Pathology of peripheral nerves can occur secondary to a variety of etiologies, including mechanical entrapment, compression by external factors, trauma, infectious and inflammatory causes, neoplasm, or as a complication of surgery. Clinical evaluation often begins with a detailed history and focused physical exam and may include electrodiagnostic studies or advanced imaging. With recent innovations in MRI techniques, high-resolution MRI of peripheral nerves is possible and is often referred to as “MR neurography.” MR imaging can demonstrate both primary signs of nerve injury and secondary signs such as muscle denervation. Ultrasound can be used as a complementary or alternative imaging modality for diagnostic evaluation of peripheral nerves. Advantages of ultrasound include dynamic assessment of peripheral nerves, easy evaluation of the contralateral side for comparison, and utility in patients who cannot tolerate MRI or in cases where MRI is limited by metallic hardware. Ultrasound can also be used to guide diagnostic and therapeutic perineural injections with anesthetic and/or corticosteroids. This course reviews ultrasound findings of peripheral nerve pathology.
1. TECHNIQUE
Diagnostic peripheral nerve ultrasound should be performed by an experienced physician. The patient should be placed in a comfortable position to optimize imaging of the nerve in question. Typically, a high-frequency transducer (usually 12–18 MHz) is utilized. For deeper nerves, a 9-MHz transducer can be used. Images can be obtained in either grayscale or chromatic scale, depending on physician preference. Both transverse and longitudinal imaging of the nerve should be obtained. Dynamic sonography, if indicated, can be performed by gently maneuvering the patient’s