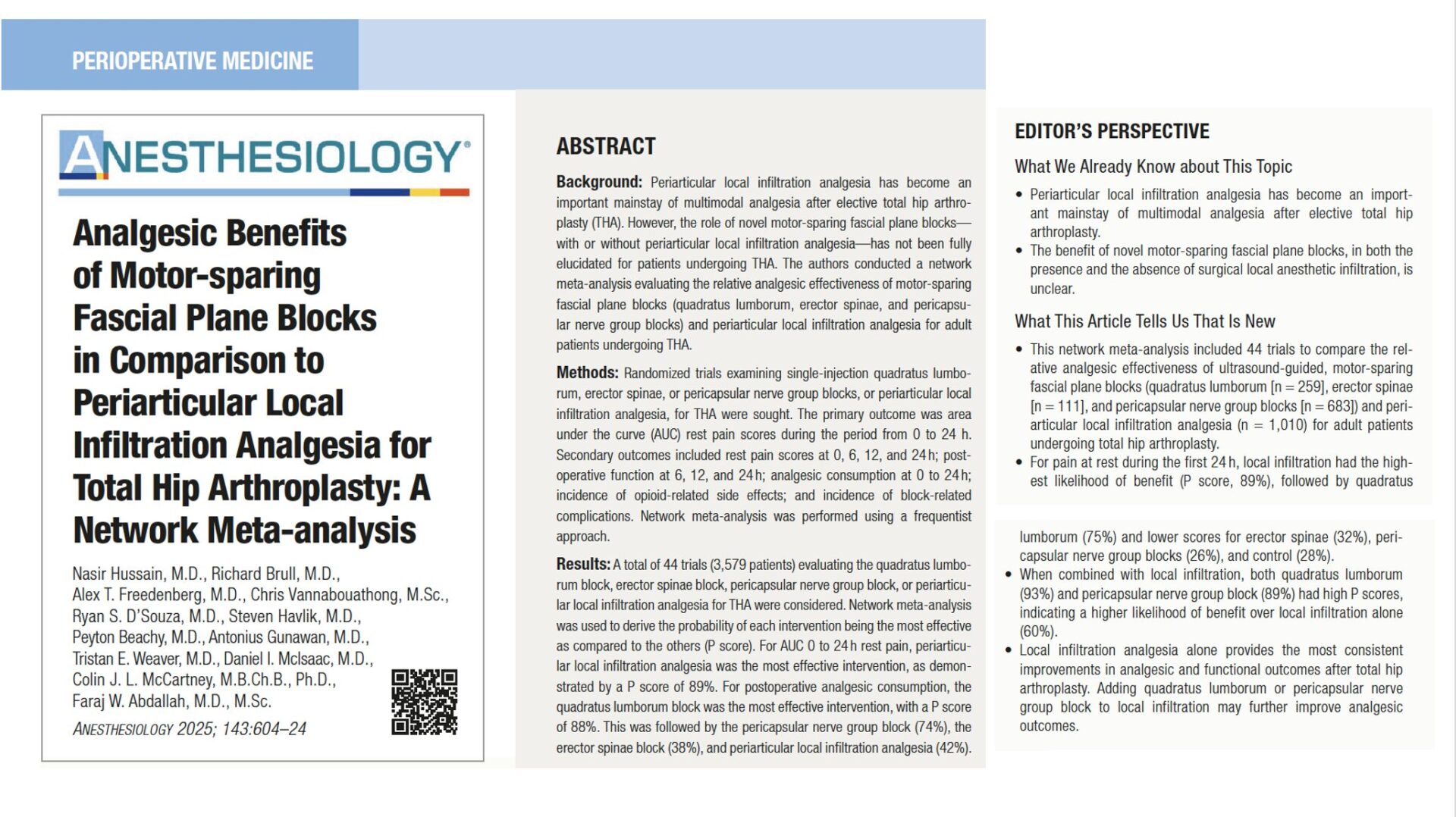
Total hip arthroplasty (THA) is one of the most common orthopedic procedures worldwide, offering substantial improvements in mobility and quality of life. However, managing postoperative pain remains a major challenge. Poorly controlled pain can delay mobilization, increase opioid requirements, and negatively impact recovery.
