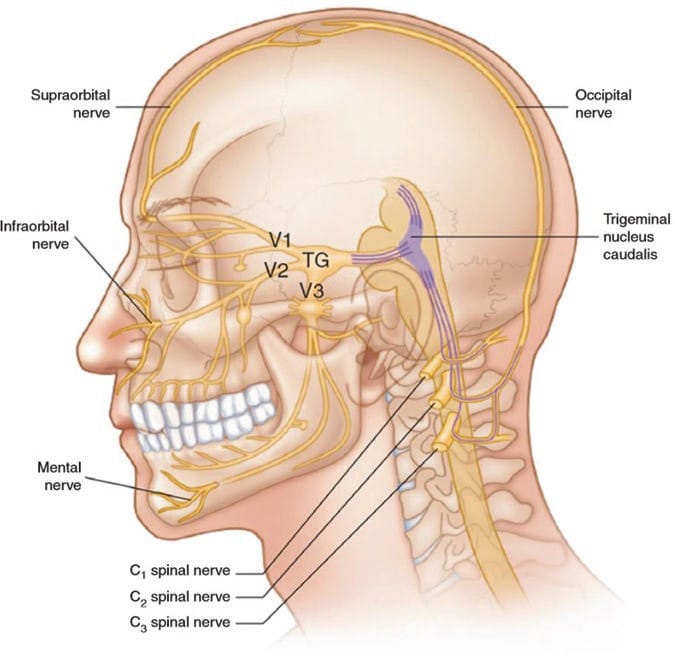
Occipital neuralgia is defined as a unilateral or bilateral paroxysmal, shooting, or stabbing pain in the posterior part of the scalp, in the distribution of the greater, lesser, or third occipital nerves. It is commonly associated with tenderness over the involved nerve and sometimes accompanied by diminished sensation or dysesthesia in the affected area [1]. The pain of occipital neuralgia may reach the frontoorbital area through trigeminocervical interneuronal connections in the trigeminal spinal nucleus (Fig. 1).
1. DIAGNOSTIC CRITERIA
The diagnostic criteria of occipital neuralgia in the International Classification of Headache Disorders (ICHD-3) appear in Table 1.
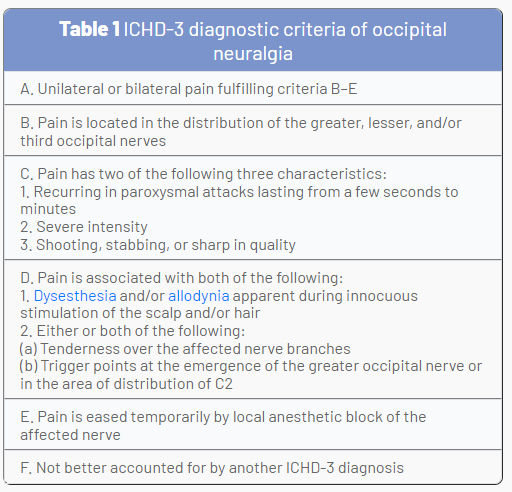
From The International Classification of Headache Disorders, 3rd edition [1]
2. ETIOLOGY
Occipital neuralgia can have many causes:
• Trauma • Infection • Tumors
