The popliteal block is one of the most useful regional anesthesia procedures ever. Using the all-new NYSORA Compendium of Regional Anesthesia, let’s review this nerve block.
When it comes to the popliteal block, you can perform bunionectomies, Achilles tendon repairs, triple arthrodesis, or anything on the foot, really.
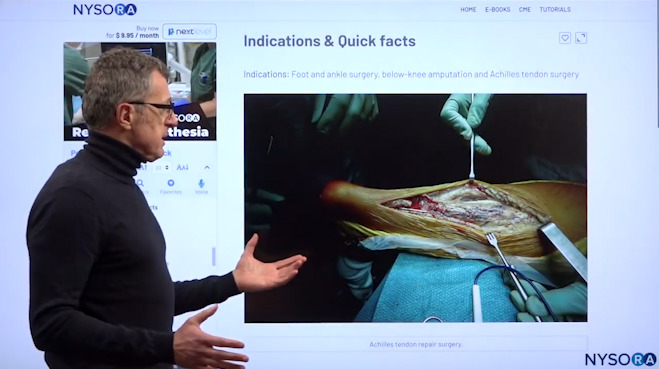
Dr. Hadzic’s favorite indication is the Achilles tendon repair with the patient awake and in the prone position.
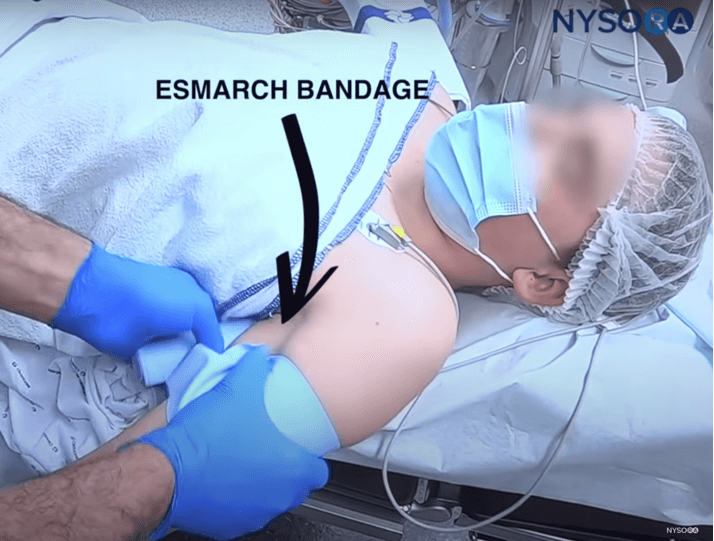
Surgeons can use the tourniquet on the calf which would be preferable, but if unable they will have to use the tourniquet on the thigh, and they can combine the long-acting anesthetic for the popliteal sciatic block with a short-acting anesthetic, such as Lidocaine, for the femoral nerve block, which would basically also eliminate tourniquet pain.
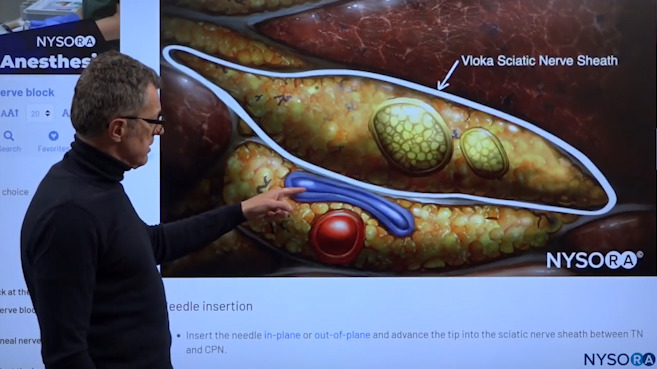
The goal of this technique is to spread the local anesthetic inside the sciatic nerve sheath and the popliteal fossa.