Traditionally, periarticular local infiltration analgesia (LIA) has been a cornerstone of multimodal analgesia for THA, delivering local anesthetic directly into tissues surrounding the joint. In recent years, novel motor-sparing fascial plane blocks—such as the quadratus lumborum block (QLB), erector spinae plane block (ESPB), and pericapsular nerve group (PENG) block—have gained attention. These ultrasound-guided techniques aim to provide targeted analgesia while preserving motor function, potentially facilitating early ambulation and reducing opioid consumption.
Despite growing popularity, the relative effectiveness of these blocks compared to periarticular infiltration remains uncertain. Previous studies have reported conflicting results, with limited evidence directly comparing multiple techniques. This has made it difficult to establish a standardized regional anesthesia strategy for THA.
To address this knowledge gap, researchers conducted a large network meta-analysis of randomized controlled trials. By comparing LIA and various motor-sparing blocks—alone and in combination—they aimed to clarify which techniques provide the best balance of pain control, opioid sparing, and functional recovery after THA.
Study objective and methods
The primary objective of the meta-analysis was to determine which regional anesthesia strategy—LIA, QLB, PENG block, or ESPB—provides the most effective postoperative analgesia for patients undergoing elective THA. The goal was not only to compare their relative analgesic effectiveness but also to assess whether adding a motor-sparing fascial plane block (QLB or PENG) to LIA yields incremental benefits in terms of pain relief, opioid consumption, functional recovery, and side effect reduction.
- Design: Frequentist network meta-analysis of randomized controlled trials.
- Population: Adults undergoing unilateral or bilateral primary THA. Surgery under either general or spinal anesthesia (rarely with intrathecal morphine).
- Interventions compared:
- LIA: Surgeon-delivered infiltration of local anesthetic ± adjuncts.
- QLB, PENG, ESPB: Single-shot, ultrasound-guided fascial plane blocks.
- Combinations where available (LIA + QLB; LIA + PENG; fewer data for LIA + ESPB).
- Primary outcome: Area under the curve (AUC) of rest pain scores during the first 24 h postoperatively.
- Secondary outcomes: Rest pain at 0, 6, 12, and 24 h; opioid consumption at 0–24 h (oral morphine equivalents); early functional outcomes (6, 12, 24 h); incidence of opioid-related side effects (PONV, pruritus, urinary retention); block-related complications/adverse events.
Key findings
-
Primary endpoint: 0–24 h pain AUC
- LIA ranked highest for improving AUC rest pain vs parenteral analgesia alone (P-score ~ 89%).
- QLB trailed but performed well; PENG and ESPB were less consistent for this composite.
- If your goal is the overall pain burden across day 1, LIA is the most reliable single intervention.
-
Pain at individual time points
- PACU/0–2 h: LIA most likely best (P-score ~ 80%); ESPB sometimes ranked second.
- 6 h: QLB tended to rank highest (P-score ~ 71%).
- 12 h: LIA again led (P-score ~ 79%).
- 24 h: PENG often ranked top (P-score ~ 64%), with QLB and LIA close behind.
- LIA shines early and at 12 h; QLB may strengthen the mid-window (6 h); PENG competes by 24 h.
-
Opioid consumption (0–24 h)
- QLB had the highest likelihood of reducing opioids (P-score ~ 88%), followed by PENG (~ 74%); LIA lagged for this specific endpoint (~ 38%).
- When opioid-sparing is paramount (frailty, high PONV risk), QLB offers the greatest probability of benefit.
-
Early function (6–24 h)
- Mixed instruments pooled.
- PENG most often ranked best at 6 h (or shared high ranking with LIA).
- LIA ranked best at 12 h.
