Cervicogenic headache (CGH) is a challenging clinical condition that straddles the boundaries of neurology, pain management, and musculoskeletal medicine. Though often misdiagnosed as migraine or tension-type headache, CGH originates from the cervical spine and can cause persistent, disabling head pain that radiates from the neck to the occipital, temporal, or even orbital regions.
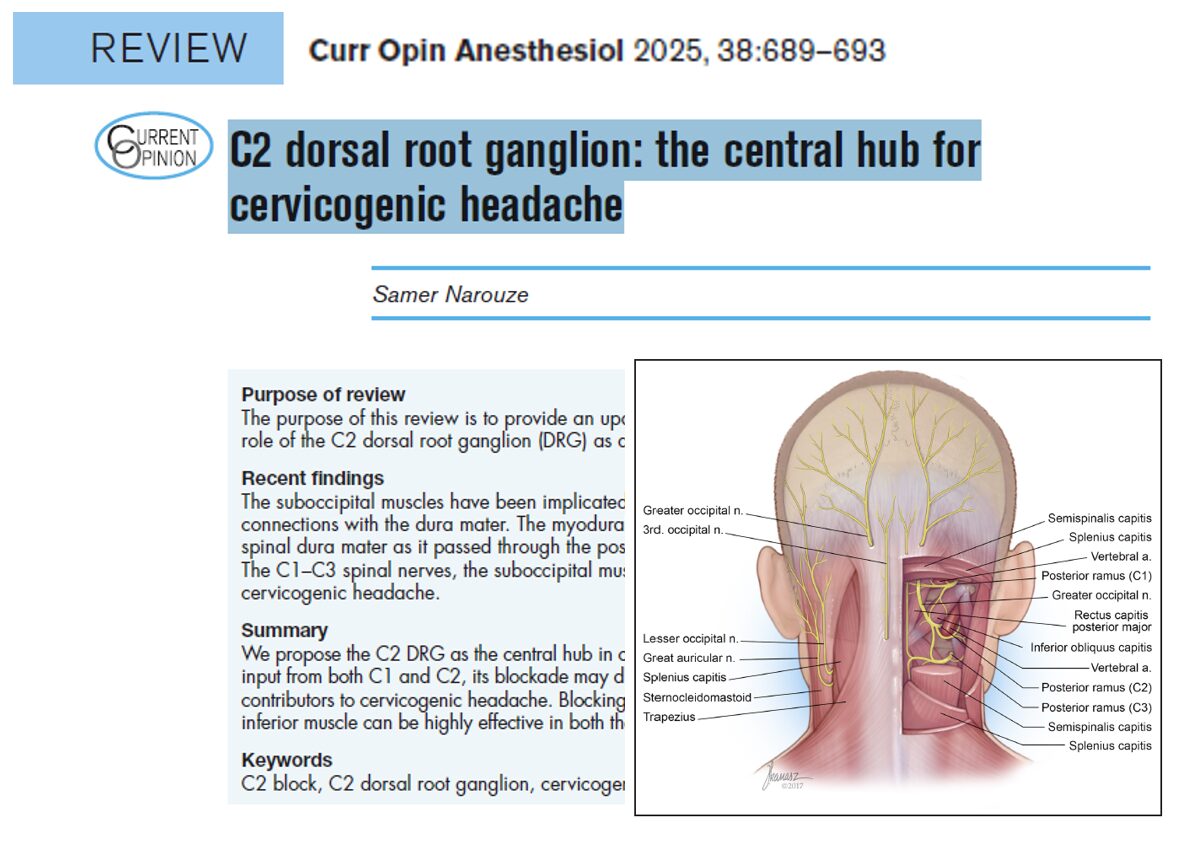
In a landmark review published in Current Opinion in Anesthesiology, Dr. Samer Narouze consolidates decades of anatomical and clinical research to position the C2 dorsal root ganglion (DRG) as the central hub for both the pathogenesis and treatment of CGH. His review emphasizes the importance of the C2 DRG, myodural bridges (MDBs), and suboccipital musculature in understanding and managing cervicogenic headaches.
What is a cervicogenic headache?
