Hemorrhagic shock remains a leading cause of preventable mortality in trauma, demanding rapid and effective resuscitation strategies. Yet the optimal approach to volume replacement in this context remains controversial. Over the past two decades, clinical guidelines have moved markedly away from liberal fluid administration toward more restrictive resuscitation strategies, reflecting concerns over iatrogenic complications such as dilutional coagulopathy, hypothermia, acidosis, and organ dysfunction. The 2025 review by Markl-Le Levé et al. provides a timely synthesis of the evolving evidence, physiological rationale, and clinical controversies surrounding resuscitation fluid choice. It underscores the ongoing transition from aggressive crystalloid and colloid use to more targeted, physiologically grounded strategies based on patient-specific needs and pathophysiologic context.
Methods
This article is a narrative literature review synthesizing contemporary research, guideline recommendations (notably the 2023 European Trauma Guidelines), and key trials investigating fluid resuscitation modalities in trauma-associated hemorrhagic shock. It evaluates the efficacy and safety profiles of:
- Crystalloids (balanced vs. unbalanced)
- Synthetic colloids (hydroxyethyl starch, gelatin)
- Natural colloids (albumin)
- Blood products and plasma derivatives
The review considers pathophysiological mechanisms such as the “lethal triad of trauma” (hypoperfusion, acidosis, coagulopathy), endothelial dysfunction, and trauma-induced coagulopathy (TIC), which heavily influence resuscitation efficacy and risks.
The physiological basis: the lethal triad and trauma-induced coagulopathy
At the heart of hemorrhagic shock lies the lethal triad—hypoperfusion, acidosis, and coagulopathy—which perpetuates a downward spiral of tissue injury, inflammation, and hemostatic failure. The review highlights the increasingly appreciated role of endotheliopathy and systemic inflammation in triggering trauma-induced coagulopathy (TIC), a condition that resists simple correction via volume expansion alone.
TIC is driven by several overlapping mechanisms:
- Hypoperfusion-induced activation of the protein C pathway
- Hyperfibrinolysis and clotting factor depletion
- Platelet dysfunction and impaired thrombin generation
- Disruption of fibrin polymerization
These insights necessitate a shift away from purely volumetric resuscitation targets toward strategies that also consider coagulopathy and microcirculatory integrity.
Crystalloids: foundational yet limited
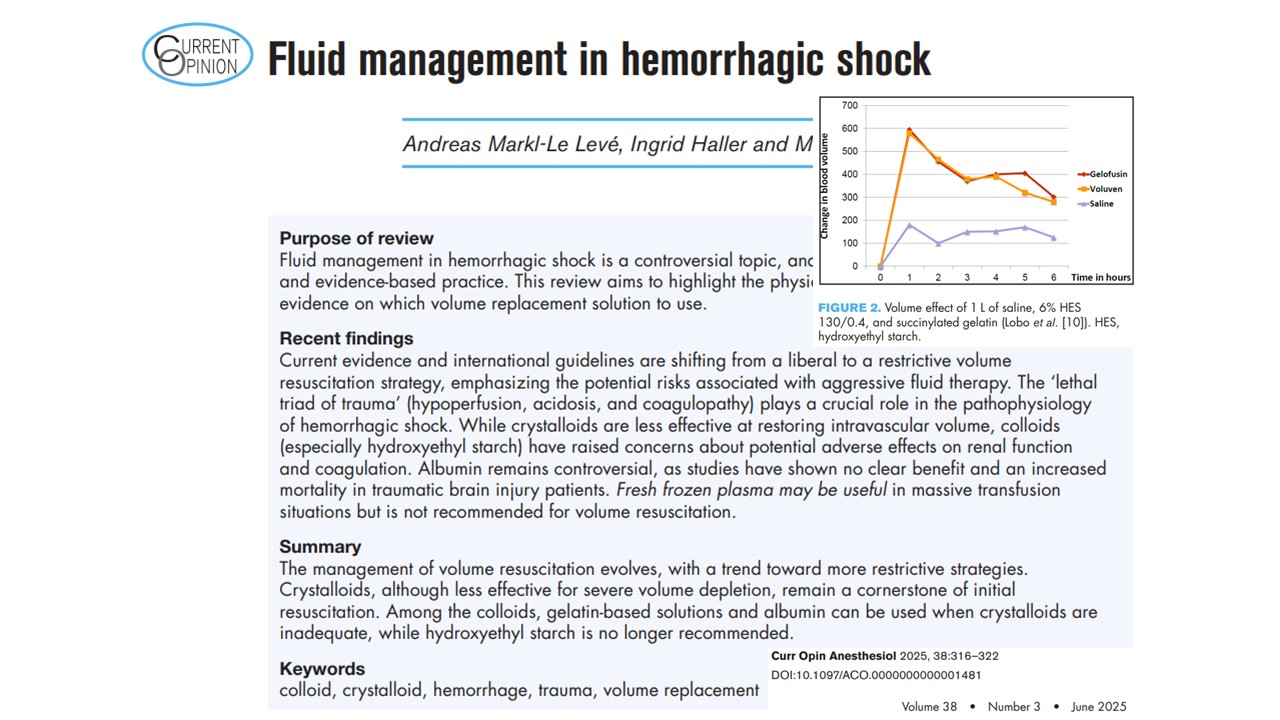
Crystalloids, especially balanced formulations, remain first-line agents for initial resuscitation due to their accessibility, low cost, and familiarity. However, their limitations are well-documented:
- Poor intravascular retention: Only ~18% remains intravascular 20 minutes post-infusion
- Risk of tissue edema: May exacerbate compartment syndromes and impair organ perfusion
- Dilutional coagulopathy: Large volumes dilute clotting factors and fibrinogen
- Hyperchloremic acidosis: Associated with saline-based fluids
Balanced crystalloids, such as lactated Ringer’s or Plasma-Lyte, are increasingly preferred over normal saline. Studies show they better preserve acid–base balance and mucosal perfusion, although conclusive mortality benefits remain elusive.