- PENG again led at 24 h (P-score ~93%), with ESPB second and LIA close.
- If you’re targeting early mobility milestones, PENG repeatedly features near the top—especially by 24 h.
-
Combination strategies (exploratory)
- Adding QLB or PENG to LIA yielded higher P-scores than LIA alone (e.g., LIA + QLB ~ 93%, LIA + PENG ~ 89% for AUC).
- Evidence is limited (few trials), but the signal favors stacking in selected patients.
- In high-pain-risk cases (posterolateral approach, opioid-tolerant, high anxiety), LIA + QLB or LIA + PENG may provide incremental gains.
-
Opioid-related side effects
- ESPB ranked best for reducing PONV (P-score ~ 92%); QLB also favorable.
- For pruritus and urinary retention, QLB ranked best with modest certainty.
- If PONV dominates decision-making, ESPB may have a role—though its core analgesic performance was less consistent.
-
Safety and complications
Overall few block-related AEs across > 1,200 patients with reported safety:
- Rare hematomas (QLB, PENG, and even sham).
- Isolated prolonged motor weakness (QLB and ESPB) were rare.
- No signal of increased respiratory depression in any group.
- Single-shot, motor-sparing techniques had low complication rates in trials; standard cautions (coagulopathy, LA dose limits) still apply.
Conclusion
Across 44 randomized trials, periarticular LIA was the most consistent single strategy for reducing overall 0–24 h rest pain and improving early recovery after elective THA. If you need to push opioid sparing, QLB offers the highest probability of reducing 24-h opioid consumption, while PENG frequently optimizes function by 24 h. For many programs, LIA as baseline with selective addition of QLB or PENG in higher-risk cases appears to be a pragmatic, ERAS-aligned pathway. ESPB can be considered in PONV-prone patients, but its core analgesic performance was less consistent.
Future research
- Head-to-head RCTs of LIA vs LIA + QLB and LIA vs LIA + PENG powered for clinical significance (pain AUC and opioid thresholds).
- Standardized functional endpoints (e.g., timed mobilization, discharge readiness) and fall risk.
- Surgical approach–specific analyses (anterior vs posterolateral) and dose/volume optimization for each block.
- Cost-effectiveness and workflow impact (block room vs OR time).
- High-risk cohorts (opioid-tolerant, OSA, frailty) for tailored strategies.
Clinical implications
For routine primary THA with robust multimodal care, make periarticular LIA your default—it most reliably lowers day-1 pain burden and supports recovery without motor impairment. When opioid minimization is crucial (PONV history, OSA, high opioid risk), consider adding a QLB; it offers the strongest signal for reducing opioid needs at 24 h. When early functional milestones (standing, transfers, walking at 24 h) are the priority, PENG is a reasonable adjunct, particularly when surgical infiltration quality may vary. In high-pain-risk scenarios (posterolateral approach, complex revisions, opioid tolerance), stacking LIA with QLB or PENG can deliver incremental benefit—balancing gains against extra time, LA dose, and resource use. Reserve ESPB for patients where PONV reduction carries outsized value, recognizing its less consistent analgesic performance. Build these choices into a decision pathway that accounts for surgical approach, patient risk, and team skill set.
Clinical pearls
- LIA most consistent for 0–24 h pain AUC.
- QLB best signal for 24-h opioid reduction.
- PENG often strongest for 24-h function.
- ESPB useful for PONV control, weaker for core analgesia.
- LIA + QLB/PENG may outperform LIA alone in select patients.
Practical tip: Start with LIA for all THA; add QLB for opioid-sparing or add PENG when 24-h function is the top goal.
For more detailed information, refer to the full article in Anesthesiology.
Hussain N. et al. Analgesic Benefits of Motor-sparing Fascial Plane Blocks in Comparison to Periarticular Local Infiltration Analgesia for Total Hip Arthroplasty: A Network Meta-analysis. Anesthesiology. 2025;143:604-624.
