Learning objectives
- Recognize sings & symptoms of BrS
- Diagnose BrS
- Manage patients with BrS
Definition & mechanisms
- Brugada syndrome (BrS) is an abnormality of cardiac ion channels that increases the risk of ventricular fibrillation and sudden cardiac death
- Linked to 19 genetic mutations that encode for sodium, calcium, or potassium channels and result in either increase or decrease in their activity
- In up to 80% of patients, no causative genetic mutation can be found
- Thought to be responsible for up to 40% of sudden cardiac death cases in a structurally normal heart
Signs & symptoms
- Palpitations
- Chest discomfort
- Syncope and nocturnal agonal respiration
- Monomorphic ventricular tachycardia is rare but is more often seen in infants and children
- Events typically occur during sleep with increased vagal tone, with fever, or can be precipitated by drugs, alcohol, and electrolyte disorders
- Between 20 and 30% of patients: supraventricular tachycardias (atrial flutter, atrioventricular nodal re-entry, Wolff-Parkinson-White syndrome), atrial fibrillation is seen most frequently
- In critical care, the most common presentation will be a patient with aborted sudden cardiac death
- Many patients remain asymptomatic
Diagnosis
Diagnosis is based on fulfilling the BrS ECG morphological criteria:
- Type 1: A cove shaped (with T-wave inversion) ST-segment elevation 2 mm in V1 and/or V2 when placed in a standard or superior position, either spontaneously or after Na-channel blocking agent administration (e.g., ajmaline/flecainide)
- Additional ECG morphologies:
- Type 2: Saddleback-shaped (with positive T-wave) ST-segment 1 mm in V1 and/or V2
- Type 3: Saddleback or cove-shaped ST-segment elevation <1 mm in V1 and/or V2
- Neither are diagnostic
- The ECG morphology can change with time and an individual with true BrS can manifest all three different morphologies at different times
- Many conditions can reproduce a type 1 Brugada ECG, differential diagnosis:
- Early repolarisation
- Athlete’s heart
- Acute coronary events
- Pulmonary embolism
- Electrolyte disturbance
- Pericarditis
- Myocarditis
- Dissecting aortic aneurysm
- Arrhythmogenic right ventricular cardiomyopathy
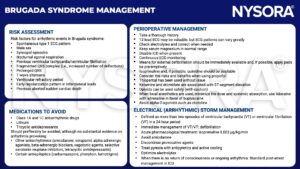
Management
Suggested reading
- Levy D, Bigham C, Tomlinson D. Anaesthesia for patients with hereditary arrhythmias part I: Brugada syndrome. BJA Educ. 2018;18(6):159-165.
We would love to hear from you. If you should detect any errors, email us at customerservice@nysora.com