Learning objectives
- Describe the difference between omphalocele and gastroschisis
- Anesthetic management of pediatric patients with abdominal wall defects
Definition and mechanisms
- Omphalocele and gastroschisis are congenital abdominal wall defects resulting in intestinal herniation from the abdominal cavity
- Resulting from major defects in the closure of the abdominal wall → exposure of abdominal viscera
- Main difference: There is no sac covering the intestines in gastroschisis
- Both can be detected antenatally using fetal ultrasound → allows timing, location, and mode of delivery to be planned in advance
- Omphalocele: Deliver at term
- Gastroschisis: Benefit from early delivery (37 weeks gestation) to limit bowel damage from exposure to amniotic fluid
- Both are associated with prematurity and low birth weight
Omphalocele
- Herniation of abdominal contents through the middle of the abdominal wall at the umbilicus
- The skin, muscle, and fibrous tissue are missing
- The intestines herniate through the opening and are covered by a thin sac
- The sac is formed from an outpouching of the peritoneum and protrudes in the midline, through the umbilicus
- Commonly occurs with other congenital defects (e.g., heart and kidney defects), chromosome abnormalities (e.g., Down syndrome, trisomy 18, trisomy 13), and genetic syndromes (e.g., Beckwith-Wiedemann syndrome)
Gastroschisis
- Herniation of abdominal contents from a defect lateral to the umbilicus (usually right-sided), but not directly over it
- Protruding organs are not covered by a thin sac → damage due to direct contact with amniotic fluid in the uterus → inflammation
- Rarely have other congenital defects, seldom associated with chromosome abnormalities or genetic syndromes
Signs and symptoms
- External herniation of abdominal viscera
Omphalocele
- Omphalocele minor: Minor herniation into the umbilical cord, small 5-8 cm defect
- Omphalocele major: Large defect, including the liver, with poorly developed abdominal and pulmonary hypoplasia
- Intestine looks normal
Gastroschisis
- The intestine wall may be thickened, with a fibrin “peel” due to exposure to amniotic fluid
- May involve the stomach, bladder, uterus, and rarely liver
Complications
- Intrauterine growth retardation
- Underdevelopment of the lungs → respiratory insufficiency may require mechanical ventilation
- Feeding difficulties
- Poor gut motility
- Malrotation
- Intestinal atresia
- Volvulus
- Stenosis
- Gastroesophageal reflux
- Short bowel syndrome → dehydration
Sequelae of an open abdomen
- Aspiration
- Hypothermia
- Fluid and electrolyte abnormalities
- Sepsis
Treatment
Initial post-delivery treatment
- Fluid resuscitation
- Care of herniated bowel/viscera and their blood supply: Cover exposed organs with a sterile dressing to keep them moist and protected
- Bowel decompression using a nasogastric tube
- Temperature regulation: Nurse in an incubator to reduce heat loss
- Omphalocele: Inspect the sac to check whether or not it is ruptured
- IV antibiotics to minimize the risk of infection
Single vs staged surgery
- Surgery typically takes place shortly after birth
- Omphalocele: Semi-urgent surgery unless sac is ruptured
- Gastroschisis: Urgent surgery
- Required to replace the intestines in the abdomen and to close the opening
- Single stage surgery: Omphalocele minor
- Intestines are moved back in the abdomen, and the opening is closed during the same surgery
- Staged surgery: Omphalocele major and gastroschisis
- Wrap intestines in a protective covering (i.e., silo)
- Gradually move intestines back into the abdomen over several days or weeks
- Surgically close the opening once all intestines are back in the abdomen
Management
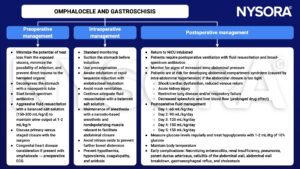
Keep in mind
- Neonates are highly susceptible to dehydration and heat loss before repair of the abdominal wall defect → fluid resuscitation and temperature control
- Repair surgery may be primary or staged
- Improved survival is associated with optimal pre- and postoperative care
Suggested reading
- Saraiya NR. GASTROSCHISIS AND OMPHALOCELE. In: Houck PJ, Haché M, Sun LS. eds. Handbook of Pediatric Anesthesia. McGraw Hill; 2015. Accessed February 14, 2023. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=1189§ionid=70363342
- Poddar R, Hartley L. Exomphalos and gastroschisis. Continuing Education in Anaesthesia Critical Care & Pain. 2009;9(2):48-51.
- Wouters K, Walker I. Neonatal anaesthesia 2: Anaesthesia for neonates with abdominal wall defects. WFSA. August 28, 2008. Accessed February 14, 2023. https://resources.wfsahq.org/atotw/neonatal-anaesthesia-2-anaesthesia-for-neonates-with-abdominal-wall-defects/
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com