Colloids: controversy and caution
Hydroxyethyl starch (HES)
Once a mainstay in trauma resuscitation, HES has fallen out of favor due to associations with:
- Acute kidney injury (AKI)
- Impaired coagulation, particularly fibrin polymerization
- Increased mortality in sepsis
Nevertheless, the FIRST trial suggests that HES may retain a role in hemorrhagic shock, where it improved renal function and lactate clearance compared to saline. These benefits, however, must be weighed against:
- Tissue accumulation
- Dose-dependent toxicity
- Regulatory restrictions
The review concludes that HES is no longer recommended due to its overall risk profile.
Gelatin-based colloids
Gelatin solutions have a long history and a more favorable safety profile than HES. Advantages include:
- No tissue storage
- Lower risk of renal toxicity
- Rapid clearance
Pharmacodynamically, succinylated gelatin offers a sustained volume effect and modest impact on coagulation compared to HES. However, it still interferes with fibrin cross-linking and may impair clot integrity. There is also a low but present risk of anaphylaxis (especially with urea-linked formulations like Haemaccel, now obsolete). The GENIUS trial found no renal harm from gelatin in septic patients, but conclusive trauma-specific data remain limited.
Albumin: natural colloid, unnatural fit for trauma
Albumin, a natural plasma protein with oncotic properties, offers benefits in maintaining intravascular volume and modulating inflammation. However, its use in trauma has been curbed by several concerns:
- Increased mortality in traumatic brain injury
- Dilutional coagulopathy is similar to synthetic colloids
- High cost and limited availability
- Lack of a clear survival benefit in trauma
Due to these factors, albumin is not recommended for routine volume resuscitation in hemorrhagic shock and may be contraindicated in TBI.
Plasma and blood products: targeted use, not routine volume therapy
Fresh frozen plasma (FFP) has utility in massive transfusion protocols where clotting factor replacement is critical. However:
- FFP is not advised solely for volume resuscitation
- Risks include TRALI, TACO, and immunologic complications
- Evidence for mortality benefit in prehospital use is mixed
Emerging evidence favors the use of coagulation factor concentrates over FFP for targeted hemostatic support. Factor concentrates offer:
- Precise dosing
- Reduced volume load
- Lower immunologic risk
The RETIC trial, which compared FFP with factor concentrates, was halted early due to a higher incidence of multiple organ failure in the FFP arm.
