Lung transplantation (LTx) remains a life-saving yet complex surgical procedure marked by significant perioperative challenges, one of which is effective postoperative pain control. The surgery often involves large thoracic incisions—typically clamshell or hemi-clamshell—and the placement of multiple chest tubes, which can cause substantial acute and chronic pain. Efficient pain management is crucial, not only for patient comfort but also for promoting early extubation, reducing pulmonary complications, and improving overall recovery.
Traditionally, thoracic epidural analgesia (TEA) has been the gold standard for thoracic surgeries, including LTx. However, increasing reliance on extracorporeal membrane oxygenation (ECMO) during LTx requires systemic anticoagulation, which raises serious safety concerns regarding TEA due to the risk of spinal epidural hematoma. Consequently, the use of regional fascial plane blocks as safer alternatives has gained increasing interest.
This new retrospective exploratory study by Azem et al. investigates the effectiveness of combining superficial parasternal intercostal plane (sPIP) blocks and serratus anterior plane (SAP) blocks with standard systemic analgesia in improving outcomes after LTx.
Study objective and methods
The primary goal of the study was to assess whether the addition of sPIP and SAP blocks to standard anesthetic care could improve tracheal extubation rates and reduce opioid consumption in the first 72 hours postoperatively.
- Design: Single-center, retrospective exploratory study.
- Population: 60 patients undergoing single or double LTx between April 2021 and May 2023.
- Control group (n=35): Received standard anesthesia and systemic multimodal analgesia.
- Intervention group (n=25): Received the same care plus bilateral sPIP blocks and SAP blocks via catheters.
Regional techniques:
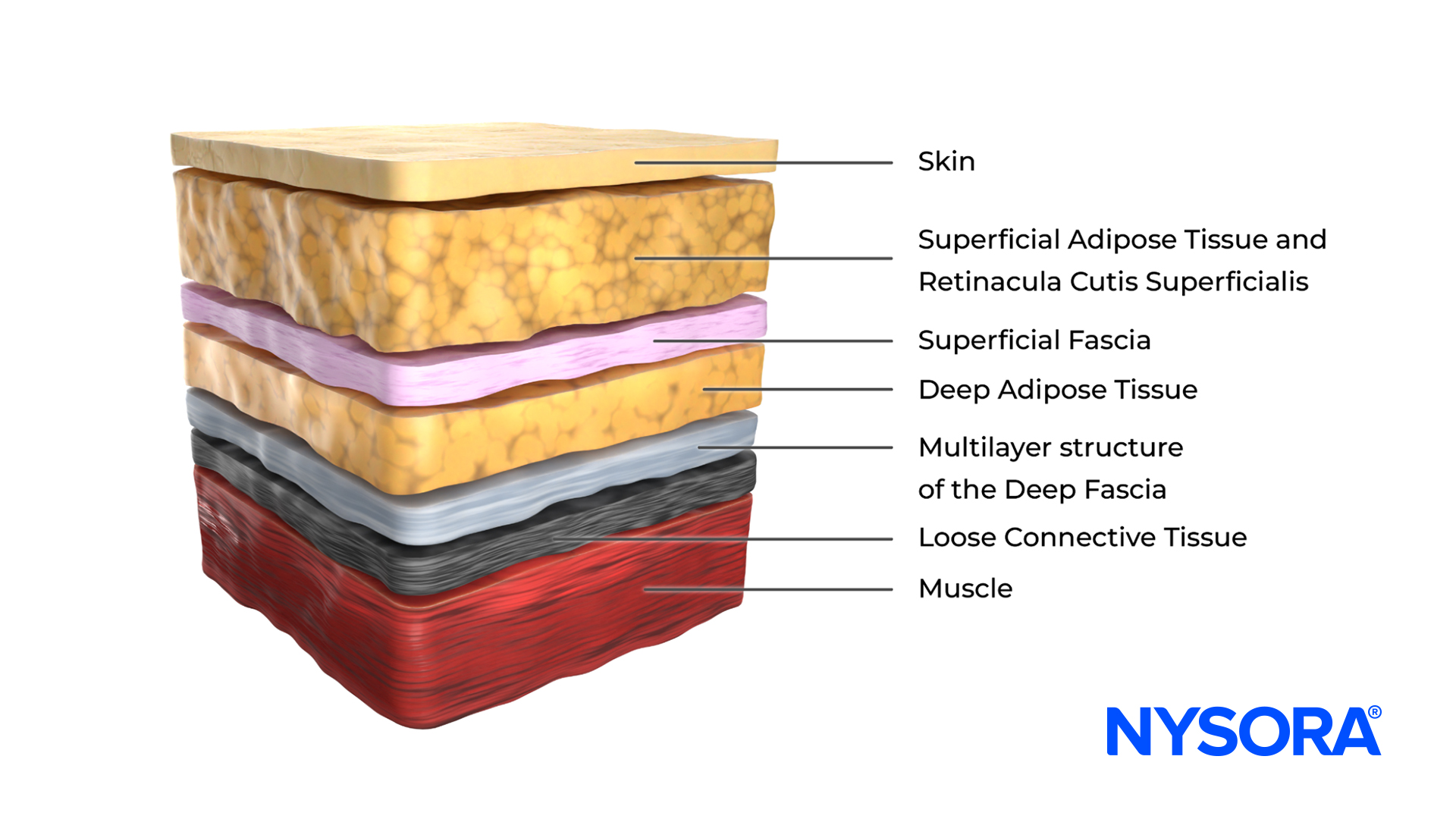
- sPIP block targeted the anterior cutaneous branches of the intercostal nerves for anteromedial chest wall coverage.