• Postoperative, especially after Arnold-Chiari malformation surgery or other craniocervical junction surgeries
• Radiofrequency ablation (RFA)
• Atlanto-axial joint (AAJ), rheumatoid arthritis, and subluxation, as the C2 dorsal root ganglion lies over the posterior medial aspect of the joint
• C2 nerve root and dorsal root ganglion (DRG) lesions (e.g., meningioma, vascular malformation)
• Occipital nerve entrapment
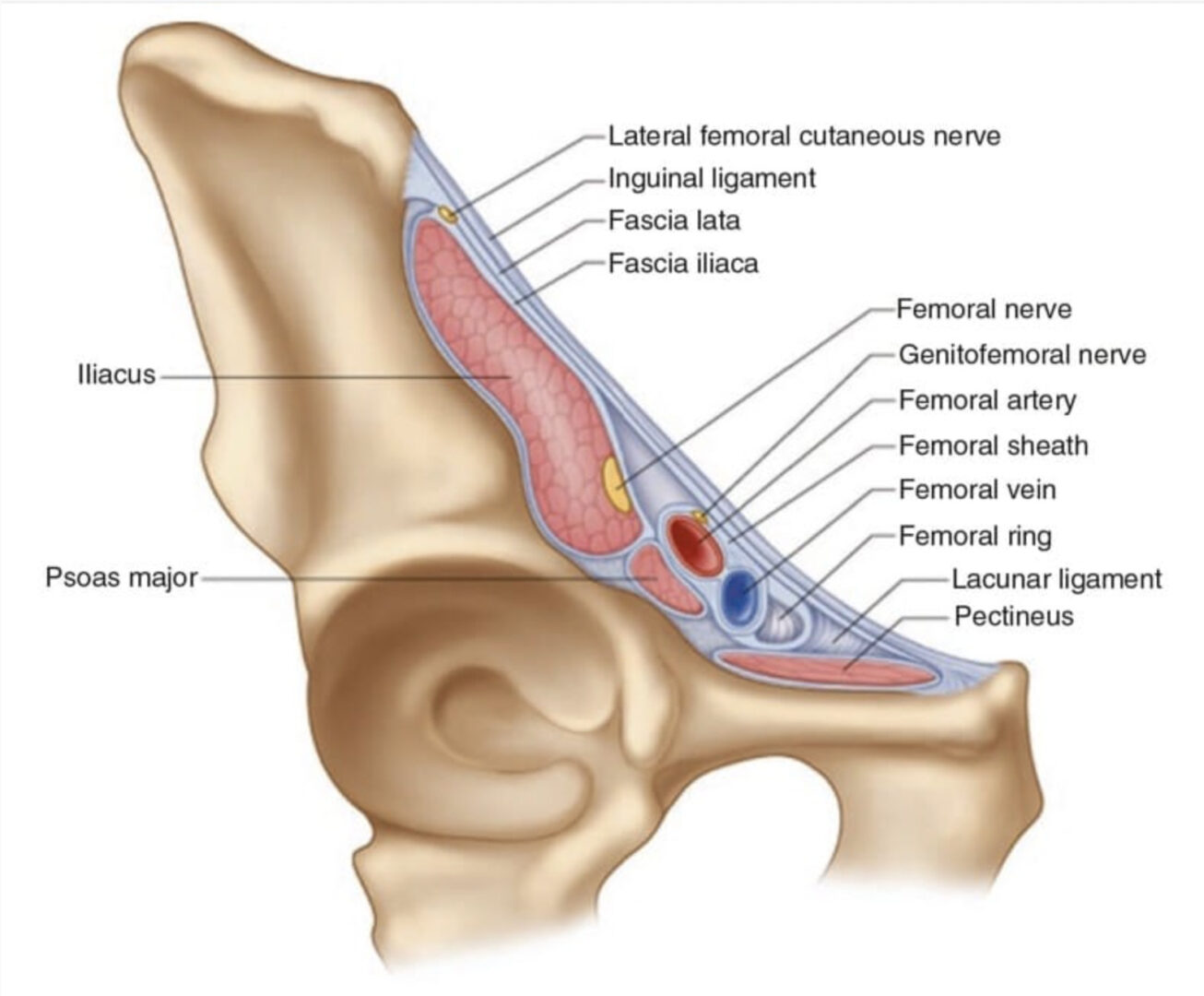
3. OCCIPITAL NERVE ENTRAPMENT
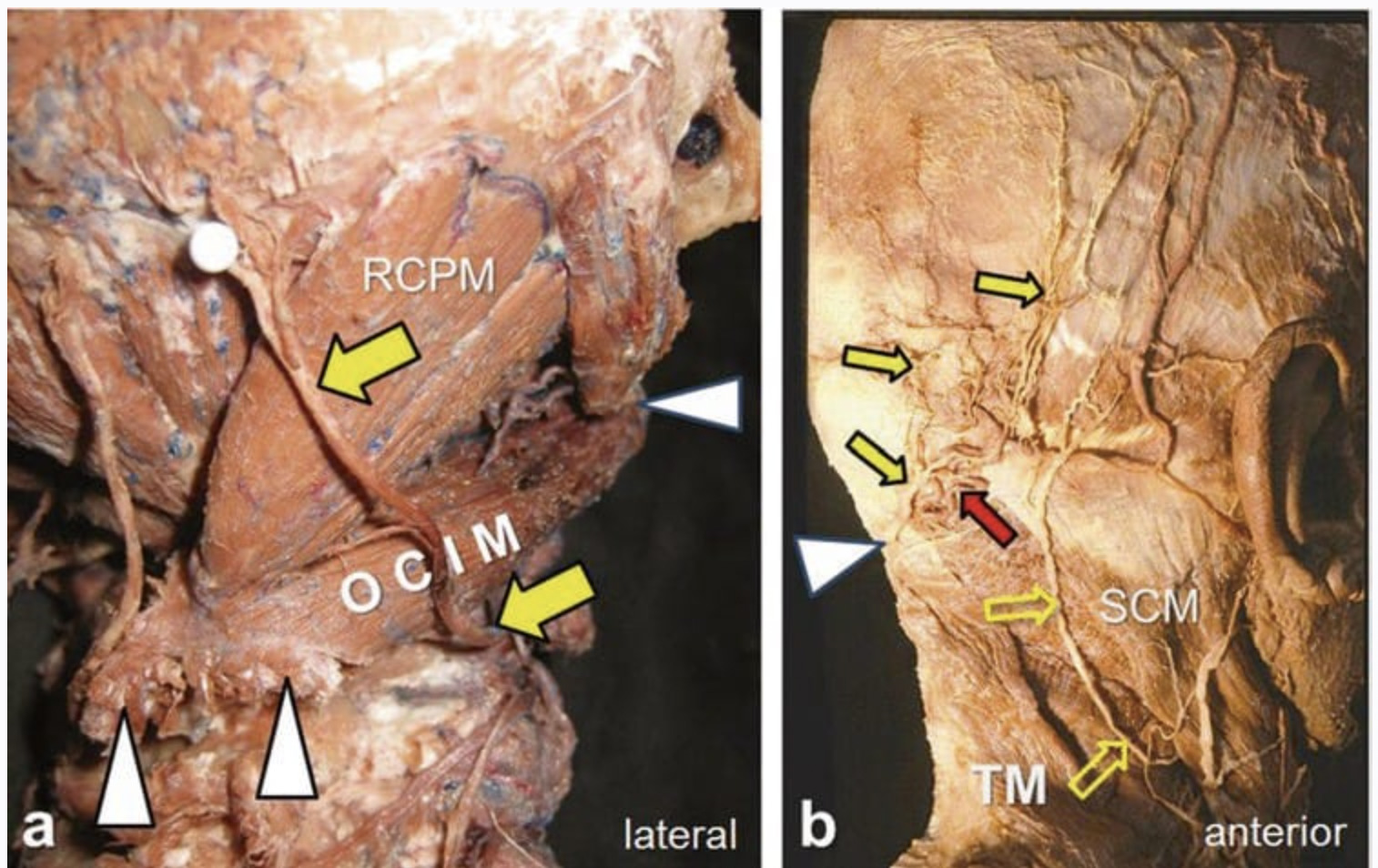
The greater occipital nerve (GON) arises from the C2 dorsal ramus and curves around the inferior border of the inferior oblique muscle to ascend on its superficial surface. Then it penetrates the semispinalis capitis (and invariably the splenius muscle) to end subcutaneously near the nuchal line by penetrating the trapezius muscle or the fascia [3–5]. The GON can be entrapped anywhere from its origin at the C2 nerve root until it becomes subcutaneous at the trapezius aponeurosis.
