Chronic lower back pain (CLBP) remains a prevalent and often debilitating condition impacting millions globally. Despite multiple treatment options, many patients continue to struggle with persistent pain, reduced functionality, and heavy reliance on opioids. Lumbar facet joint arthropathy, a major contributor to CLBP, has seen promising therapeutic interventions with radiofrequency ablation (RFA). However, until recently, the optimal temperature for achieving sustained relief with RFA has remained unclear.
A new randomized, double-blinded clinical trial led by researchers at the Cleveland Clinic sheds vital light on this issue. By comparing outcomes of RFA performed at 80°C versus 90°C, the study offers compelling evidence that higher temperatures deliver longer-lasting pain relief without additional risks. This discovery could influence the future of spinal interventional medicine.
What is lumbar facetogenic back pain?
Lumbar facetogenic pain arises from the facet joints, which are small stabilizing joints in the back of the spine. These joints can degenerate over time or due to injury, leading to inflammation, joint dysfunction, and pain. The condition is:
- Common in adults over 50
- Associated with prolonged standing or spinal extension
Frequently localized without radiating to the leg
Understanding radiofrequency ablation (RFA)
RFA is a minimally invasive outpatient procedure targeting pain-carrying nerves. Under fluoroscopic guidance, a radiofrequency probe is inserted to apply controlled thermal energy to the medial branch nerves, disrupting their ability to transmit pain signals.
Key goals of RFA:
- Reduce pain intensity
- Improve mobility and function
- Minimize the need for opioids
Historically, temperatures for RFA have varied between 70°C and 90°C, with no consensus on the most effective setting. This study fills a critical knowledge gap by directly comparing outcomes at 80°C and 90°C.
Study methodology and patient profile
The trial enrolled 144 patients with unilateral CLBP due to confirmed lumbar facet joint arthropathy.
Inclusion criteria:
- Adults aged 18 and older
- Pain >6 months duration
- Positive response to two diagnostic medial branch blocks (≥75% pain relief)
- Failed conservative therapy (e.g., medications, physical therapy)
Exclusion criteria:
- Bilateral back pain or radiculopathy
- Prior surgery at treated levels
- BMI >35 kg/m²
- Active infections or bleeding disorder
Study design highlights:
- Double-blinded: Neither the patient nor the physician knew the temperature used
- Randomization: Equal allocation to 80°C and 90°C RFA groups
- Uniform protocol: Standardized needle type (20G, 10 mm), duration (90 seconds), and approach
Outcome measures
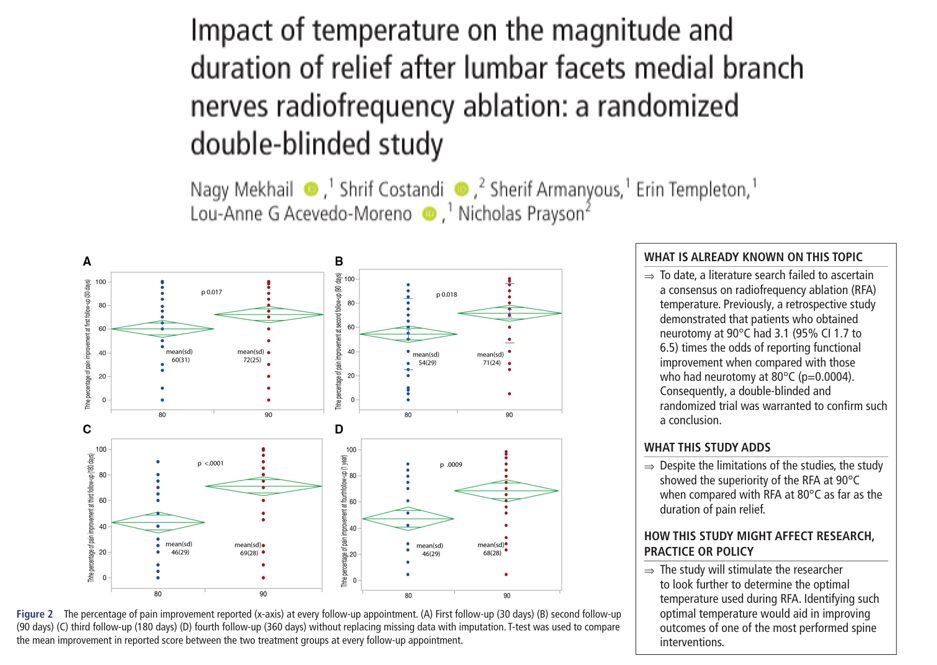
The researchers assessed outcomes at 1, 3, 6, and 12 months post-procedure using:
- Visual Analog Scale (VAS) for pain
- Pain Disability Index (PDI)
- Beck Depression Inventory (BDI)
- Patient satisfaction scores
- Opioid consumption
- Time to repeat RFA
Key results and interpretation
1. Pain relief
Both groups experienced significant reductions in VAS scores. However, the 90°C group demonstrated:
