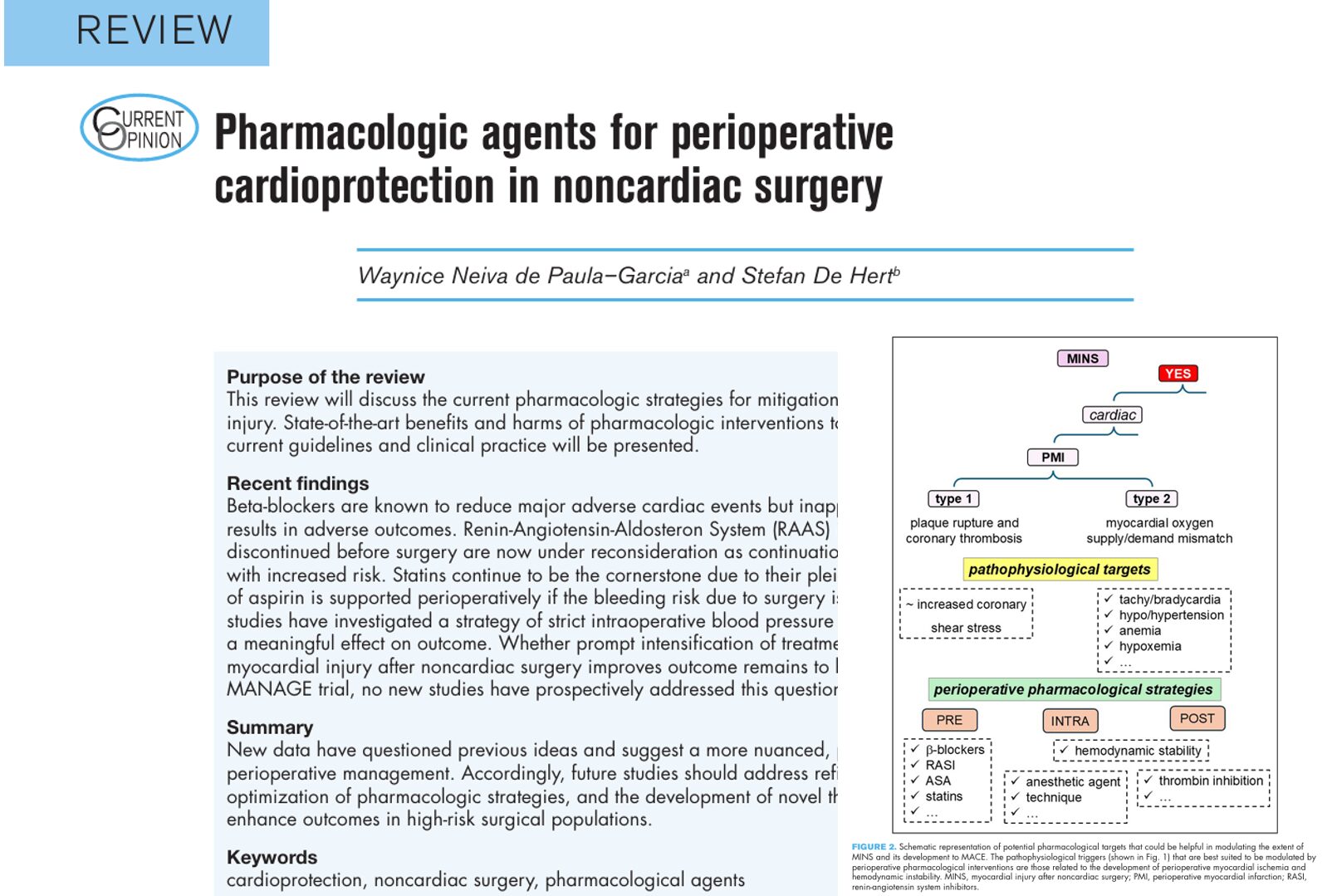
In recent years, the focus on preventing cardiac complications in patients undergoing noncardiac surgery has intensified. Myocardial injury after noncardiac surgery (MINS) is now recognized as a significant contributor to postoperative morbidity and mortality. With an incidence rate as high as 20%, MINS has emerged as a silent yet serious threat, often without obvious symptoms, only detectable by cardiac biomarkers like troponin.
A recent in-depth review by de Paula–Garcia et. al provides critical updates on pharmacologic strategies for perioperative cardioprotection. This news post provides a comprehensive summary of current practices, emerging evidence, and expert recommendations.
What is myocardial injury after noncardiac surgery (MINS)?
MINS is defined as isolated postoperative elevations in cardiac troponin (cTn) levels within 30 days after surgery, typically without the classical symptoms of myocardial infarction (MI).
Key facts:
- Occurs in ~20% of noncardiac surgical patients.
- Associated with increased risk of major adverse cardiac events (MACE) and higher 1-year mortality.
- Detection relies entirely on perioperative cTn monitoring, as MINS is often clinically silent.
Understanding the pathophysiology
MINS results from a variety of underlying triggers, broadly categorized into:
- Cardiac causes: Type 1 or Type 2 MI, tachyarrhythmia, acute heart failure.
- Extracardiac causes: Sepsis, stroke, pulmonary embolism.
Implication:
Treatment must be tailored based on the etiology, as outcomes and interventions vary widely depending on the root cause.
Key pharmacologic strategies for perioperative cardioprotection
1. Beta-blockers
- Benefits: Reduce heart rate, myocardial oxygen demand, and MACE risk.
- Risks: Inappropriate initiation can lead to hypotension and bradycardia.
- Guideline advice: Continue pre-existing therapy; avoid new initiation immediately before surgery.