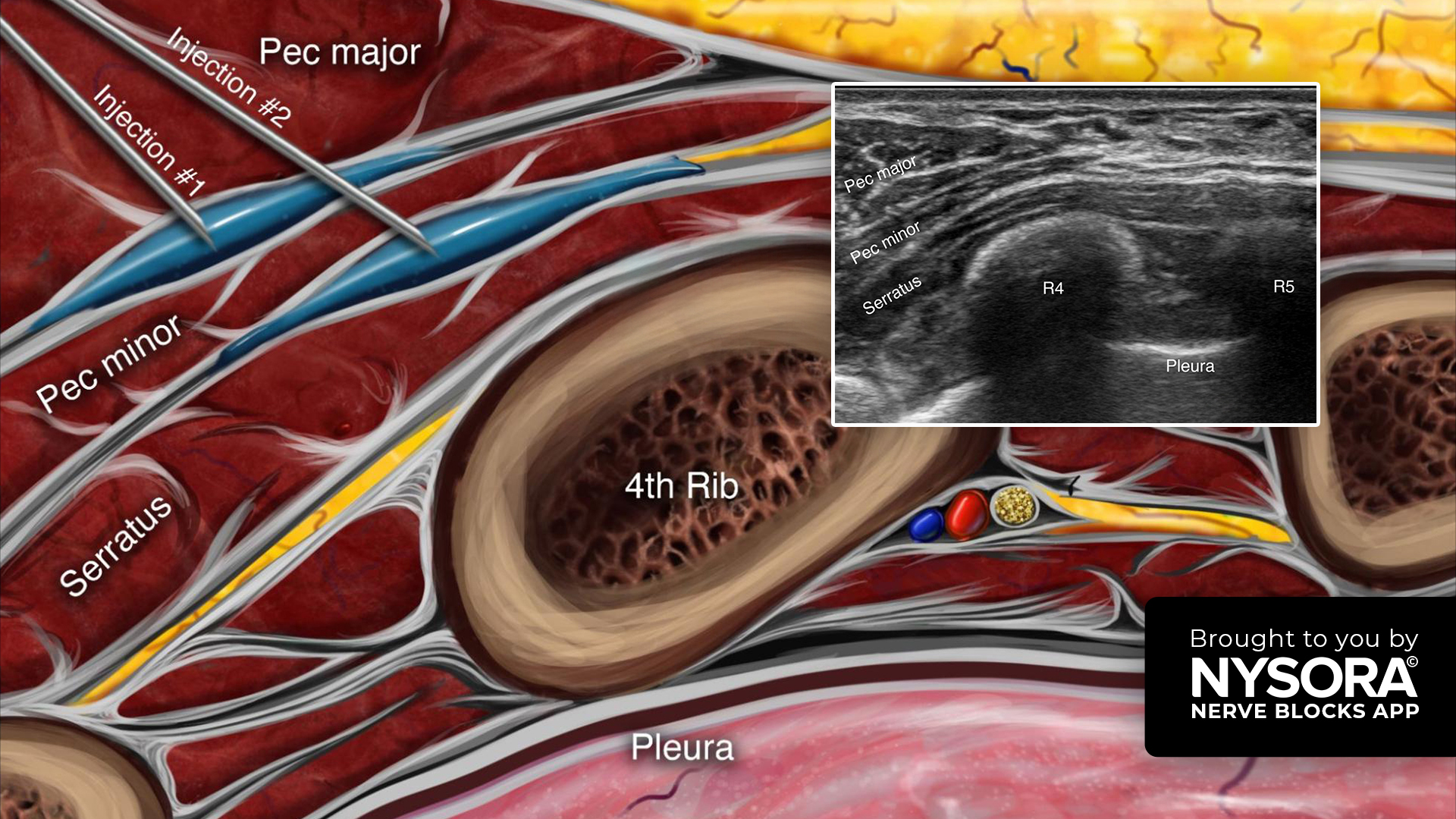
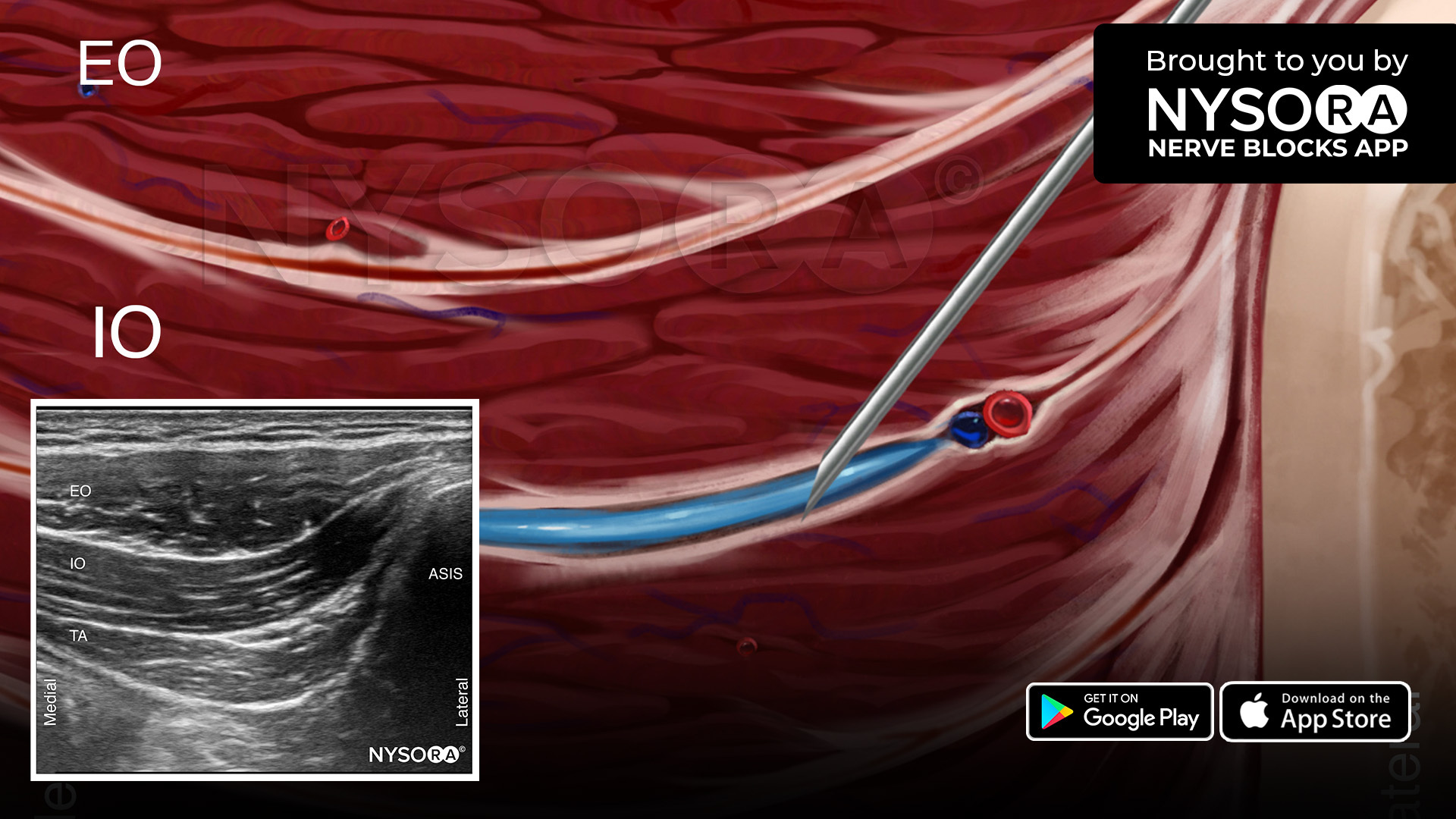