limb to demonstrate nerve subluxation or mechanical impingement. Sonopalpation can be applied to assess the reproducibility of the patient’s symptoms. For subtle findings, imaging of the contralateral nerve may be helpful for comparison. Vascular Doppler imaging may also be useful to help distinguish very small nerves from vessels.
2. NERVE ANATOMY
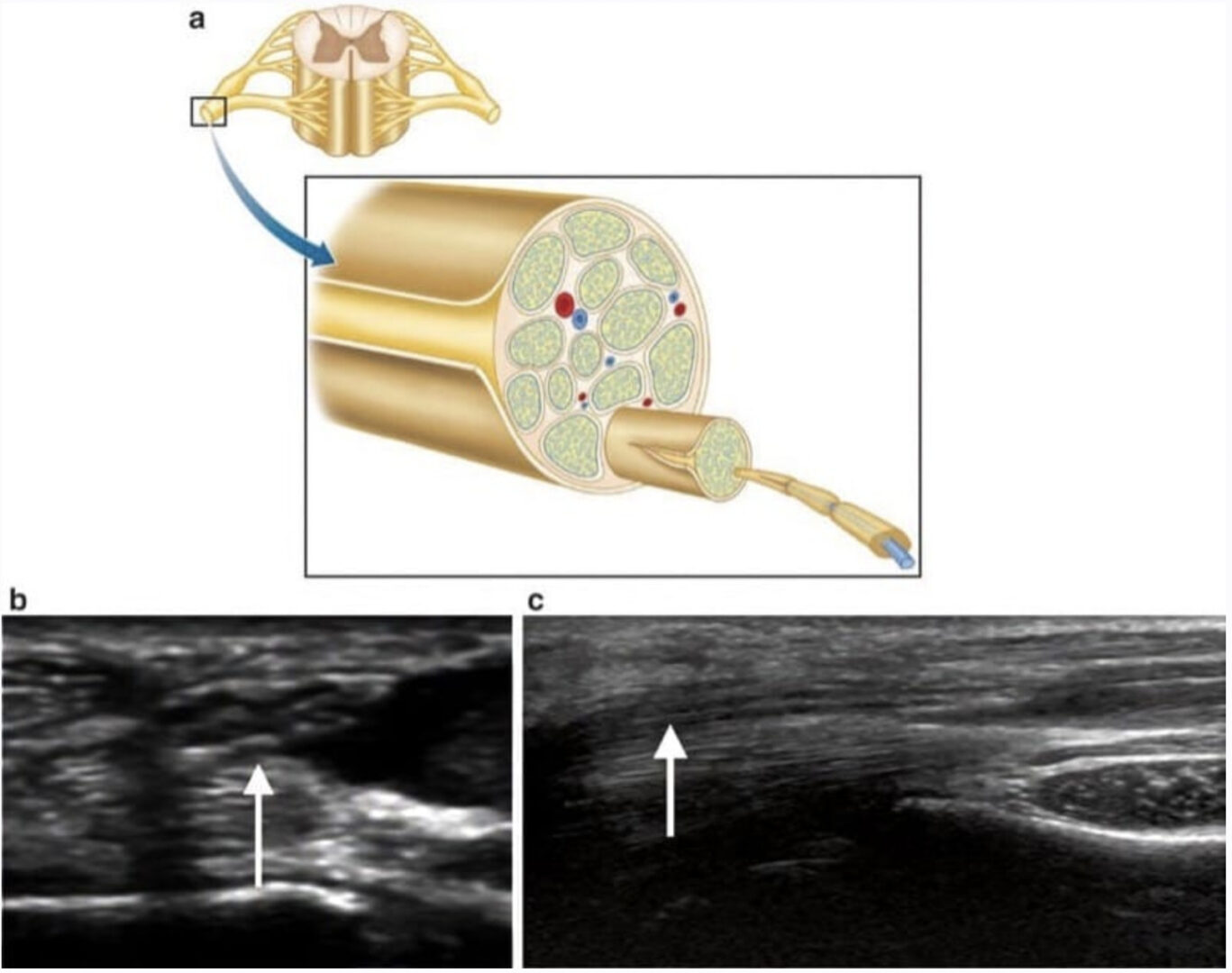
Peripheral nerves are composed of individual axons, which are bundled together to form a fascicle. Several fascicles are grouped together to form the nerve, which is wrapped in a layer of connective tissue called the epineurium. On ultrasound, nerve anatomy can be appreciated up to the fascicular level. Transverse sonography of a normal peripheral nerve will demonstrate a typical “honeycomb” appearance with hypoechoic individual fascicles and a surrounding echogenic epineurium. Longitudinal sonography should demonstrate the nerve in continuity, with even caliber along its course (Fig. 1).
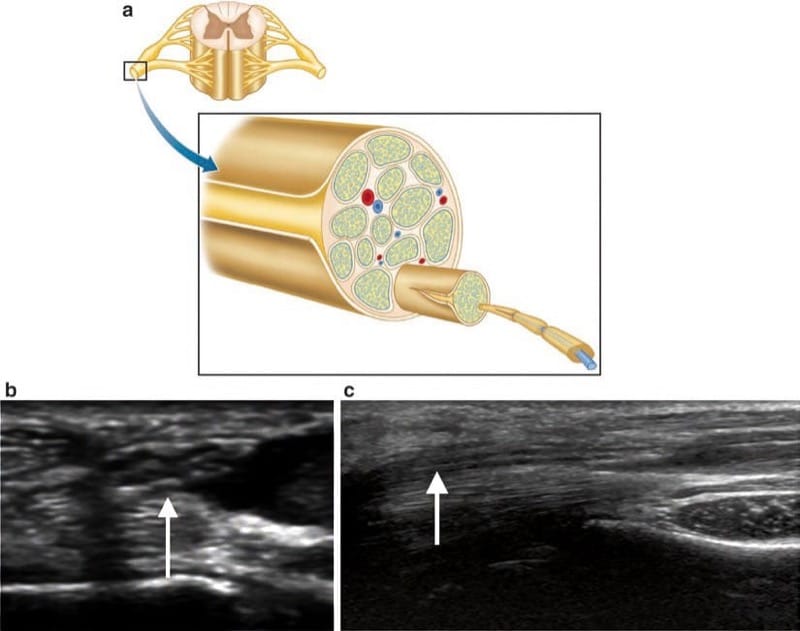
Fig.1 (a) Anatomy of a peripheral nerve. Transverse (b) and longitudinal (c) ultrasound demonstrates the normal sonographic appearance of a peripheral nerve, with hypoechoic fascicles and surrounding echo-genic epineurium. The typical “honeycomb” appearance of peripheral nerves is appreciated on transverse imaging. Longitudinal ultrasound demonstrates normal nerve size and continuity along its course. (a, original artwork by Dr. Victoria Young)
3. NERVE INJURY
Nerve injury can be characterized according to the Seddon and Sunderland classification Scheme [1]. Neurapraxia, the mildest type of nerve injury, affects only the myelin sheath. Corresponding ultrasound findings may include nerve thickening and fascicular enlargement.
