Learning objectives
- Describe Cushing’s syndrome
- Recognize the symptoms and signs of Cushing’s syndrome
- Anesthetic management of a patient with Cushing’s syndrome
Definition and mechanisms
- Cushing’s syndrome is a collection of signs and symptoms due to prolonged exposure to glucocorticoids (i.e., cortisol)
- Cushing’s disease is a specific type of Cushing’s syndrome caused by a pituitary tumor leading to excessive production of adrenocorticotropic hormone (ACTH) → excessive ACTH stimulates the adrenal cortex to produce high levels of cortisol
Causes
Exogenous
- Patients taking prescribed glucocorticoids (e.g., prednisone) to treat other diseases (i.e., asthma and rheumatoid arthritis) or for immunosuppression after organ transplants = iatrogenic Cushing’s syndrome
- Adrenal glands may gradually atrophy due to lack of stimulation by ACTH, which’s production is reduced by the glucocorticoid medication
- Resolves when the patient stops the glucocorticoid medication
Endogenous
- Derangement of the body’s system to secrete cortisol
- Hormone-secreting tumors of the adrenal glands or pituitary
- Pituitary Cushing’s: Benign pituitary adenoma secretes ACTH = Cushing’s disease
- Adrenal Cushing’s: Excess cortisol production by adrenal glands tumors, hyperplastic adrenal glands, or adrenal glands with nodular adrenal hyperplasia
- Tumors (e.g., small cell lung cancer) outside the pituitary-adrenal system can also produce ACTH = ectopic or paraneoplastic Cushing’s disease
Signs and symptoms
- Moon face
- Central obesity with buffalo hump
- Thin skin that bruises easily
- Purple striae on the abdomen and thighs
- Proximal muscle wasting
- Thin extremities
- Osteoporosis
- Hypertension
- Left ventricular hypertrophy
- Hyperglycemia
- Impaired glucose tolerance and diabetes mellitus type II
- Metabolic alkalosis
- Hypokalemia
- Poor wound healing
- Menstrual irregularities
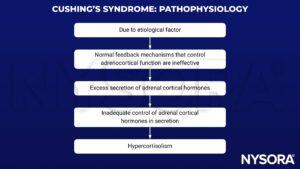
Pathophysiology
Treatment
- Transsphenoidal microadenomectomy and radiotherapy for pituitary-dependent Cushing’s disease
- Adrenal adenoma or carcinoma requires surgical removal of the affected gland
- Hypercortisolism can be controlled with adrenal enzyme inhibitors, such as ketoconazole, metyrapone, mitotane, or aminoglutethimide, given alone or in combination → drugs to inhibit release and synthesis of glucocorticoids
Management
Preoperative considerations
- Patients with Cushing’s syndrome are classified as ASA 2 or 3
- Airway evaluation: Mallampati score, mouth opening, neck extension, tireomental and sternomental distances, and Wilson score
- Careful cardiovascular evaluation: ECG, echo
- Careful respiratory evaluation: X-ray, blood gases, PFT
- Stabilize glycemia: Stop oral therapy and start insulin regimen
| Regular insulin | Type 1 DM (male) | Type 1 DM (female) | Type 2 DM |
|---|---|---|---|
| Initial bolus infusion | 0.05-0.1 U/kg 1 U/h | 0.05-0.1 U/kg 0.5 U/h | 0.05-0.1 U/kg 1 U/h |
- Correct acid-base and electrolytes imbalances: Spironolactone, potassium
- Continue antihypertensive drugs until the morning of surgery except for the angiotensin-converting enzyme inhibitors (i.e., captopril, enalapril, lisinopril, enalaprilat, and ramipril) and angiotensin II receptor blocks (i.e., valsartan)
- Discontinue clopidogrel 5-7 days before surgery, except in coronary-stent patients (risk of stent occlusion)
- Continue glucocorticoid inhibitors (i.e., ketoconazole, metyrapone, mitotane, or aminoglutethimide)
- Prevent perioperative venous thromboembolism and pulmonary embolism: LMWH (i.e., enoxaparin, dalteparin) or fondaparinux
- Avoid deep preoperative sedation → Premedication drugs: Midazolam 1 mg i.v.
Intraoperative considerations
- Positioning and taping: Careful and gentle positioning to avoid fractures
- Standard monitoring: Non-invasive blood pressure, temperature, end-tidal carbon dioxide, pulse oximetry, and ECG
- Invasive monitoring: Invasive blood pressure via arterial catheter cannulation and Swan-Ganz pulmonary artery catheter (if necessary)
- Venous access: Large bore peripheral and central venous catheters
- Maintain the glucose blood level within normal values (i.e., 120-180 mg/dL) → insulin regimen
| Glucose blood level (mg/dL) | Infusion rate change (U/h) |
|---|---|
| ≤70 | Reassessment within 30 min |
| 70-120 | ↓ 0.3 |
| 121-180 | No change |
| 181-240 | ↑ 0.3 |
| 241-300 | ↑ 0.6 |
| ≥300 | ↑ 1 |
- Prevent gastric aspiration: Metoclopramide 10 mg, ranitidine 50 mg i.v., and sodium citrate 30 mL P.O.
- Induction of anesthesia and endotracheal intubation: Rapid induction sequence
- Blunt sympathetic response (i.e., hypertension and arrhythmias) during induction: Opioids, lidocaine, clonidine, and esmolol
- Avoid ketamine because of its sympathetic effects
- Extubate if the patient is alert, warm, hemodynamically stable, and fully reversed from muscle relaxants
Postoperative considerations
- Prevent respiratory complications (i.e., atelectasis, hypoxemia): Effective postoperative pain relief, early mobilization, and respiratory exercises
- Postoperative acute pain treatment: Systemic analgesic drugs (i.e., patient-controlled analgesia pumps or epidural analgesia)
- Routinely check cortisol, glucose, and electrolytes blood levels
- Continue replacement of cortisol, guided by cortisol blood levels
- Use insulin regimen to maintain the glucose blood level within recommended levels
- Continue antihypertensive drugs based on the patient’s hemodynamic status
Keep in mind
- The anesthesiologist has to deal with difficult ventilation and intubation, hemodynamic disturbances, volume overload and hypokalemia, glucose intolerance, and diabetes, maintain the blood cortisol level, and prevent glucocorticoid deficiency in the perioperative period
Suggested reading
- Melanie Davies, FRCA, Jonathan Hardman, DM FRCA, Anaesthesia and adrenocortical disease, Continuing Education in Anaesthesia Critical Care & Pain, Volume 5, Issue 4, August 2005, Pages 122–126, https://doi.org/10.1093/bjaceaccp/mki033
- Domi R, Sula H, Kaci M, Paparisto S, Bodeci A, Xhemali A. Anesthetic considerations on adrenal gland surgery. J Clin Med Res. 2015;7(1):1-7.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com