Cervicogenic headache is defined as head pain referred from a source in the cervical spine, typically the upper three cervical nerves (C1–C3). It is often unilateral, non-throbbing, and provoked by neck movement. The International Classification of Headache Disorders, 3rd edition (ICHD-3) provides clear criteria for diagnosing CGH, including:
- Radiological or clinical evidence of cervical pathology
- Temporal relationship between the cervical lesion and headache onset
- Symptom resolution with local anesthetic blocks
- Pain provoked by neck movements or pressure on cervical structures
Epidemiology and clinical impact
- General population prevalence: 0.4% to 2.5%
- Prevalence in chronic headache patients: Up to 20%
- In patients undergoing cervical spine surgery: 21% meet CGH criteria
Given these figures, CGH is likely under-recognized and undertreated, particularly in patients labeled with chronic migraines or non-specific headaches.
Clinical features of CGH
Distinctive signs include:
- Occipital pain that may radiate anteriorly
- Side-locked headache (consistently one-sided)
- Pain aggravated by neck movement or sustained posture
- Reduced cervical range of motion
- Tenderness over C2–C3 joints or suboccipital muscles
Common mimics include:
- Migraine (due to overlapping distribution)
- Tension-type headache
- Occipital neuralgia (may coexist)
Why is the C2 DRG central to CGH?
The C2 DRG receives sensory afferents from both C1 and C2, placing it at the anatomical crossroads of multiple headache generators.
It influences pain from:
- Atlanto-occipital joint
- Atlanto-axial joint
- C2–C3 zygapophyseal joint
- Suboccipital muscles
Anatomical position
- Located within the C2 foramen, bordered by the atlas (C1) and axis (C2)
- Occupies nearly 75% of the foramen’s height, making it vulnerable to compression or irritation
- Closely associated with the greater occipital nerve (GON)—a major contributor to CGH
Key anatomical players in CGH
- The trigeminocervical complex (TCC)
- A region in the upper spinal cord where trigeminal and cervical afferents converge
- Explains how cervical pathology can cause pain perceived in the forehead, orbit, and temples
- The greater occipital nerve (GON)
- A medial branch of the C2 dorsal ramus
- Frequently involved in CGH and occipital neuralgia
- GON stimulation increases central sensitization to cervical inputs
- Myodural bridges (MDBs)
- Connective tissue structures linking suboccipital muscles to the dura mater
- May transmit mechanical tension to the intracranial dura, triggering or sustaining headache
Diagnostic and interventional strategy
The role of diagnostic blocks:
- C2 DRG block offers high diagnostic accuracy:
- Sensitivity: 0.743
- Specificity: 0.999
- Also serves as a therapeutic intervention, offering both symptom relief and diagnostic clarity
- Advanced imaging (e.g., diffusion tensor imaging) shows that C2 DRG abnormalities correlate with headache severity
Diffusion tensor imaging findings:
- FA values at the symptomatic C2 DRG are significantly reduced
- Apparent diffusion coefficients (ADC) are increased
- Supports neuroinflammation or structural disruption in CGH patients
The myodural bridge complex: structure and significance
What are MDBs?
- MDBs are fibrous structures originating from:
- Rectus capitis posterior minor
- Obliquus capitis inferior (OCI)
- Nuchal ligament
- They attach to the spinal dura mater through the atlanto-occipital and atlanto-axial spaces
Proposed functions:
- Stabilize the dura during head movement
- Prevent infolding of the dura
- Transmit mechanical forces to the dura mater
Clinical implications:
- Overactivity or tension in suboccipital muscles → dural traction → headache
- Severing MDBs experimentally abolishes CSF pressure changes during muscle stimulation
Suboccipital plane block: a practical approach
Developed by Dr. Narouze, the suboccipital plane block (SOB-2) is designed to target:
- The C2 DRG
- The MDBs beneath the obliquus capitis inferior (OCI) muscle
Technique summary:
- Patient position: Prone or lateral
- Imaging modality: Ultrasound or fluoroscopy
- Identify landmarks: C1 posterior arch, C2 lamina, OCI
- Needle approach: In-plane or out-of-plane
- Target site: C2 ganglion near the intervertebral foramen
- Injectate: Local anesthetic ± steroid
- Optional: Hydrodissection under OCI to reach MDBs
Alternative: The SOB-1 technique targets the GON superficial to OCI, useful for occipital neuralgia or limited access.