Effacement or disruption of nerve fascicles suggests axonotmesis, axonal rupture with an intact supporting connective tissue scaffold. Ultrasound findings may include nerve enlargement, fascicular enlargement, and loss of internal fascicular architecture. An intact epineurium should be present. Finally, neurotmesis represents total nerve severance and can be seen on ultrasound as discontinuity of the nerve.
4. NEURITIS
Neuritis is a broad term used to describe inflammation of any nerve, resulting in pain or other sensory or motor dysfunction. Peripheral nerve neuritis can be caused by trauma, iatrogenic injury, infection, or mechanical impingement, or it can be idiopathic. On ultrasound, neuritis is characterized by focal nerve enlargement and abnormal fascicular appearance (Fig. 2). In subtle cases, comparison to a normal contralateral side may prove helpful.
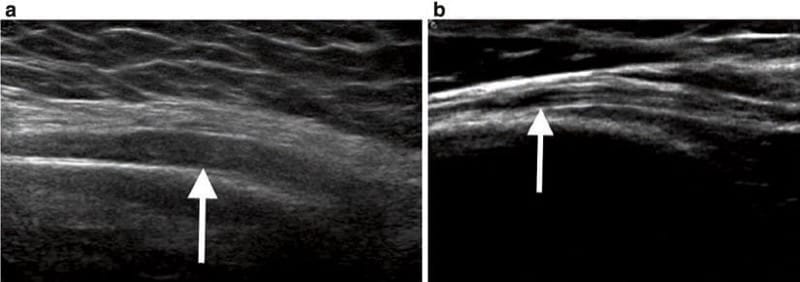
Fig.2 (a) Ultrasound demonstrates diffuse thickening of the radial nerve within the mid-arm. (b) Normal sonographic appearance of the radial nerve in a different patient
5. NERVE SUBLUXATION
Dynamic ultrasound is extremely useful for diagnosing nerve subluxation or dislocation. Evaluation of ulnar nerve subluxation at the elbow, for example, is a common request. Although ulnar nerve subluxation at the elbow is asymptomatic in many cases, it can predispose to nerve injury (Fig. 3) [2]. Sonographic evaluation of the elbow at the level of the medial epicondyle should be performed with slow flexion and extension to demonstrate potential subluxation of the ulnar nerve anterior to the medial epicondyle and subsequent “snap” back into the cubital tunnel (Fig. 4). Concomitant subluxation of the medial head of the triceps may be observed in some patients.