- Greater reduction in pain at 3, 6, and 12 months
- Median VAS change at 6 months: 25% (90°C) vs. 14% (80°C)
2. Duration of relief
The standout finding was the longer median duration before needing repeat RFA:
- 217 days (90°C)
- 112 days (80°C)
- Statistically significant (p<0.04)
3. Functional improvement
Self-reported function was significantly better at all follow-ups in the 90°C group:
- At 6 months: 72% (90°C) vs. 45% (80°C)
- Improved patient satisfaction: 90% at 12 months vs. 55% (p=0.007)
4. Opioid use and mood impact
Both groups reduced opioid usage with no significant differences. Depression scores remained stable.
5. Safety and adverse events
- No serious complications
- Numbness was more common in the 80°C group (23% vs. 7%, p=0.007)
- Temporary site discomfort in 36% of patients overall
Scientific rationale for temperature differences
Why does 90°C offer better outcomes? Higher temperatures yield:
- Larger lesions: More likely to capture all nerve branches
- Increased energy transmission: Greater nerve disruption
However, exceeding 90°C may cause tissue charring, increasing impedance, and limiting lesion size. Therefore, 90°C appears to be the upper effective threshold without risking complications like burns or nerve injury.
6 steps for lumbar medial branch RFA
- Initial evaluation: History, physical exam, and diagnostic imaging
- Diagnostic medial branch block: Two blocks confirming >75% relief
- Determine eligibility: Exclude bilateral pain, prior surgery, or contraindications
- Schedule the procedure: Typically outpatient with mild sedation
- Ablation:
- Fluoroscopic needle guidance
- Targeted nerve heating for 90 seconds
- Follow-up: Monitor pain, function, and any need for repeat RFA
What does this mean for patients and providers?
For patients:
- More informed choices about their RFA treatment
- Higher chances of longer relief without added risks
For pain specialists:
- Potential guideline updates recommending 90°C as the standard
- Reinforces the importance of procedural precision and temperature setting
For policymakers and insurers:
- Justification for supporting the slightly more resource-intensive 90°C RFA
- Potential for improved outcomes and reduced repeat procedures
Final thoughts
This trial adds a crucial piece to the evolving puzzle of interventional pain management. RFA has long been a cornerstone therapy for lumbar facet-mediated pain, but this study highlights how even minor adjustments, like increasing the ablation temperature, can have significant clinical implications.
Key takeaway: While 80°C and 90°C RFA both provide meaningful relief, 90°C offers superior, longer-lasting benefits without additional safety concerns.
For more information, refer to the full article in RAPM.
Mekhail N, Costandi S, Armanyous S, et alImpact of temperature on the magnitude and duration of relief after lumbar facets medial branch nerves radiofrequency ablation: a randomized double-blinded studyRegional Anesthesia & Pain Medicine 2025;50:331-338.
Read more about the latest impactful research in pain medicine in Pain Medicine Updates 2025!