- SAP block targeted the lateral branches of intercostal nerves for anterolateral chest wall analgesia.
- Blocks were performed under ultrasound guidance with appropriate volume adjustments based on patient weight.
Outcomes measured:
- Primary: Tracheal extubation rates within 72 hours.
- Secondary: Pain scores using Numeric Rating Scale (NRS) and cumulative oral morphine milligram equivalents (MME) at 24, 48, and 72 hours. Safety data and complications were also analyzed.
Key findings
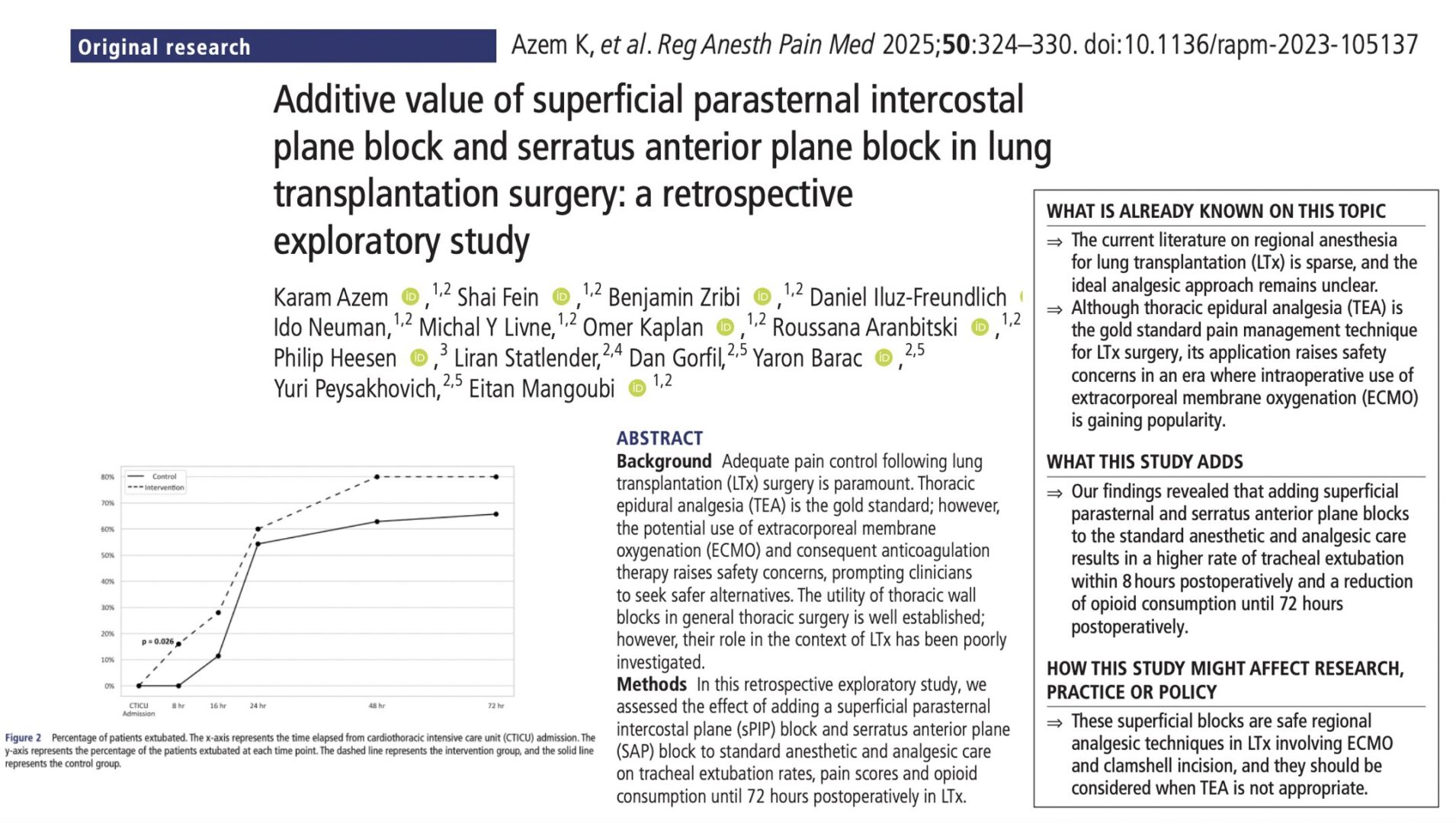
- Early extubation: A significantly higher rate of tracheal extubation was seen at 8 hours post-op in the intervention group (16%) versus none in the control group (p = 0.03). This effect remained statistically significant after adjusting for prognostic factors (p = 0.02). However, no major differences were observed at 24 or 72 hours, likely due to the plateauing of extubation rates beyond 24 hours.
- Opioid consumption: At 0–24 hours, opioid use was significantly lower in the block group (median MME 266 vs. 405; p = 0.02). Cumulative MME was also lower at 48 hours (287 vs. 454; p < 0.01) and 72 hours (318 vs. 549; p < 0.01). Adjusted analysis confirmed the 24-hour difference (p = 0.03), though differences at 48–72 hours were not statistically significant.
- Pain scores: Pain scores remained low and similar in both groups throughout 72 hours (median NRS 1–2), reflecting the strong multimodal regimen and preemptive opioid rescue strategies used across all patients.
- Safety and complications: The addition of blocks was not associated with any adverse events like hematoma or infection. A trend toward fewer complications was observed in the intervention group, including:
-
- Lower rates of reintubation, prolonged ventilation, and CTICU readmission.
- No 30-day mortality in the intervention group versus one death in the control group.
Conclusion
