Learning objectives
- Describe the physiological changes associated with aging
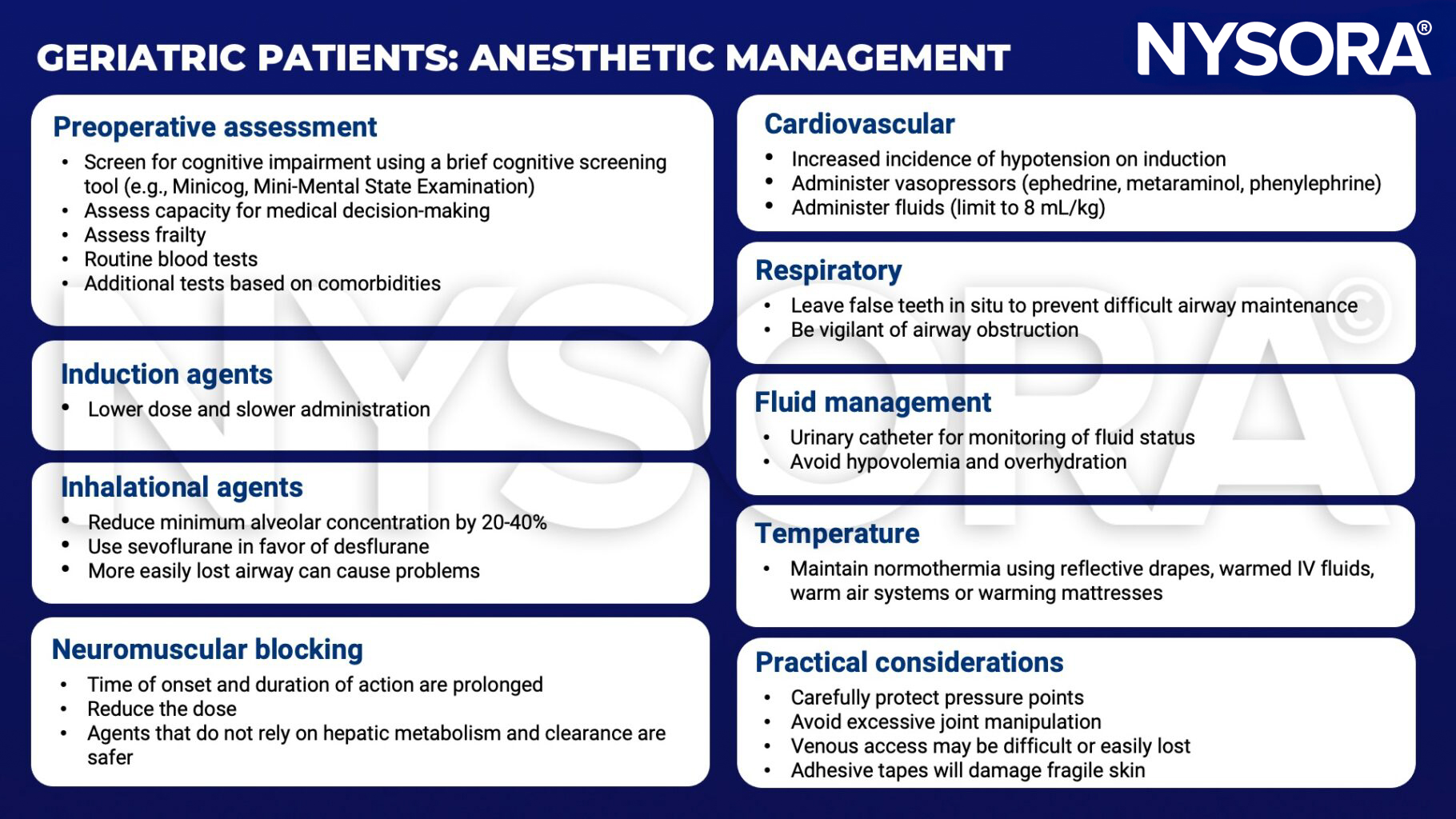
- Manage geriatric patients presenting for surgery
Background
- Geriatric patients often present with conditions requiring surgery
- Age increases perioperative risks associated with anesthesia
- Geriatric patients have a greater risk of perioperative morbidity and mortality
Physiological changes

Common surgeries in the elderly
- Cataract surgery
- Trans-urethral resection of the prostate
- Hip fracture surgery
- Knee arthroplasty
- Cholecystectomy
- Pacemaker implantation
- Colorectal excision
- Breast excision
Management
Suggested reading
- Staheli B, Rondeau B. Anesthetic Considerations In The Geriatric Population. [Updated 2022 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572137/
- Murray D, Dodds C. Perioperative care of the elderly. Continuing Education in Anaesthesia Critical Care & Pain. 2004;4(6):193-6.
Clinical updates
Loggers et al. (JAMA Surgery, 2022) report from the FRAIL-HIP study that in severely frail, institutionalized adults ≥ 70 years with proximal femoral fractures, nonoperative management was noninferior to surgery for health-related quality of life, despite markedly higher short-term mortality. Nonoperative care was associated with fewer adverse events and high proxy-rated satisfaction, supporting shared decision-making and comfort-focused, palliative approaches when life expectancy is limited.
The 2024 European Society of Anaesthesiology and Intensive Care (ESAIC) guidelines emphasize that postoperative delirium is a common and preventable complication in older adults, recommending mandatory preoperative risk screening for patients ≥ 60 years. The guidelines strongly support multicomponent nonpharmacological prevention bundles (reorientation, sleep hygiene, early mobilization) and advise against routine use of antipsychotics, with dexmedetomidine reserved for selected high-risk patients.
Ardeshiri et al. (Regional Anesthesia & Pain Medicine, 2025) show that restorative neurostimulation for chronic mechanical low back pain provides durable benefit in older adults, with 62% achieving ≥ 50% pain reduction and meaningful improvements in disability and quality of life at 2 years. Outcomes in patients up to 82 years were comparable to those of younger cohorts, with marked gains in mobility and function.
- Read more about this study HERE.









