Learning objectives
- Describe Sjogren’s syndrome
- Recognize the symptoms and signs of Sjogren’s syndrome
- Anesthetic management of a patient with Sjogren’s syndrome
Definition and mechanisms
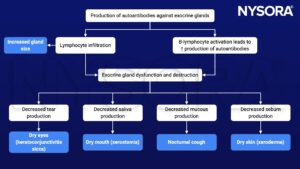
- Sjogren’s syndrome is a frequent autoimmune disease (autosomal recessive disorder) characterized by dysfunction and destruction of exocrine glands (e.g., lacrimal and salivary glands), associated with lymphocytes infiltrates and immunological hyperreactivity
- The hallmark symptoms of Sjogren’s syndrome are dry eyes and a dry mouth
- The condition often accompanies other immune system disorders (e.g., rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis)
Signs and symptoms
- Dry eyes (keratoconjunctivitis sicca)
- Dry mouth (xerostomia)
- Joint pain, swelling, and stiffness
- Swollen salivary glands
- Skin rashes or dry skin (xeroderma)
- Vaginal dryness
- Chronic dry cough
- Prolonged fatigue
- Thyroid problems
Causes
- Genetic factors: Mutations in HLA-DR and HLA-DQ genes
- Environmental factors: Viruses (e.g., Epstein-Barr virus, hepatitis C, and human T-cell leukemia virus type 1), hormones (e.g., estrogen, prolactin), etc.
Complications
- Dental cavities
- Yeast infections
- Vision problems: Light sensitivity, blurred vision, and corneal damage
- Lymphoma
- Inflammation can cause pneumonia, bronchitis, or other problems in the lungs; lead to problems with kidney function; and cause hepatitis or cirrhosis of the liver
- Peripheral neuropathy (numbness, tingling, and burning of the hands and feet)
Risk factors
- Age >40 years
- Female gender
- Rheumatic disease (i.e., rheumatoid arthritis or lupus)
Pathophysiology
Treatment
- Medications
- Decrease eye inflammation (artificial tears): Cyclosporine or lifitegrast
- Increase production of saliva (and sometimes tears): Pilocarpine and cevimeline
- Address specific complications: NSAIDs or other arthritis medications, antifungal medications for yeast infections
- Surgery to seal the nasolacrimal ducts that drain tears from the eyes
Management
Preoperative management
- Complete medical history: Evolution and symptomatology of the disease
- Thorough physical examination
- Continue chronic therapy until the morning of surgery
Intraoperative management
- Goal: Humidify the mucous membranes rigorously during the anesthetic procedure
- Lubricate the eyes to prevent corneal damage
- Avoid respiratory dryness by using humidified oxygen
- Suction efficiently to prevent mucous plugs
- Avoid parasympatholytic and anticholinergic drugs due to their decrease in gland secretions
Postoperative management
- No increased risk for postoperative complications
Suggested reading
- Sjögren Syndrome. In: Bissonnette B, Luginbuehl I, Marciniak B, Dalens BJ. eds. Syndromes: Rapid Recognition and Perioperative Implications. McGraw Hill; 2006. Accessed February 20, 2023. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=852§ionid=49518220
We would love to hear from you. If you should detect any errors, email us [email protected]