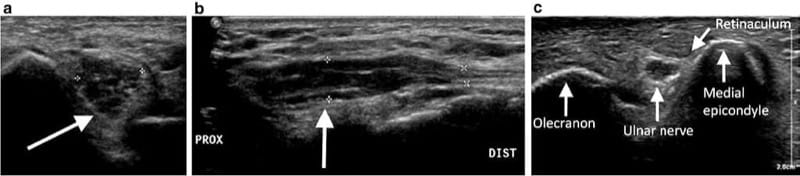
Fig.3 Transverse (a) and longitudinal (b) ultrasound of the elbow in a patient with clinical history of cubital tunnel syndrome demon-strates segmental enlargement of the ulnar nerve within the cubital tunnel. On longitudinal imaging, the normal size of the ulnar nerve can be appreciated distally. (c) Transverse posterior ultrasound of the elbow in a different, asymptomatic patient demonstrates normal appearance and positioning of the ulnar nerve within the cubital tunnel
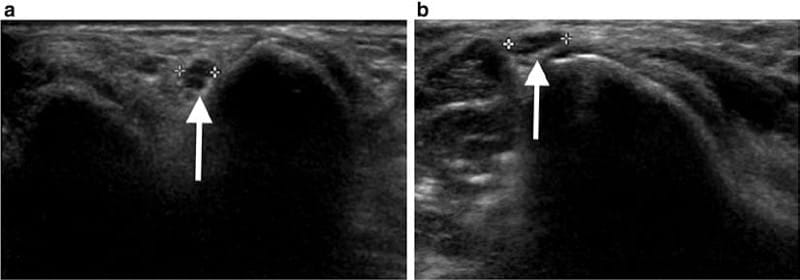
Fig.4 Dynamic ultrasound of the ulnar nerve at the cubital tunnel demonstrates ulnar nerve subluxation. On extension imaging (a), the ulnar nerve is visualized within the cubital tunnel. Upon flexion imaging (b), however, the ulnar nerve is seen subluxating over the medial epicondyle
6. NERVE ENTRAPMENT/IMPINGEMENT
Anatomic peripheral nerve entrapment occurs when a nerve courses through a constricted space secondary to osseous, ligamentous, or fibrous constraints. For example, entrapment of the medial nerve within the carpal tunnel is a common indication for sonographic evaluation (Fig. 5).
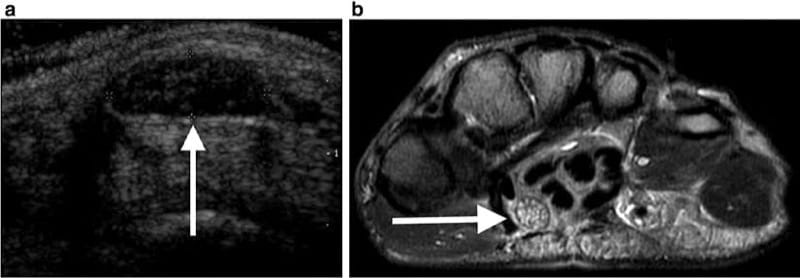
Fig.5 (a) Ultrasound of the wrist in a 55-year-old woman with tingling in her fingers demonstrates focal enlargement and loss of fascicular architecture of the median nerve within the carpal tunnel. (b) Axial MR image confirms enlargement and signal hyperintensity of the median nerve within the carpal tunnel
Other potential entrapment sites include the ulnar nerve in Guyon’s canal or in the cubital tunnel and the tibial nerve at the ankle in tarsal tunnel syndrome. Ultrasound findings of nerve entrapment may include segmental nerve swelling and pain upon sonopalpation (Figs. 6 and 7). Denervation effect and muscle atrophy may be seen in cases involving peripheral nerves with motor function and can be demonstrated on ultrasound as increased echogenicity of the affected muscle [3].
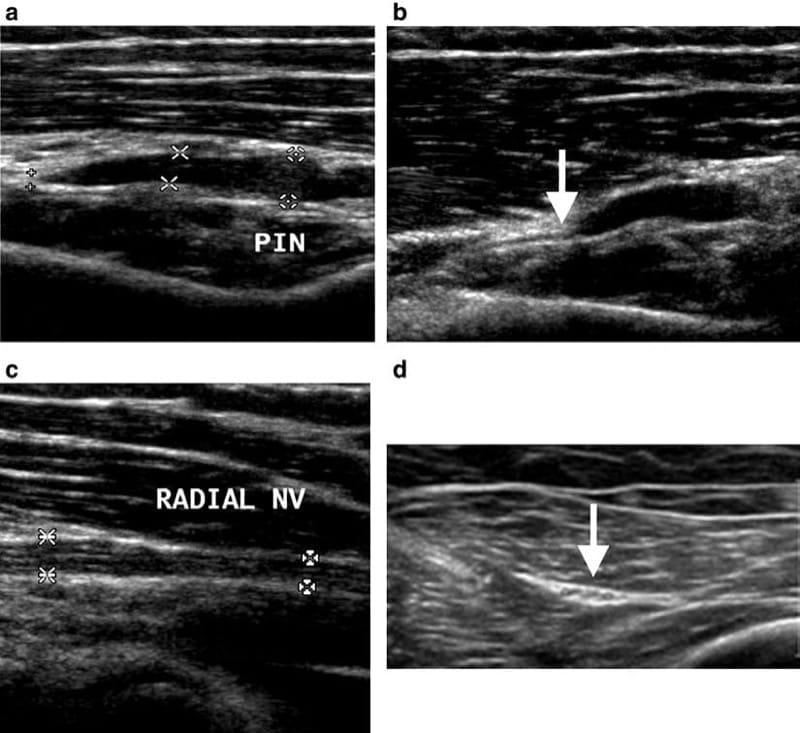