Clinical evidence for C2 DRG and MDB blocks
- Patients receiving SOB-2 reported:
- Improved range of motion
- Reduced headache intensity
- Longer duration of relief compared to GON block alone
- A case series showed consistent results in patients refractory to pharmacologic treatments
Indications:
- Diagnostic confirmation of CGH
- Refractory occipital headaches
- CGH with coexisting neck muscle tension
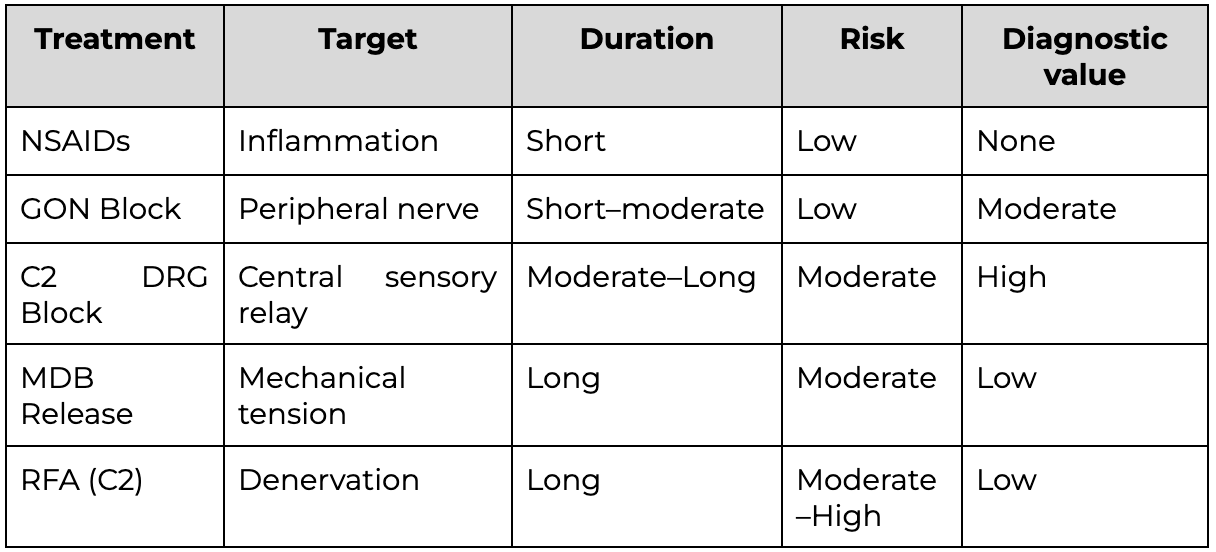
Comparison with other interventions
Limitations and future directions
While promising, current data are limited to small studies and clinical experience. Research gaps include:
- Randomized controlled trials (RCTs) comparing C2 DRG block with other modalities
- Long-term safety and efficacy data
- Standardization of MDB-targeting protocols
- Better understanding of the CSF dynamics affected by MDBs
Best practices for clinicians
- Consider C2 DRG involvement in patients with chronic occipital or posture-sensitive headaches
- Use imaging guidance to improve safety and precision
- Combine C2 DRG and MDB approaches for synergistic relief
- Educate patients on posture, ergonomics, and muscle relaxation techniques
- Collaborate with physical therapists for comprehensive care
Conclusion
The C2 dorsal root ganglion is emerging as the neuroanatomical cornerstone in cervicogenic headache. Its unique position, receiving afferents from C1 and C2, and interfacing with the trigeminocervical system, makes it an ideal target for both diagnosis and treatment.
When coupled with insights into myodural bridge dynamics, clinicians now have a comprehensive model to understand and treat CGH more effectively than ever before.
As interventional pain management continues to evolve, techniques like suboccipital plane blocks and C2 DRG targeting represent the future of personalized, anatomy-driven headache care.
For more information, refer to the full article in Current Opinion in Anaesthesiology.
Narouze S. C2 dorsal root ganglion: the central hub for cervicogenic headache. Curr Opin Anaesthesiol. 2025;38(5):689-693.
For step-by-step guidance on cervicogenic headache treatment and 50+ other techniques, read NYSORA’s Ultrasound-Guided Interventional Pain Manual. For the digital companion to this book, download NYSORA’s Ultrasound Pain App.