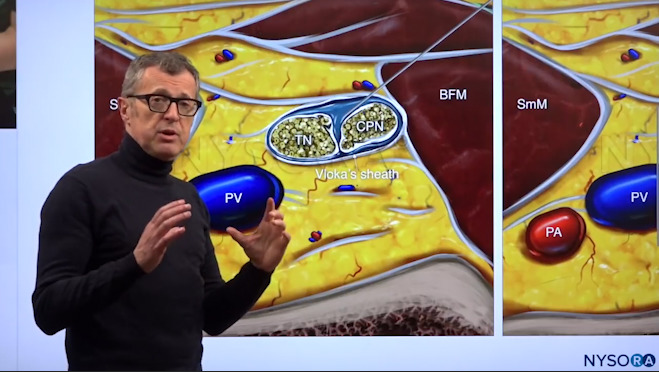
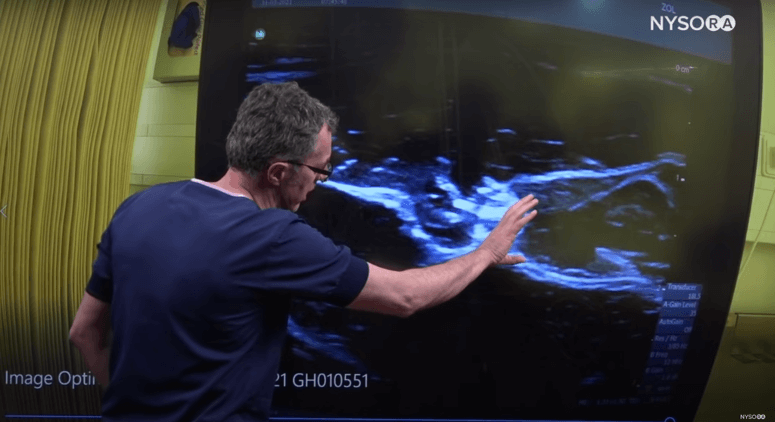
Dr. Hadzic showing the Tibial Nerve(TN) and the Common Peroneal Nerve (CPN).
These tibial and common peroneal nerves are enveloped in a common sheath. The goal of this technique is to find the spot where these two nerves just start to separate in order to place the needle safely in between them and fill that space with the local anesthetic.
This is a very useful trick, you can do this out-of-plane or in-plane; it’s really your choice. But, you really should make your selection not based on what you do best, but what the anatomical configuration of the sciatic nerve in the popliteal fossa is.
Most of the time the popliteal nerve, the two nerves, the tibial and common peroneal are very superficial in the popliteal fossa. So, if they are superficial at about 2-3 centimeters depth, oftentimes it’s much easier to actually do an out-of-plane position and see the two nerves separate.
Dr. Hadzic demonstrating where the needle should be inserted inside Vloka’s sheath for the deposit of local anesthetic.
Tip: If you are injecting here you want to scan proximally because if your injection here results in a spread of the local aesthetic 3, 4, or 5 centimeters proximally in the same sheath, there’s no other place where you could be but in the sciatic nerve sheet, where you want to be.
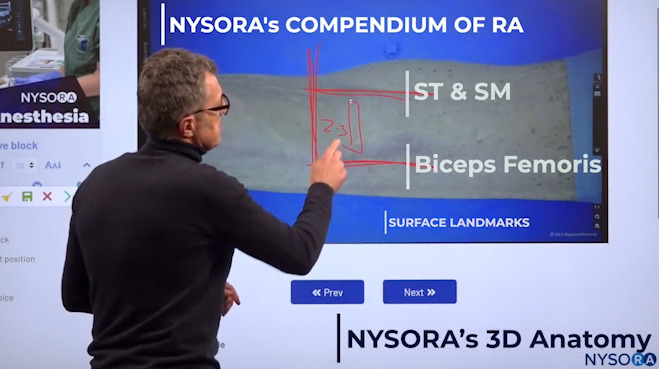
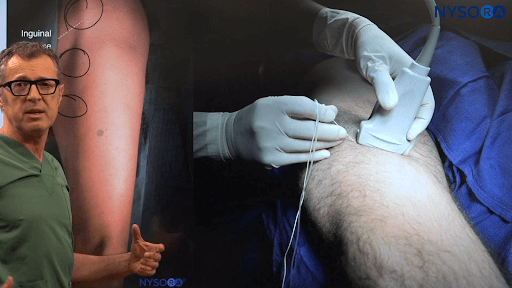
Dr. Hadzic showing the popliteal fossa crease and anatomic surface points where you will be able to see the sciatic nerve.