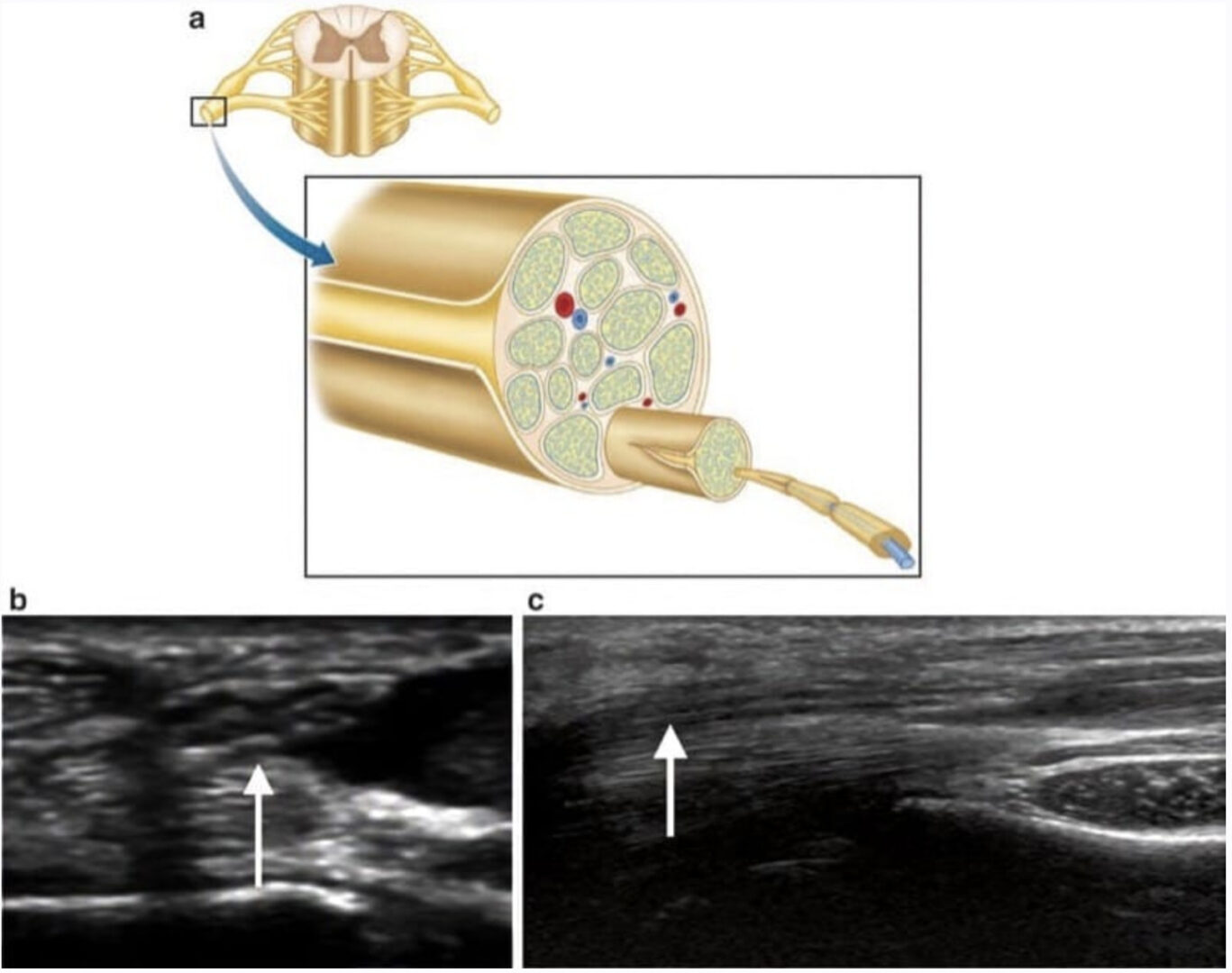
The normative sonographic data indicate that the GON cross-sectional area is 2.0 ± 0.1 mm2 at C1–C2 level (range, 1–4 mm2 ). The size of the GON typically remains the same until it branches in the occipital area. The mean GON crosssectional area in symptomatic patients following entrapment was 4.1 ± 2.6 mm2 (range, 2–13 mm2 ) [6].
4. THE ROLE OF ULTRASOUND IN DIAGNOSIS AND TREATMENT
Diagnostic Ultrasound
• Diagnosis of occipital nerve entrapment by demonstrating enlarged, abnormal, swollen nerve [7, 8] (Figs. 2 and 3).
• Diagnosis of the cause of entrapment, such as entrapment within the suboccipital muscles (Fig. 4) or impingement by an arterial aneurysm or malformation (Fig. 5), venous aneurysm or malformation (Fig. 6), or muscle lesion or mass (Fig. 7).
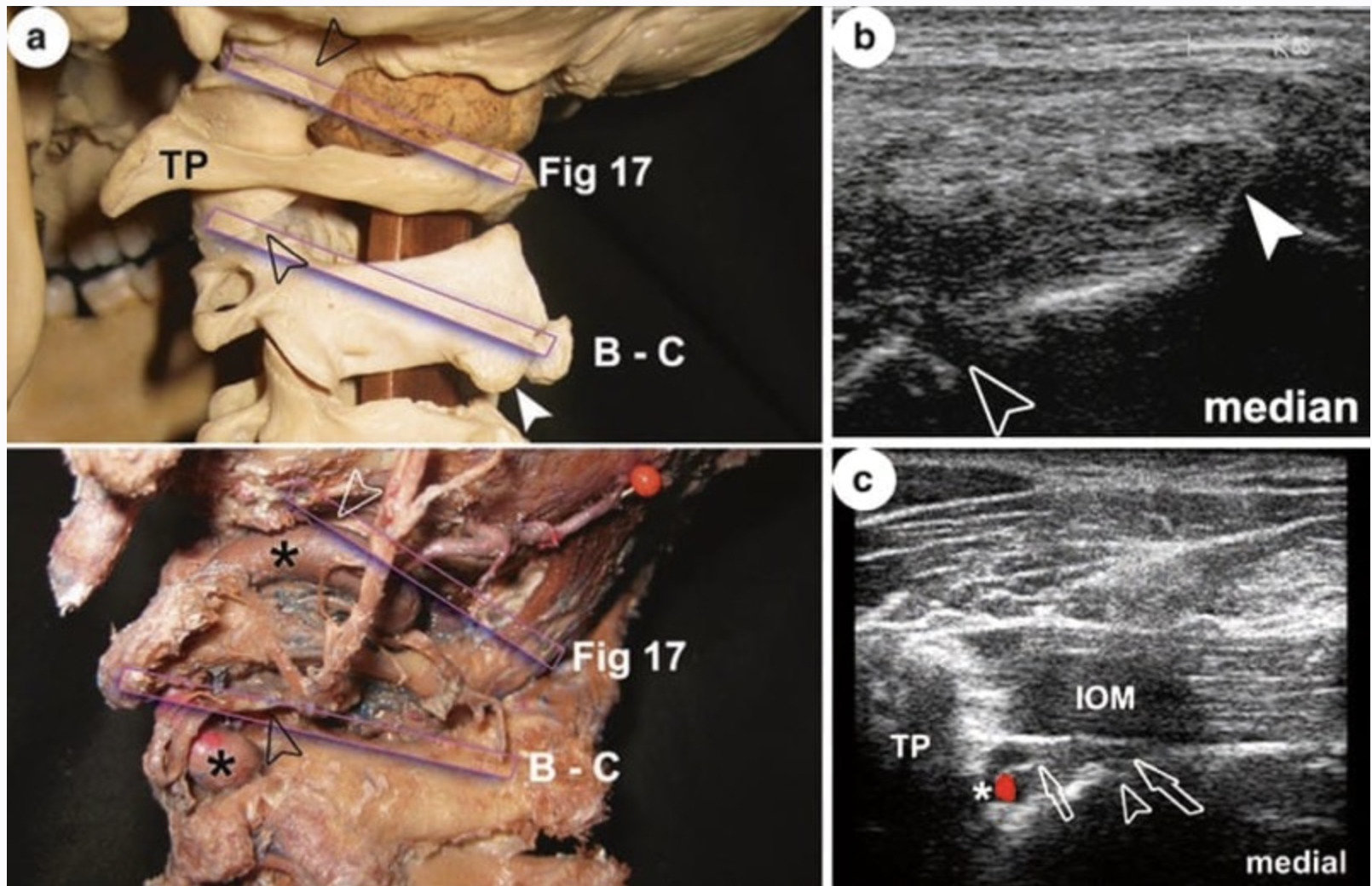