Fig.6 (a) Ultrasound in a patient with clinical symptoms of posterior interosseous nerve (PIN) syndrome demonstrates marked thickening and loss of internal fascicular architecture of the posterior interosseous nerve. (b) Distally, the posterior inter-osseous nerve resumes normal size. The posterior interosseous nerve is the deep branch of the radial nerve and passes between the two heads of the supinator muscle deep to the arcade of Frohse, where it is susceptible to entrapment. (c) Ultrasound of the radial nerve demonstrates normal size and echogenicity. (d) Ultrasound of the contralateral limb, shown for comparison, demonstrates normal size and echogenicity of the contralateral posterior interosseous nerve
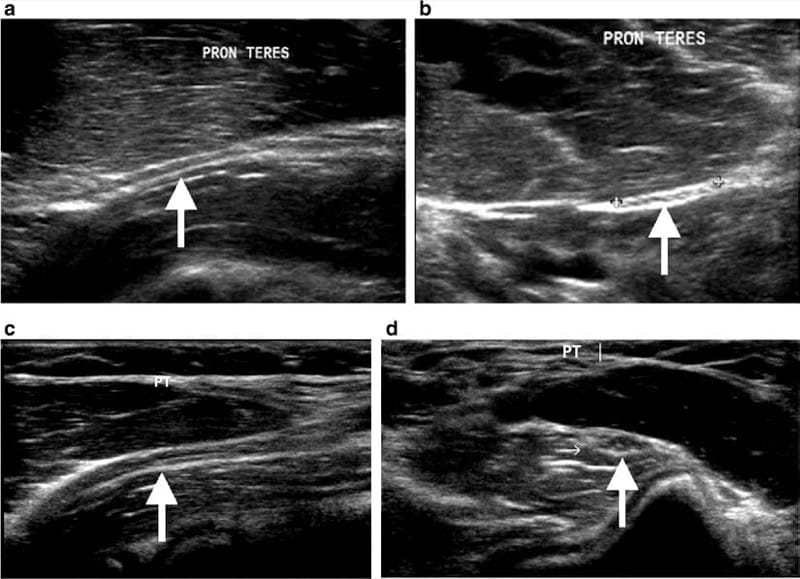
Fig.7 Longitudinal (a) and transverse (b) ultrasound demonstrate enlargement of the pronator teres muscle with compression of the underlying median nerve (arrows). Longitudinal (c) and transverse (d) ultrasound of the contralateral side, shown for comparison, demonstrates normal appearance of the pronator teres muscle and the median nerve (arrows)
Nerve entrapment can also occur secondary to multiple nonanatomic factors. Osseous fracture fragments, osteophytes, and metallic hardware may impinge on a peripheral nerve, leading to nerve injury and dysfunction. Similarly, neoplasm, hematoma, or ganglion cyst can exert mass effect with subsequent nerve injury. Ultrasound can directly demonstrate impingement on a peripheral nerve as well as primary findings of nerve injury such as segmental nerve swelling and loss of fascicular architecture.
Chronic compression secondary to external factors is another mechanism of nerve impingement. For example, in Wartenberg’s disease, the superficial branch of the radial nerve can be injured due to over-tightened handcuffs or a watch strap, leading to sensory abnormality or pain (Fig. 8) [2]. In posttraumatic or postoperative cases, scar tissue may tether or even encase a peripheral nerve. On ultrasound, scar is identified as hypoechoic tissue (Fig. 9).