This study provides preliminary evidence that combining sPIP and SAP blocks with systemic analgesia in LTx can facilitate earlier extubation and reduce opioid requirements, without compromising safety—even in patients undergoing ECMO-supported surgeries. The combination of sPIP for medial thoracic coverage and SAP for lateral thoracic coverage offers nearly circumferential chest wall analgesia. When performed with ultrasound guidance, these blocks are technically straightforward and suitable for use even in patients on anticoagulation.
Given that TEA is often contraindicated in this population, these superficial blocks offer a compelling alternative for effective postoperative pain management in lung transplant recipients.
Future research
While the findings are promising, future research should focus on several key areas. Larger, multicenter randomized controlled trials are needed to validate the additive value of sPIP and SAP blocks across varied surgical environments and patient populations. Studies should also explore optimization of technique, including whether block administration is more effective pre- or postoperatively, the comparative value of catheters versus single-shot approaches, and the ideal dosing strategies. Incorporating patient-reported outcomes—particularly regarding pain interference with mobility, sleep, and respiratory function—will be crucial to fully understand the clinical impact of these blocks. Lastly, cost-effectiveness analyses should determine whether reduced opioid consumption, shorter ICU stays, and fewer complications translate into measurable financial and resource savings for healthcare systems.
For more detailed information, refer to the full article in RAPM.
Azem K et al. Additive value of superficial parasternal intercostal plane block and serratus anterior plane block in lung transplantation surgery: a retrospective exploratory study. Reg Anesth Pain Med. 2025;50:324-330.
Download the Nerve Blocks App HERE for in-depth insights on the serratus anterior plane block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Block Manual Module on NYSORA360!