• Tracing the GON: The GON can be traced with ultrasound from its origin at the C2 nerve root all the way until it becomes subcutaneous at the trapezius aponeurosis. Lesions at the level of the C2 nerve root and dorsal root ganglion (DRG) may be identified (Fig. 8).
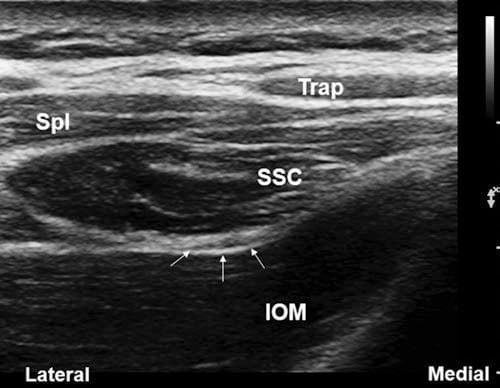
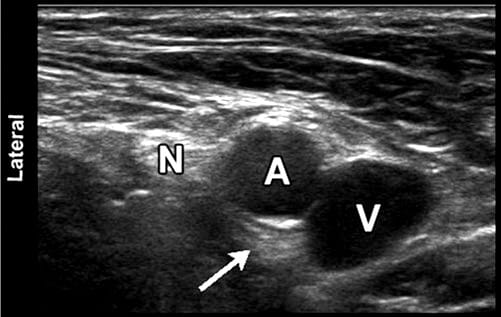
Fig.2 Short-axis sonogram at C1–C2 level showing a normal greater occipital nerve (arrows) as it runs between the inferior oblique muscle (IOM) and the semispinalis capitis (SSC). Trap trapezius muscle, Spl splenius muscle
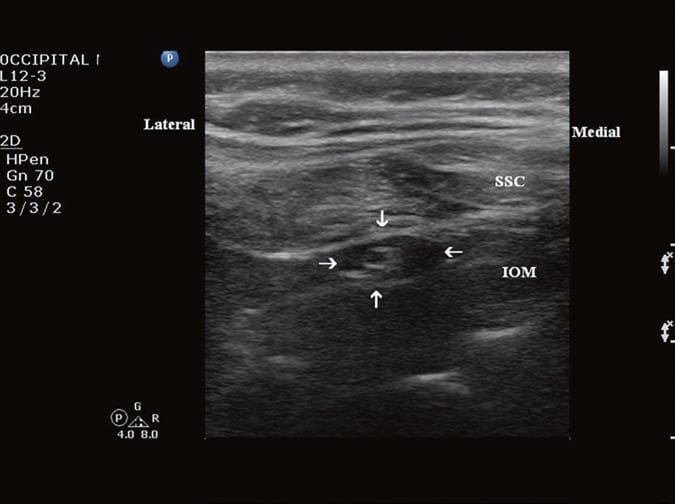
Fig.3 Short-axis sonogram at C1–C2 level showing a swollen greater occipital nerve with edema surrounding the nerve
(arrows) as it runs between the inferior oblique muscle (IOM) and the semispinalis capitis (SSC)
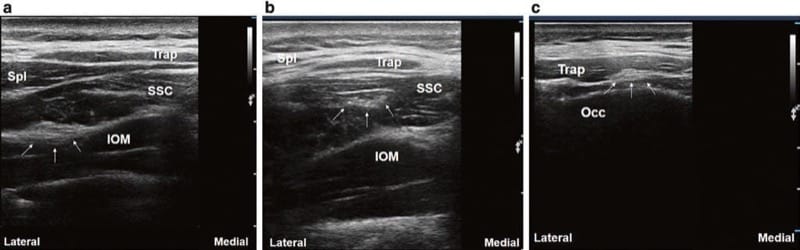
Fig.4 (a) Short-axis sonogram at C1–C2 level showing the greater occipital nerve (arrows) as it runs between the inferior oblique muscle (IOM) and the semispinalis capitis (SSC). (b) Short-axis sonogram at C1 level showing the