In the popliteal fossa crease, if you know these anatomical surface points: (1) semitendinosus, (2) semimembranosus muscles, and (3) biceps femoris tendon; all you need to do is to place the transducer at about 2-3 centimeters proximal to the popliteal fossa crease, in between these tendons, usually a little closer to the biceps femoris tendon.
Usually at that location, without searching any further, you will be able to see the sciatic nerve.

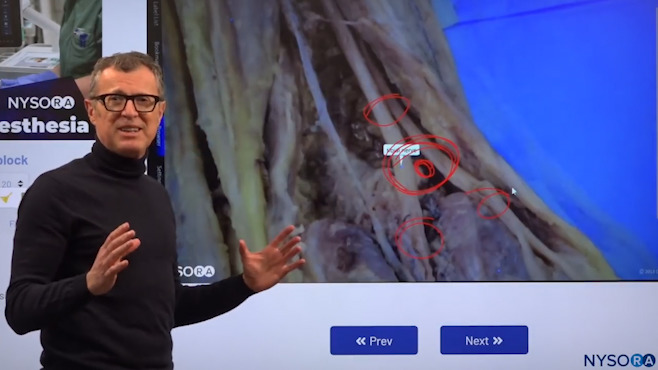
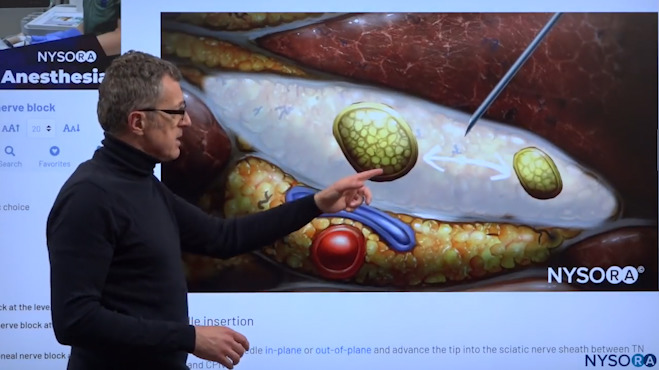
Dr. Hadzic using NYSORA’s 3D Anatomy cognitive aids to show the popliteal fossa space where we can see the two nerves, the tibial nerve, and common peroneal nerve, to inject the local anesthetic.
We’re looking into the popliteal fossa space and what we see is two specific nerves: (1) the tibial nerve, and (2) the common peroneal nerve.
Again, the goal of the technique is to inject the local anesthetic in that space between these two nerves.

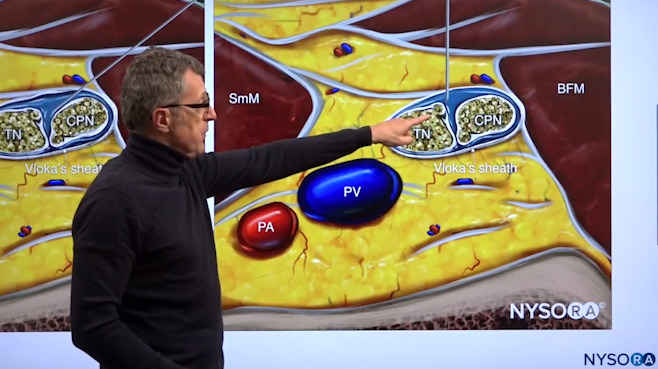
Dr. Hadzic using NYSORA’s 3D Anatomy cognitive aids to show the process of scanning proximally and distally in order to find “the sweet spot” where the injection should occur.
Now, the sweet spot for this nerve block is when you start acquiring images just above the popliteal fossa crease, and then you move your transducer more proximally. Because usually you first see the tibial nerve, and then you’re moving your transducer proximally until you see both of these nerves, the tibial nerve, and the common peroneal nerve. Then you go back more distally until you see these two nerves sufficiently separated by a space where you can inject the local anesthetic inside the sheath that envelops them.
Dr. Hadzic showing the tibial nerve, the common peroneal nerve, and the popliteal artery in the popliteal vein and how the injection will take place in this space.