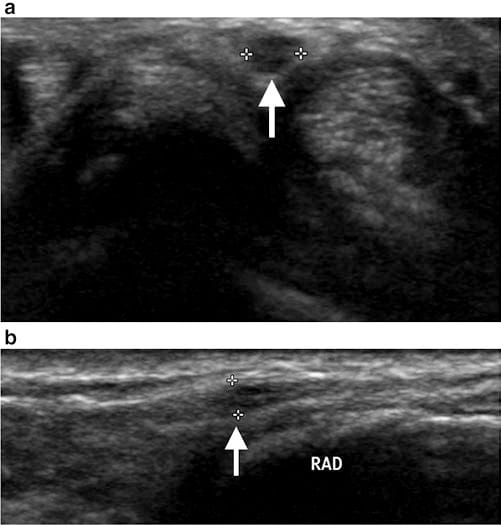
Fig.8 Transverse (a) and longitudinal (b) ultrasound of the wrist in a middle-aged woman with paresthesias of the thumb extending from the dorsal radial forearm demonstrates focal thickening and hypoechogenicity of the superficial branch of the radial nerve, consistent with a neuroma. The patient reported that her symptoms were exacerbated by wearing a watch
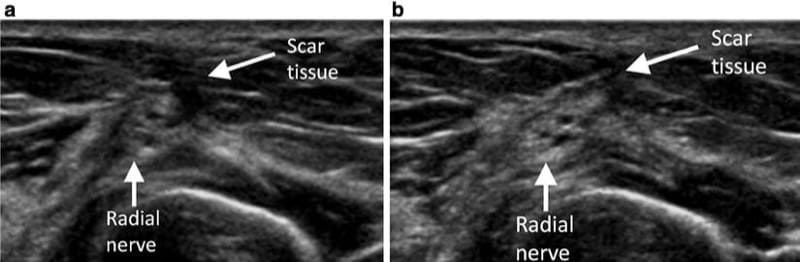
Fig.9 (a, b) Ultrasound of the mid-arm demonstrates hypoechoic scar tissue tethering the radial nerve. The radial nerve demonstrates mild enlargement and loss of normal fascicular architecture
7. NERVE TRANSECTION/NEUROMA
Laceration or transection of a peripheral nerve can be visualized on ultrasound as focal discontinuity in both transverse and longitudinal imaging. Adjacent soft tissue injury may be appreciated. In cases of traumatic injury, ultrasound can also be used to assess for a potential foreign body.
If nerve fibers abnormally regenerate after transection or traumatic injury, a neuroma may form, and it can be painful. Ultrasound findings of neuroma include fusiform, mass-like thickening of the nerve with hypoechogenicity, and loss of fascicular architecture (Figs. 10 and 11). Neuromas can occur at the end of a nerve (stump neuroma) or in continuity along the course of the nerve.