greater occipital nerve (arrows) entrapped within the belly of the semispinalis capitis (SSC). Notice the enlarged nerve with enhanced fascicular pattern. (c) Short-axis sonogram at the occipi-tal level showing the greater occipital nerve (arrows) as it pierces the trapezius muscle (Trap). Notice the swollen, enlarged nerve. Occ occiput, Spl splenius muscle
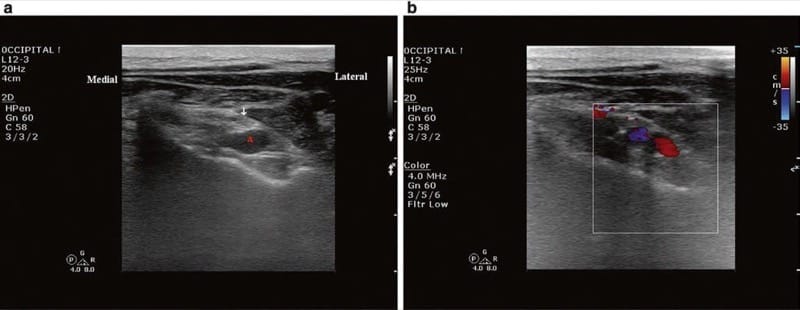
Fig.5 (a, b) Short-axis sonogram at C1–C2 level showing an abnormal artery (a) impinging the greater occipital nerve (arrow) as it runs between the inferior oblique muscle (IOM) and the semispinalis capitis (SSC). (Figure b with color Doppler)
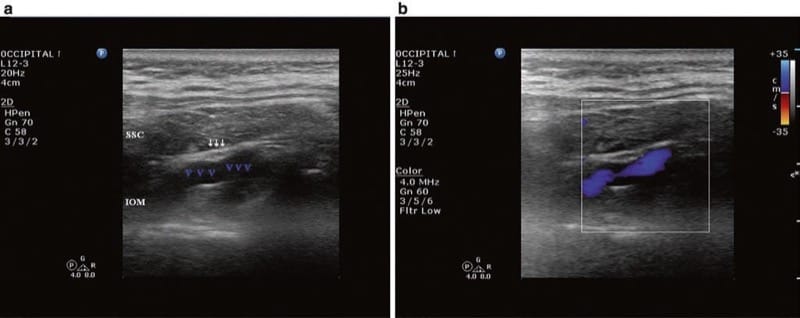
Fig.6 (a, b) Short-axis sonogram at C1–C2 level showing an abnormal vein (VV) impinging the greater occipital nerve (arrows) as it runs between the inferior oblique muscle (IOM) and the semispinalis capitis (SSC). (Figure b with color Doppler)
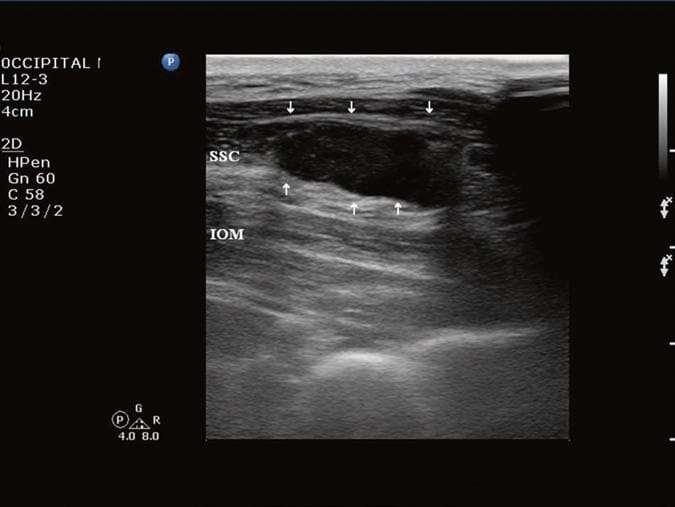