In another perspective, we can see the tibial nerve, the common peroneal nerve, and the popliteal artery in the popliteal vein. But the point of injection for this block will always be in between the two nerves. So we really want to find that sweet spot where the nerves are together in the sheath, they have not separated yet, but they still have sufficient space in between them so we can easily place the needle between them into the sheath in order to avoid injury and deposit the local anesthetic.
A nerve block is always an injection of local anesthetic in the space that contains the nerves. The popliteal block will provide you with quite large sensory motor coverage. In other words, once you have a popliteal block, you’re going to actually have a foot drop for the duration of the block and quite wide sensory coverage.
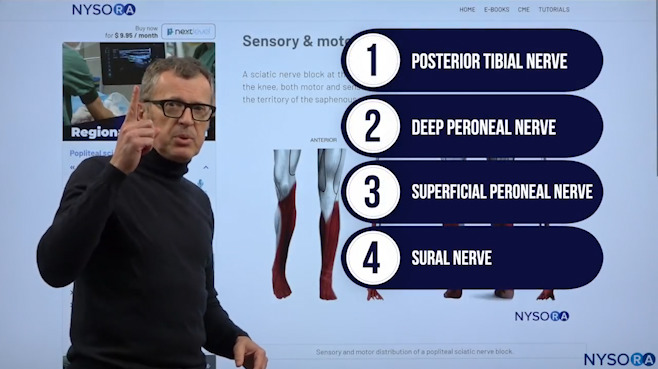
Dr. Hadzic explaining which nerves are covered by the popliteal block.
The popliteal block actually covers four different nerves:
- Posterior Tibial Nerve
- Deep Peroneal Nerve
- Superficial Peroneal Nerve
- Sural Nerve
The only nerve that we don’t cover with the popliteal block that involves innervation of the foot and the leg below the knee is the saphenous nerve.
Popliteal block patient and transducer position.
We start scanning just above the popliteal fossa crease. The idea is that once we localize the tibial nerve, we want to follow that tibial nerve more proximally when it joins the common peroneal nerves. Because the two nerves are joined together into a common sheath and it is in that common sheath that we inject the local anesthetic.
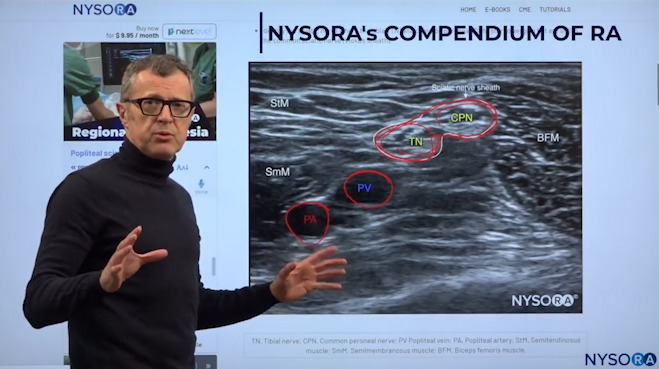
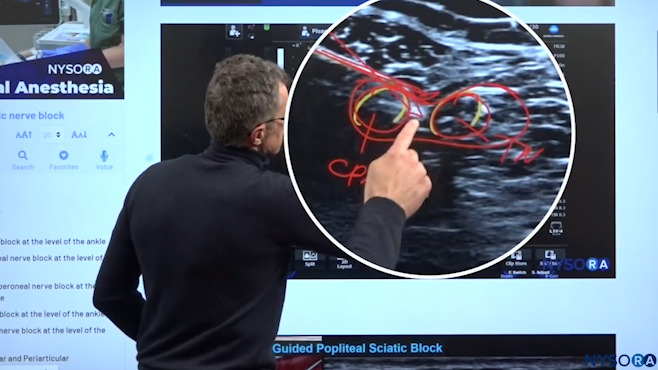
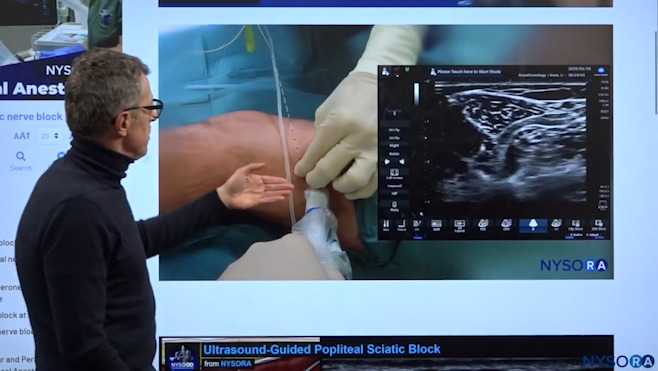
Dr. Hadzic demonstrating the relevant anatomy for the popliteal block on an ultrasound image.
