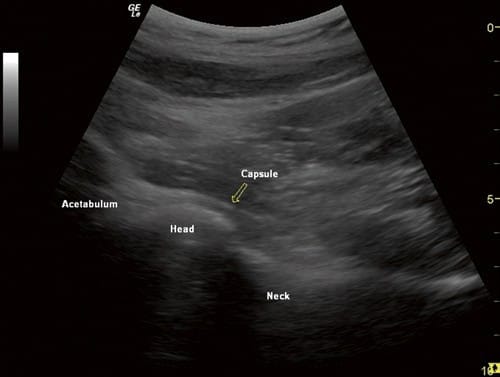
Fig.1 Anterior longitudinal ultrasound view of the hip joint, show-ing the head of the femur, neck, acetabulum, and the capsule
An initial scout scan is performed to identify the neurovascular bundle and the location of the femoral head and neck (Fig. 2). Color Doppler sonography should be used to exclude any blood vessels, especially the circumflex artery, in the needle path (Fig.3).
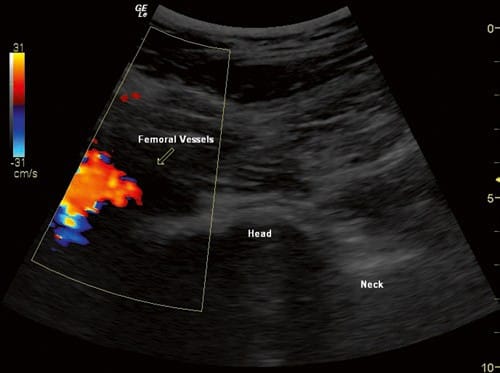
Fig.2 Ultrasound view of an internally rotated normal hip joint, with color flow Doppler showing the femoral vessels. The transducer was placed more medially than normal to get the vessels and the joint in one view

Fig.3 Anterior longitudinal sonographic view of the hip joint, with color flow Doppler showing the circumflex vessels
The skin is prepped with either chlorhexidine gluconate or betadine, and sterile drapes are placed. After identification of the location, orientation, and depth of the femoral head and neck, the transducer is placed in a sterile sheath with an adequate amount of water-soluble gel. A sterile 3.5-inch spinal needle is introduced either in-plane or out-of-plane depending on individual preference and comfort (Fig. 4).
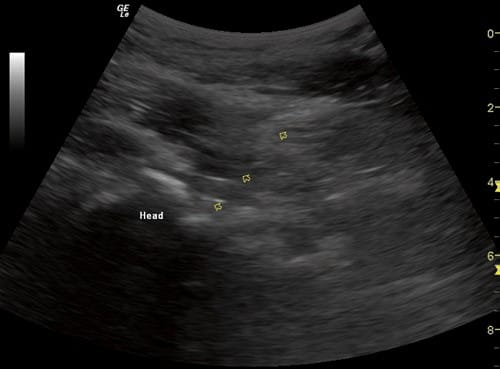
Fig.4 Ultrasound view of a severely arthritic hip showing the femoral head as an irregular, hyperechoic shadow. The arrowheads indicate the 25 G spinal needle
Hydrolocalization may permit identification of the location of the needle tip. The ultrasound view of the femoral head may reveal arthritic changes. During real-time injection he local anesthetic and steroid mixture may appear hyperechoic, and spread is visualized anteriorly beneath the capsule (Fig. 5).
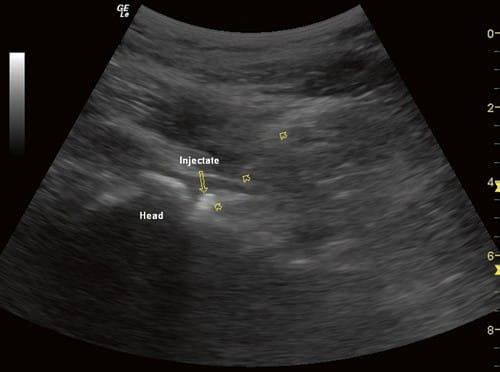
Fig.5 Ultrasound view of the hip joint after a steroid injection showing the injectate as a hyperechoic shadow. The arrowheads point to the 25 G spinal needle
An alternative lateral approach has been described, in which the needle is advanced in-plane from the lateral side with the patient lying with the affected side up and the transducer placed anteriorly.
6. CONCLUSIONS
Visualization of the target site and the surrounding structures ensures improved patient care and demonstrates evidence for the procedural competency of the operating clinician. Although landmark-based and fluoroscopy-guided intra-articular injections provide some visualization, they have attendant risks. Ultrasound imaging can safely and effectively provide real-time needle guidance for hip joint injections while avoiding neurovascular injury and radiation exposure.