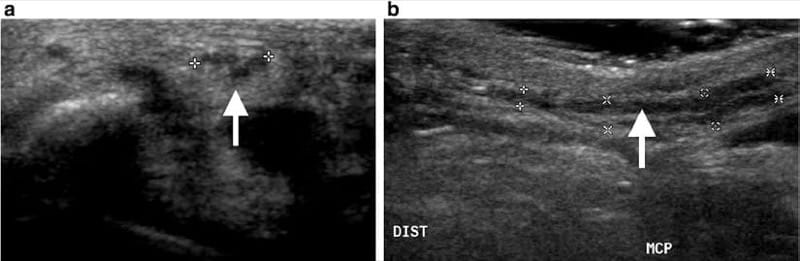
Fig.10 Transverse (a) and longitudinal (b) ultrasound of the thumb demonstrates focal thickening, hypoechogenicity, and enlarged fascicles of the ulnar digital nerve in a 40-year-old male semi-professional bowler, who presented with ulnar-sided thumb pain and a palpable nodule. Findings are consistent with a neuroma of the ulnar digital nerve of the thumb
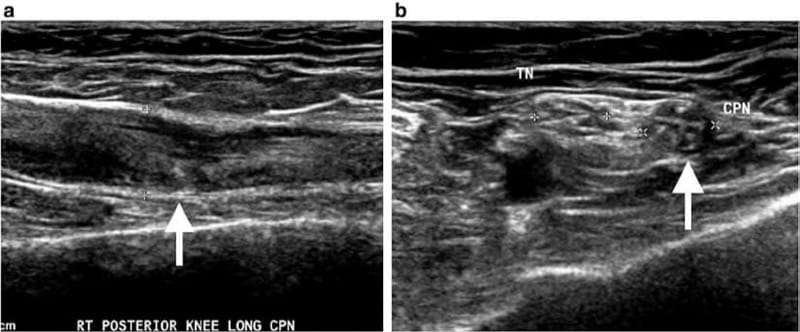
Fig.11 Longitudinal (a) and transverse (b) ultrasound of the knee demonstrates focal thickening, hypoechogenicity, and loss of normal fascicular architecture of the common peroneal nerve (CPN, arrow), consistent with a posttraumatic neuroma. The tibial nerve (TN) is nor-mal in size and appearance
8. NERVE MASS LESIONS/TUMORS
Ultrasound can demonstrate mass lesions of peripheral nerves including peripheral nerve sheath tumors, intraneural ganglion cysts, and fibrolipomatous hamartoma. On sonography, schwannomas and neurofibromas both appear as a hypoechoic mass in continuity with the peripheral nerve (Fig. 12).
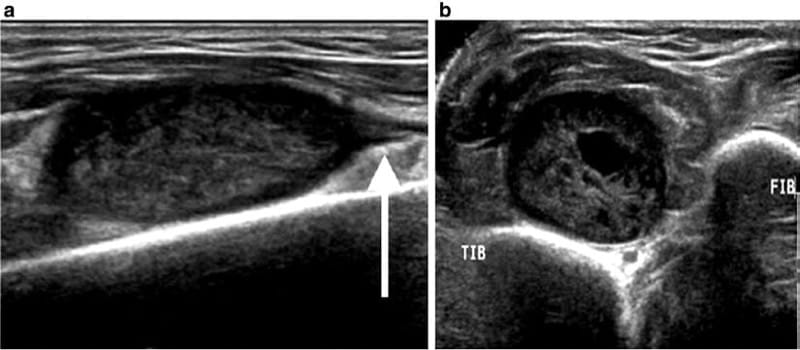
Fig.12 Longitudinal (a) and transverse (b) ultrasound in a patient with a palpable mass demonstrates a well-circumscribed mass along the course of the deep branch of the peroneal nerve (arrow), consistent with a nerve sheath tumor
Color and power Doppler imaging usually demonstrates internal flow, which can help differentiate nerve sheath tumors from complex ganglion cysts. Neurofibromas may be multiple, are associated with a typical “target” appearance, and are usually located centrally relative to the nerve. In contrast, schwannomas typically demonstrate an eccentric location relative to the affected nerve. An enlarging peripheral nerve sheath tumor is concerning for potential malignancy and warrants further evaluation [4].
An intraneural ganglion cyst can occur within the common peroneal nerve with potential extension to the sciatic or tibial nerves. Ultrasound findings include an anechoic fluid collection along the nerve [4]. Fibrolipomatous hamartoma is a rare benign tumor that can involve peripheral nerves and may result in compression neuropathy, most commonly carpal-tunnel syndrome. Ultrasound findings involve a fibrofatty mass infiltrating the affected peripheral nerve (Fig. 13) [5].