In the sheath of the sciatic nerve, we can find the tibial nerve and the common peroneal nerve. These two nerves are always enclosed in Vloka’s sheath, and underneath you have the popliteal vein which is more superficial, and the popliteal artery. The one thing that you should remember is that in large or obese patients, or in patients who have varicose veins, it is not uncommon to find additional veins inside the popliteal sheath. So always watch for it and use a color doppler before you perform the block.
Dr. Hadzic explaining the sciatic nerve sheath using NYSORA’s proprietary Reverse Ultrasound Anatomy cognitive aids.
Using these new and advanced teaching tools, you can go back and forth between the ultrasound image and the Reverse Ultrasound Anatomy illustration as many times as you need to until you ingrain the sonoanatomical patterns. As you can see in the above image, there is the tibial nerve, the common peroneal nerve, and underneath and outside of the sheath is the popliteal vein and the popliteal artery which you definitely want to avoid.
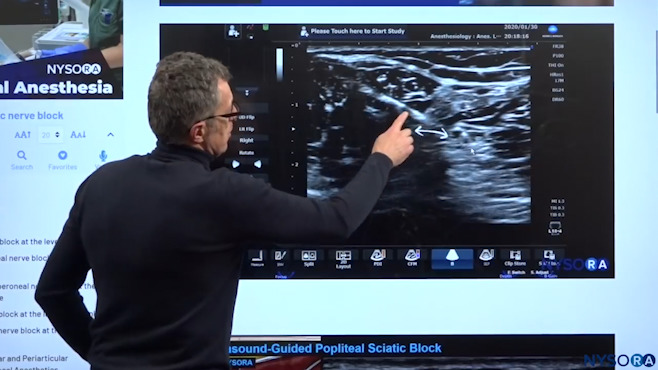
Needle insertion and local anesthetic spread inside Vloka’s sheath.
This is a needle insertion using an in-plane technique. We placed the needle inside the sheath and now we’re going to start injecting the local anesthetic. The local anesthetic injection will always fill that sheath, as well as separate these two nerves as the local aesthetic makes its way inside the sheath. You can see that separation when you sonogram more proximally and is actually what you want to see, as it’s a 100% sign that you are inside the sciatic nerve sheath.
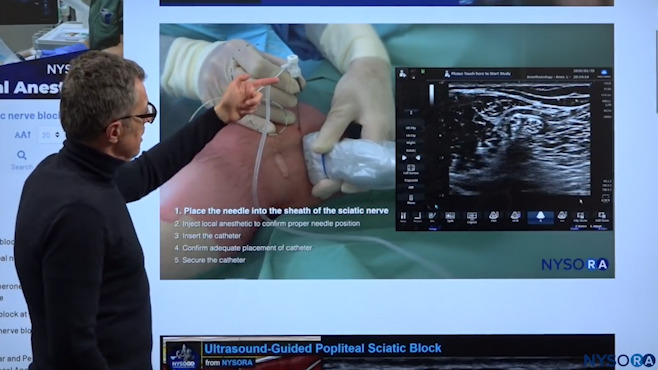
Every continuous nerve block technique consists of five specific steps, discussed in detail below.
Here we can see the pre-loaded needle catheter system that is entering in an in-plane orientation. While watching the ultrasound image, we can see the needle approaching the sciatic nerve in the popliteal sheath. So the needle is almost there now and we can see the common peroneal nerve and the tibial nerve here, but we are now negotiating our way between those two components through the sheath which we have dented now. So what we see here is that the needle has made its way through the sciatic sheath and the sciatic sheath is now indented.