Summary of resuscitation options
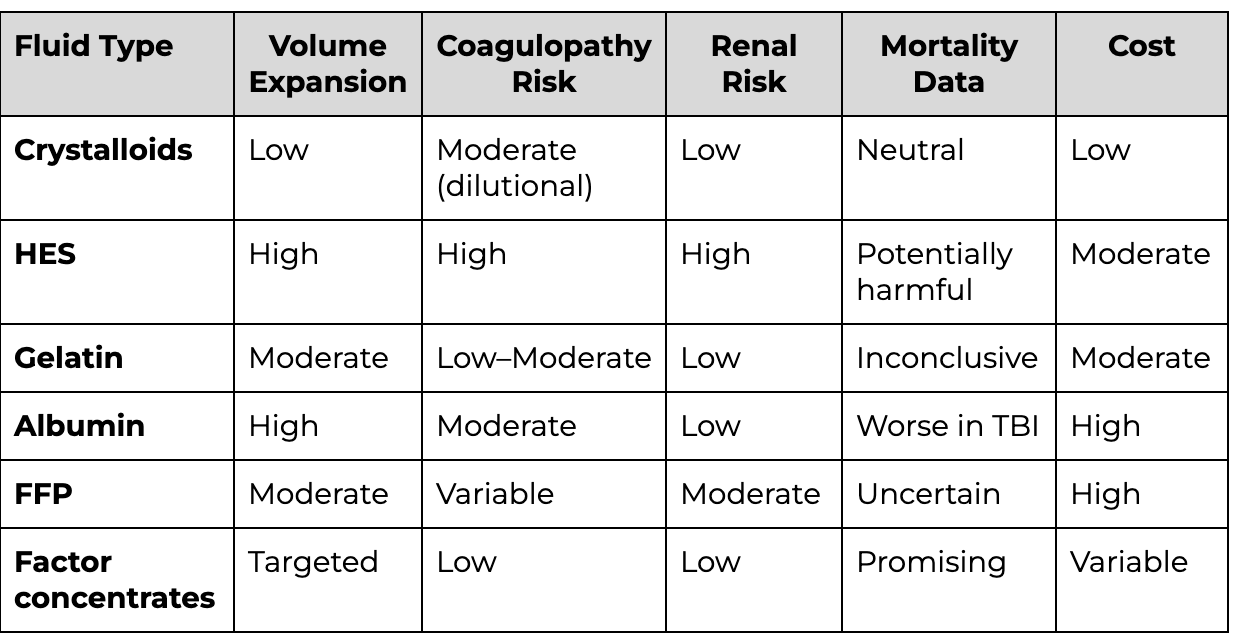
TBI = traumatic brain injury; FFP = fresh frozen plasma; HES = hydroxyethyl starch
Limitations and knowledge gaps
Despite significant progress in understanding fluid resuscitation in hemorrhagic shock, several limitations persist:
- Lack of trauma-specific RCTs: Many current recommendations are extrapolated from septic shock studies.
- Variable fluid composition: Not all colloids or crystalloids are equal; studies often group dissimilar fluids together.
- Heterogeneity of trauma: Blunt vs. penetrating trauma, isolated hemorrhage vs. polytrauma, and presence of TBI complicate generalizability.
- Coagulation assessment: Standard lab tests are inadequate for dynamic assessment; point-of-care tools (e.g., ROTEM, TEG) are underutilized.
- Prehospital vs. in-hospital strategies: The timing of intervention influences outcomes but remains underinvestigated.
- Regional variation in trauma systems: Differences in prehospital care, transfusion protocols, and injury patterns complicate the interpretation of findings.
Future directions
To improve fluid resuscitation in hemorrhagic shock, future research must:
- Conduct high-quality, trauma-specific RCTs to define optimal fluid types, timing, and volumes.
- Develop dynamic resuscitation endpoints using real-time hemodynamic and coagulation monitoring.
- Personalize therapy based on patient physiology, injury type, and coagulopathy status.
- Explore novel plasma products such as freeze-dried plasma or synthetic oxygen carriers for field use.
- Integrate machine learning into resuscitation algorithms to support decision-making in complex trauma scenarios.
Conclusion
The management of fluid resuscitation in hemorrhagic shock is undergoing a critical transformation. The once-dominant practice of aggressive fluid replacement has yielded to a more nuanced, restrictive, and physiology-guided approach. While crystalloids remain the foundation of initial resuscitation, their limitations necessitate adjunctive strategies in severe hypovolemia. Among colloids, gelatin-based solutions appear to offer a reasonable compromise between efficacy and safety, though definitive trauma-focused data are lacking. Albumin and HES, once favored, have been largely abandoned due to safety concerns.
Blood products, particularly coagulation factor concentrates, are increasingly recognized for their role in correcting TIC without the downsides of plasma overload. Yet, many clinical decisions still rely on institutional preferences and incomplete evidence.
This review reaffirms the importance of individualized, evidence-based fluid management in the treatment of hemorrhagic shock. Until more definitive data emerge, clinicians must balance the benefits of intravascular volume restoration against the risks of exacerbating coagulopathy, organ dysfunction, and adverse outcomes. A cautious, targeted resuscitation strategy—guided by physiology rather than fixed volumes—remains the most prudent path forward.
For more information, refer to the full article in Current Opinion in Anesthesiology.
Markl-Le Levé A, Haller I, Bachler M. Fluid management in hemorrhagic shock. Curr Opin Anaesthesiol. 2025 Jun 1;38(3):316-322.
Read more about fluid management in our Anesthesiology Manual: Best Practices & Case Management.