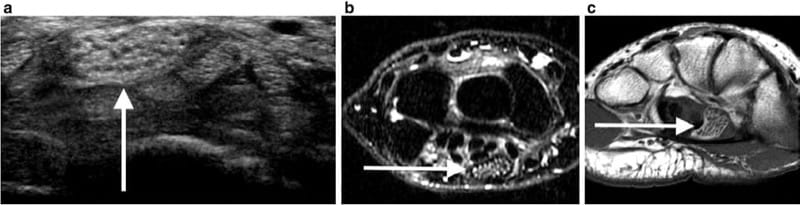
Fig.13 (a) Ultrasound of the wrist of a 20-year-old patient with paresthesias of the thumb, index finger, and middle finger demonstrates a fatty mass lesion within the median nerve. (b, c) Axial MR images
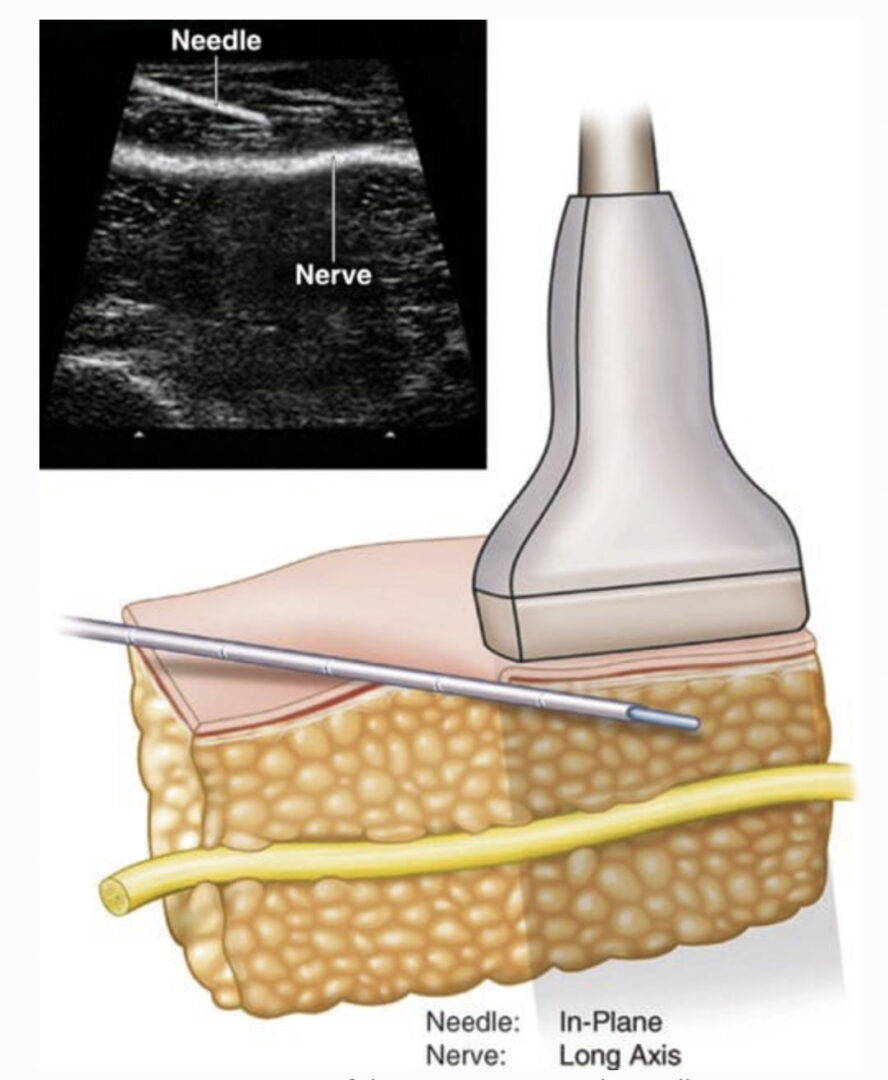
9. ULTRASOUND-GUIDED PERINEURAL INJECTION
Ultrasound-guided perineural injection of anesthetic and/or corticosteroid can be performed for management of neuropathy. Perineural injection is typically performed with a 25-gauge needle, although a 22-gauge spinal needle may be utilized for deeper nerves. The tip of the needle should be positioned directly adjacent to but not within the epineurium. Test injection with lidocaine should be performed to confirm accurate needle positioning. Circumferential spread of the injectate around the nerve is ideal.