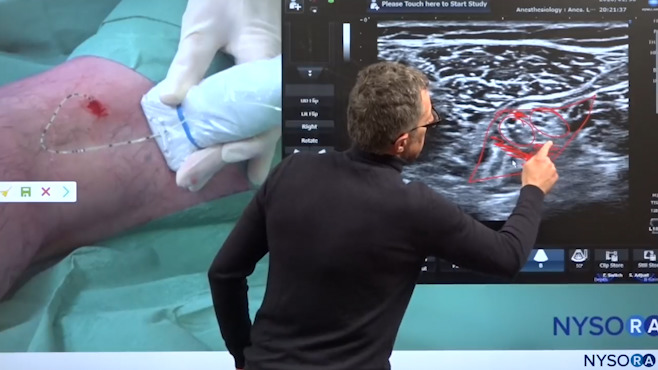
Dr. Hadzic reiterating exactly where the needle insertion and injection of local anesthetic should take place for the popliteal block.
As we can see in the image above, there is the tibial nerve and the common peroneal nerve, and our goal is to enter into the sheath between those two nerves without injuring them. So what we do is, once we get to this point between the two nerves, we want to increase the angle of the needle to force the needle through the sheath, inside the sheath, in between those two nerves.
Every continuous nerve block technique consists of five specific steps:
- Placing the needle inside the sheath;
- An injection that confirms the tip of the needle position;
- Passage of the catheter inside the sheath;
- Injections to the catheter to confirm that we are now inside the sheath injecting; and
- Taping the catheter and securing it to the skin.
Dr. Hadzic showing Step #2, i.e. Injection that confirms the tip of the needle position.
You oftentimes perceive a really very distinct click or a give as the needle makes its way inside the sheath. So that’s the injection of the local anesthetic and we can see how the two nerves now distance from each other as you inject the local aesthetic, which basically proves that the needle tip is inside the sheath, which was Step #2.
Dr. Hadzic showing Step #3, i.e. Passage of the catheter inside the sheath.
The needle and the transducer are stabilized, and once you get experienced you don’t even have to use the transducer. The catheter goes in. The goal is to place the catheter at least 5 cm inside the sheath.
Dr. Hadzic showing Step #4, i.e. Injections to the catheter to confirm that we are now inside the sheath injecting.
We want to inject the local anesthetic through the catheter, and that is the injection of the local anesthetic. We are now above the bifurcation, and these two nerves (Tibial and Common Peroneal Nerve) are together here. But we can see how the local anesthetic has spread substantially inside the sheath that contains the nerve. That was the catheter replacement for the popliteal nerve block.
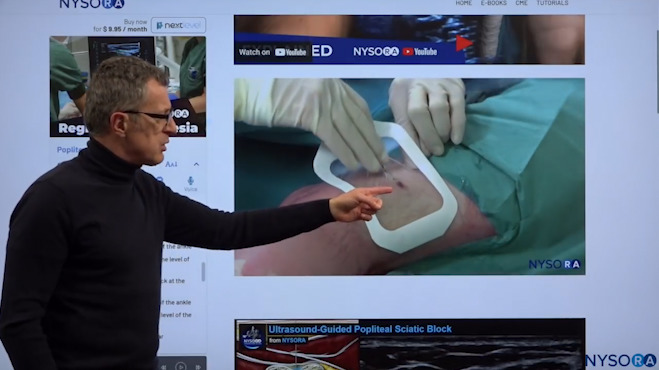
Dr. Hadzic explaining how we seal the hole of the catheter entry to secure leakage.
So what is left to do is to secure the catheter so it doesn’t fall out. First, we clean off the excess gel and apply a derma bond at the point of catheter entry. This is important because it seals the hole, because the catheter is smaller than the needle, and therefore the needle makes a bigger hole than the catheter. When you inject local anesthetic or infuse it, there tends to be leakage around the hole. That is why we use the glue, not to glue the catheter, but actually to seal that hole. We usually apply Tegaderm or some other dressing, and a port for infusion of the local anesthetic, we’re going to place it on the lateral side so it does not interfere with the patient’s positioning or ambulation.