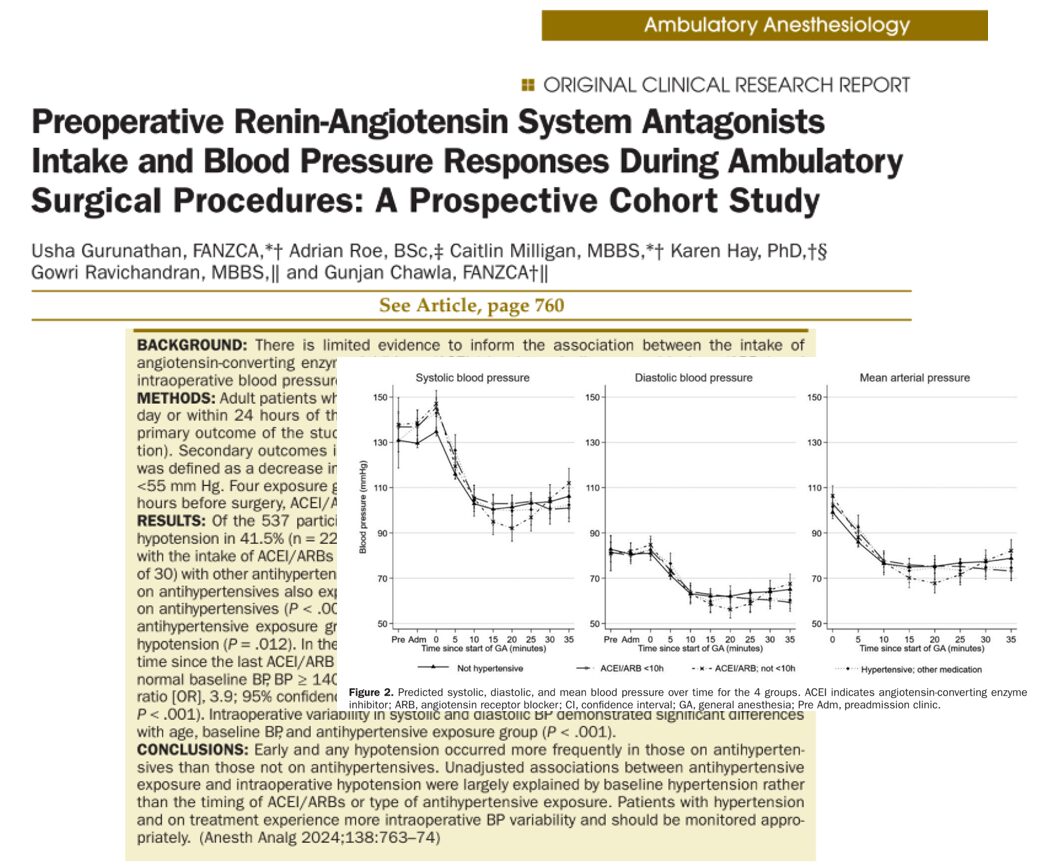
2. Renin-angiotensin system inhibitors (RASI)
- Previously advised to be stopped preoperatively due to risk of hypotension.
- New evidence suggests continuation does not increase postoperative complications.
- Clinical trials (e.g., SPACE and STOP-OR-NOT) support re-evaluation of outdated guidelines.
- Recommendation: Adopt a personalized approach based on patient stability and comorbidities.
3. Statins
- Offer lipid-lowering, anti-inflammatory, and plaque-stabilizing effects.
- Strongly recommended to continue perioperatively.
- Discontinuation may increase the risk of inflammatory response and cardiac events.
4. Aspirin
- Balancing thrombotic risk vs. bleeding is essential.
- Guidelines recommend continuation if the bleeding risk is low to moderate.
- Supported by studies showing reduced MACE without significant bleeding (e.g., ASPIRE, ASSURE DES trials).
Step-by-step: optimizing pharmacologic therapy before surgery
- Evaluate cardiovascular history.
- Continue statins and beta-blockers if already prescribed.
- Assess bleeding risk before continuing aspirin.
- Make individualized decisions on RASI continuation.
- Avoid starting new beta-blockers unless absolutely indicated.
Intraoperative strategies: managing blood pressure
- Hypotension is linked to adverse outcomes, but the causality remains uncertain.
- Several trials (e.g., POISE-3, INPRESS) investigated strict BP control strategies:
- Results showed no significant difference in MACE or mortality.
- Some evidence suggests continuous BP monitoring can reduce hypotensive episodes.
- Results showed no significant difference in MACE or mortality.
Bottom line:
- Maintaining hemodynamic stability is crucial.
- Pharmacologic choices alone are insufficient; clinician skill in monitoring and intervention is key.
Postoperative care: Is treatment intensification beneficial?
- Evidence here is still evolving.
- MANAGE trial showed that dabigatran reduced vascular complications post-MINS but raised concerns:
- High dropout rate
- The control group lacked standard therapy (aspirin, statins)
- Mixed thrombotic event types (arterial + venous)
- High dropout rate
Alternative strategies:
- Intensified care with cardiology consults and medication adjustments has shown some benefit.
- However, more trials are needed to standardize this approach.
Conclusion
Pharmacologic cardioprotection in noncardiac surgery is not one-size-fits-all. As the evidence base grows, a personalized, multidisciplinary approach, combining anesthesiology, cardiology, and surgical expertise, is essential.
Clinicians must stay informed, weigh individual patient risks, and adapt based on emerging research. Effective perioperative care isn’t just about the right drugs, it’s about the right decisions, made at the right time.
Reference: Paula-Garcia WN et al. Pharmacologic agents for perioperative cardioprotection in noncardiac surgery. Curr Opin Anaesthesiol. 2025;38:361-368.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant App. Prefer a physical copy? Get the latest literature and guidelines in book format. For an interactive digital experience, check out the Anesthesia Updates Module on NYSORA360!