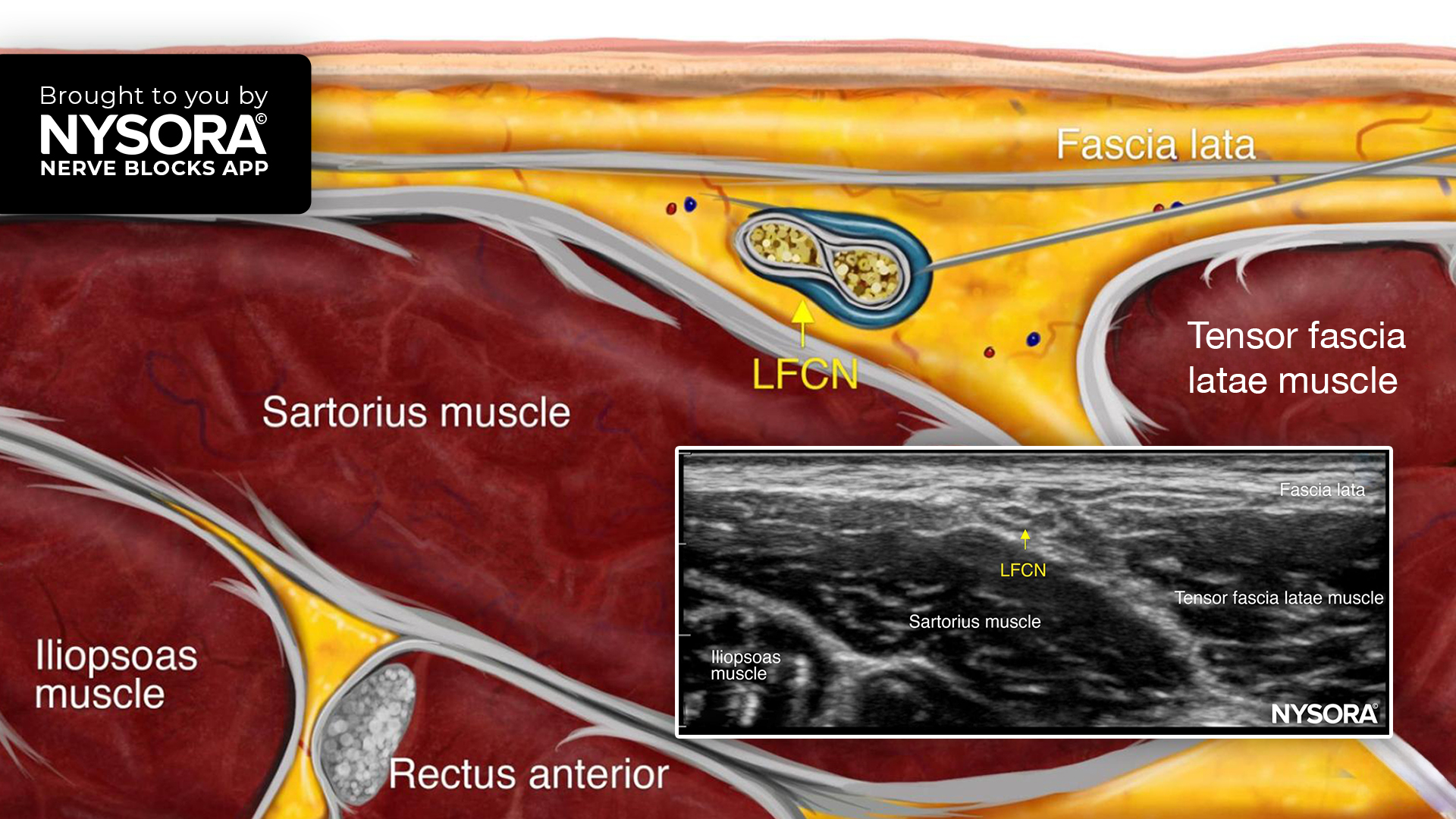
Master PENG and QLB techniques step-by-step with structured guides in the NYSORA Nerve Blocks App.