Fig.7 Short-axis sonogram at C1–C2 level showing a cyst (arrows) within the semispinalis capitis (SSC). IOM inferior oblique muscle
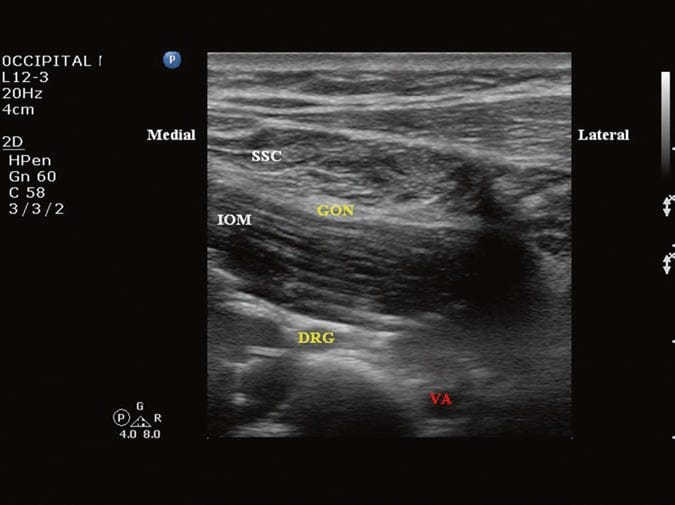
Fig.8 Short-axis sonogram at C2 level showing the C2 dorsal root ganglion
(DRG), the vertebral artery (VA), and the greater occipital nerve (GON) between the inferior oblique muscle (IOM) and the semispinalis capitis (SSC)
5. INTERVENTIONAL ULTRASOUND
• Ultrasound-guided occipital nerve block: The procedure can be performed either distally at the nuchal line (Fig. 9, position A) or more proximally between C1 and C2 (Fig. 9, position B) [9]. We prefer blocking the GON at the C1–C2 level, where it runs between the inferior oblique muscle (IOM) and the semispinalis capitis muscle (SSC). The GON is well identified here and can be easily targeted, rather than trying to identify the terminal subcutaneous branches at the nuchal line. The procedure can be performed with the patient in either the prone or sitting position. A high-frequency ultrasound transducer is usually used, though a low-frequency transducer may be used, depending on body habitus. First, a transverse short-axis view is obtained by applying the transducer in the midline over the occiput and then scanning caudally to identify the C1 and C2 levels. C1 lacks a spinous process, and the first bifid spinous process encountered is C2 (Fig. 10). Then the transducer is moved laterally until the suboccipital muscles are seen in the view. To better differentiate the IOM from the SSC, the lateral end of the transducer is tilted cephalad to be in line with the orientation of the IOM as it stretches between C1 and C2. By changing the transducer orientation in this manner, the sonogram will show the IOM in its long axis, while obtaining a short-axis view of the SSC and thus clearly differentiating the two muscles and the fascial plane in between, where the GON can be searched for (Fig.11).
• Ultrasound-guided botulinum toxin type A injections into the surrounding suboccipital muscles to relieve the pressure on the GON. Recent studies have shown that injection of botulinum toxin A into the “presumable” sites of GON entrapment provided some relief in symptomatic patients [10, 11]. It reduced headache and somewhat improved the quality of life for 3 months. Our observations indicate that botulinum toxin may provide sustained relief in patients with occipital neuralgia when injected into a “specific” entrapment location (rather than into the site of potential or “presumed” entrapment). The appropriate site for injection may be identified with bedside ultrasound imaging. The normalization of biomechanics after the release of the occipital nerve is likely the source of the long-term recovery, rather than prolonged action of the botulinum toxin itself.
• Ultrasound-guided occipital peripheral nerve stimulation.
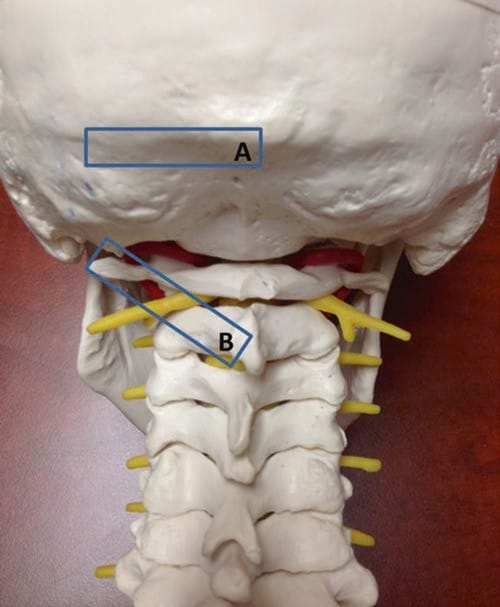
Fig.9 The position and orientation of the ultrasound transducer for greater occipital nerve block. (a) nuchal line; (b) C1–C2 level
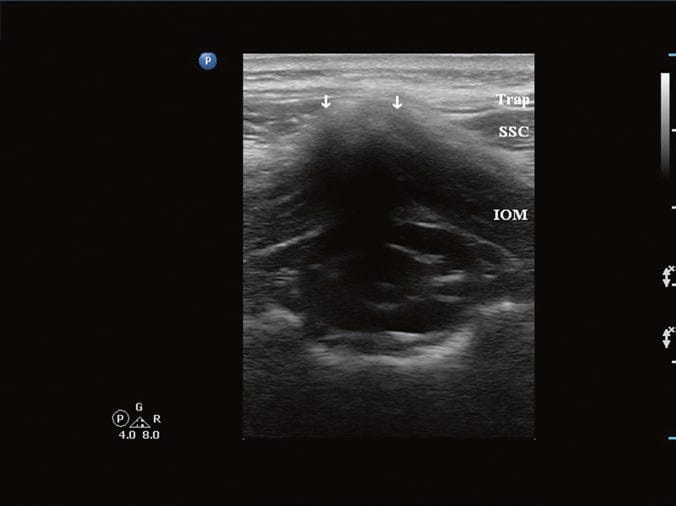
Fig.10 Short-axis sonogram at C2 level. Note the bifid spinous process of C2 (arrows). IOM inferior oblique muscle, SSC semispinalis capitis muscle, Trap trapezius muscle
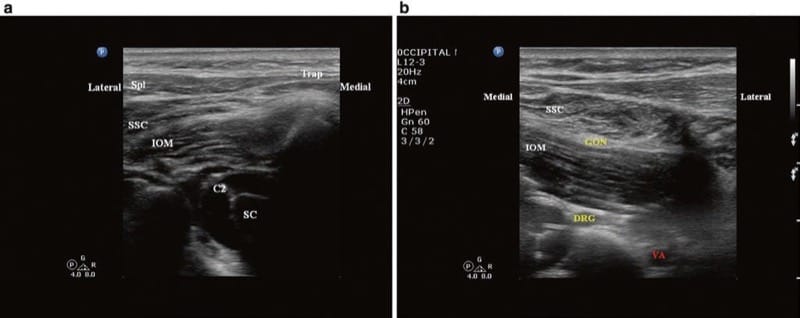
Fig.11 Short-axis sonogram at C1–C2 level. (a) The ultrasound transducer is in a horizontal position, so both the inferior oblique mus-cle (IOM) and the semispinalis capitis muscle (SSC) appear in a short- axis cut. (b) The lateral end of the ultrasound transducer is tilted cephalad; now the IOM appears in a long-axis cut and thus can be easily differentiated from the SSC, and the greater occipital nerve (GON) can be identified in between. C2 C2 nerve root, DRG C2 dorsal root ganglion, SC spinal cord at C2 level, Spl splenius muscle, Trap trapezius muscle, VA vertebral artery